CHAPTER 26 Arthrofibrosis
Some degree of shoulder stiffness is very common in clinical practice. Stiffness may or may not be the primary complaint of the patient. Weakness, pain, or even (paradoxically) a feeling of instability may have brought the patient to see the physician. Stiffness can be the primary problem, as in the case of chronic adhesive capsulitis, or may be secondary to other conditions such as trauma, rotator cuff disease, or arthritis. In our evaluation of patients with rotator cuff tears, 30 of 72 had a motion deficit of 20 degrees or more.1 It is particularly important to use the term idiopathic adhesive capsulitis only for that specific pathologic condition and not as a description of shoulder stiffness in general. Stiffness of the shoulder may be truly mechanical and attributable to a specific anatomic abnormality, or can be nonanatomic and caused by guarding because of pain or secondary gain issues. In this chapter, we will outline the various anatomic causes of shoulder stiffness and provide a guide for clinical diagnosis and treatment.
ANATOMY, PATHOANATOMY, AND ETIOLOGY
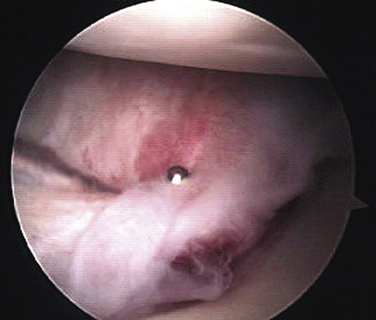
Adhesive Capsulitis
Adhesive capsulitis can be idiopathic, related to diabetes, or associated with other pathology about the shoulder. There is no standard agreement as to what range-of-motion (ROM) loss constitutes adhesive capsulitis.2 The classic, severely inflamed, thickened, and contracted capsule is pathgnomonic (Fig. 26-1). Fibroblast proliferation and smooth muscle phenotypic transformation has been found in the capsular tissue of some patients with adhesive capsulitis, similar to Dupuytren’s contracture in the hand.3 Diabetes is commonly associated with adhesive capsulitis.1,4,5 Any pathologic condition that causes primary or referred pain to the shoulder can potentially initiate an inflammatory cascade leading to adhesive capsulitis. Whereas adhesive capsulitis occurs in patients with rotator cuff disease, no relationship to acromial morphology has been found.6 Harryman has compiled an extensive list of possible pathogenic mechanisms but little scientific evidence exists to support any particular entity.7
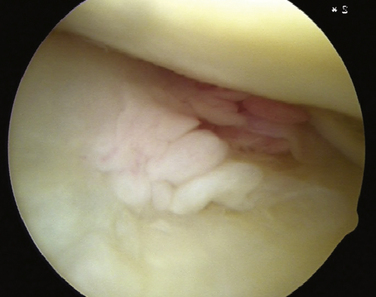
Milder Secondary Mechanical and/or Capsular Contractures
Some patients exhibit lesser degrees of shoulder stiffness compared with adhesive capsulitis. The capsule in these cases will typically have inflammatory changes or the synovium may be inflamed, but to a much lesser extent than in adhesive capsulitis (Fig. 26-2). Many patients with rotator cuff tears have mild stiffness before surgery. Patients with mild or moderate stiffness before surgery tend to have persistent stiffness after surgery but the prognosis for ultimate recovery of almost full motion is very good. Only those patients who have frank adhesive capsulitis at the time of surgery are unlikely to recover satisfactory ROM after surgery.1,8
Focal Capsular Contracture
Throwing athletes and other patients exposed to chronic repetitive throwing injuries are known to develop focal capsular contractures. Glenohumeral internal rotation deficit (GIRD) is a contracture of the posterior inferior shoulder capsule resulting in a loss of internal rotation in the abducted shoulder. GIRD is often associated with SLAP (superior labrum anteroposterior) lesions and partial rotator cuff tears.9
Acute Trauma
Shoulder stiffness following trauma can be caused by soft tissue scarring or fracture malalignment. Patients older than 40 years who suffer a traumatic anterior shoulder dislocation are more prone to the development of stiffness, including adhesive capsulitis, than younger patients.10 For patients with a displaced proximal humerus fracture, there is wide variation in the incidence of stiffness in the published literature, with some studies reporting overall 50% ROM loss for all forms of treatment, including nonoperative, open reduction internal fixation, and hemiarthroplasty.11 Reports of hemiarthroplasty for three- and four-part proximal humeral fractures differ, with some favorable12 and others showing disappointing results.13 A review of older patients with three-part fractures of the proximal humerous treated nonoperatively reported that only 4 of 15 patients had residual pain. However, these patients had significant residual stiffness, with mean flexion and abduction less than 100 degrees.14 Even isolated greater tuberosity fractures of the shoulder have been shown to cause residual pain and stiffness if displaced 3 mm or more. ROM is typically better with surgical intervention.15,16 Recently, success has been reported in the arthroscopic reduction and treatment of greater tuberosity fractures.17,18
Postsurgical Stiffness
Hematoma and secondary fibrosis or overtightening of the shoulder capsule or repaired rotator cuff structures may result in a restriction of motion. Incomplete reduction of fracture fragments after surgical repair can cause mechanical blocks to motion. One review of open rotator cuff repairs has reported a 4% incidence of significant postoperative adhesions. Although arthroscopic or open release was found to be effective, closed manipulation was not.19 Diabetic patients may be more prone to stiffness after rotator cuff repair.20 Long- term follow-up of patients who have undergone open instability repairs has shown a high incidence of osteoarthritis (40% to 60%). At least 30% of these patients have significant loss of motion.21–23 For shoulder replacement surgery, the most common reported cause of failure is stiffness.24 Arthroscopic Bankart repair is associated with very small ROM deficits, generally less than 5 degrees.25,26 However, rotator interval closure has been shown to reduce flexion, external rotation, and anterior translation of the adducted shoulder significantly.27 Thermal capsular shrinkage for multidirectional instability may also cause significant stiffness in some patients.28 Open surgical procedures in proximity to the shoulder can also cause loss of motion, including breast surgery29 and cardiac surgery.30
HISTORY AND PHYSICAL EXAMINATION OF THE STIFF SHOULDER
Physical Examination
The examination should include an evaluation of posture, muscular atrophy, areas of tenderness, active and passive ROM limits, and strength. Tests for subacromial impingement and scapular dyskinesia are performed. The cervical spine is examined for tenderness, loss of motion, and trigger points. An assessment of the neurovascular status of the upper extremities is made. The examiner should avoid painful tests or placing the shoulder in painful positions until the end of the examination to minimize guarding during ROM evaluation. The physical examination checklist is summarized in Box 26-1.
Box 26-1 Physical Examination Checklist
RANGE OF MOTION
The direction of ROM loss and the position of the shoulder point to the location of the contracted tissues. For example, patients with GIRD will primarily display loss of internal rotation with the arm abducted, but usually not with the arm adducted.31,32 Injection of 1% lidocaine into specific regions can help determine the pathoanatomy that is generating the pain and also helps reduce guarding so that the true ROM deficit can be determined. If subacromial injection results in pain relief and improved mobility, the likely cause of the patient’s problem is rotator cuff tendinitis and appropriate treatment is instituted. If pain and stiffness persist despite subacromial injection, an intra-articular injection is given. If pain is relieved but stiffness persists, the patient most likely has adhesive capsulitis. Box 26-2 summarizes the typical history and physical findings by diagnosis.
TREATMENT
Indications and Contraindications
In general, patients with chronic stiffness should have conservative treatment first. Any decision for surgery needs to be made based not only on the diagnosis, but on the patient’s age, medical condition, and premorbid activity level. Surgical indications and contraindications are summarized in Box 26-3. Each surgical indication assumes a failure of conservative treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree