Ankle fractures
INTRODUCTION
The current trend of an increasingly aging population associated with a more active lifestyle is changing the epidemiology of fractures, as well as altering healthcare costs and medical and surgical treatment strategies. The problems related to osteoporosis have become one of the priorities in most healthcare systems and considerable efforts have been made to reduce the financial burden associated with this ever-growing subgroup of patients. However, despite these efforts orthopaedic surgeons are faced with an epidemic of fragility fractures in a group of patients who wish to get back to their pre-injury level of activity as soon as possible. Both the equipment manufacturing industry and orthopaedic researchers have addressed this expanding market in an attempt to solve the problems of reduction and fixation of osteoporotic fractures. To complicate things further, patients with fragility fractures have poorer soft tissues and an increased prevalence of associated medical comorbidities that put them at risk of developing complications. They also have a lower physiological reserve making early mobilization more challenging.
This chapter reviews ankle fractures in older patients and focuses on the changing epidemiology, treatment strategies and surgical options when traditional treatment methods fail. We also review common complications as well as solutions that can be utilized to treat these fractures and prevent their occurrence.
EPIDEMIOLOGY
The age at which ankle fractures are defined as occurring in elderly patients varies, but it has tended to increase in more recent studies. Beauchamp et al.1 defined it as 50 years in 1983, but Vioreanu et al.2 defined it as 70 years in 2007. Many surgeons accept an age of ≥65 years as defining an elderly patient and ≥80 years as defining a super-elderly patient. However, we believe that it is important to consider the patients’ physiological age as opposed to their chronological age, as patients’ comorbidities often dictate treatment. We believe that strict reliance on an age range is often of little value.
Ankle fractures are the fourth most common fracture in the ≥65-year-old age group after proximal femoral, distal radial and proximal humeral fractures.3 A review of the data presented in Chapter 1 shows that about 90% of ankle fractures in this group follow a standing fall and that only 3% are high energy injuries. A further 3% present with multiple fractures. In the super-elderly group there are fewer high energy injuries, but over 6% of patients have multiple fractures, confirming the relative frailty of this group. Overall ankle fractures in the ≥65-year-old group have a type IV pattern with a relatively constant incidence of fractures in females aged between 65–69 years and 90+ years, but a declining incidence in males (Chapter 1).
Review of the different fracture types in the series presented in Chapter 1 shows that 25.9% were AO/OTA type A fractures, 67.6% were type B fractures and 6.5% were type C fractures. In the super-elderly group the equivalent figures were 24.1%, 74.4% and 1.3%, indicating the reduction in prevalence of type C supra-syndesmotic fractures with increasing age. There were no type C ankle fractures in females 80 years or older and none in males aged 75 years or older.
Chapter 1 also shows that there is a relatively high incidence of open ankle fractures in females, and in females aged ≥65 years only open fractures of the distal radius and ulna and the finger phalanges had a higher incidence. About 57% of open fractures in females aged ≥65 years were Gustilo and Anderson4 type III in severity. This rose to about 73% in the super-elderly group, confirming increasing patient frailty and the poorer condition of the soft tissues around the ankle in the aging patient.
There is evidence that the incidence of ankle fractures is increasing in the elderly population. Kannus et al.5 looked at the epidemiology of ankle fractures in Finland between 1970 and 2000 and showed that the incidence of low velocity ankle fractures in patients aged ≥60 years was 57/105/year in 1970 and 150/105/year in 2000. In males it rose from 38/105/year to 114/105/year and in females it rose from 66/105/year to 174/105/year. This study only examined in-patients and therefore might have underestimated the incidence of ankle fractures, particularly in 1970 when less surgical treatment would have been undertaken.
An analysis of the equivalent figures in Edinburgh confirms that the incidence of ankle fractures in the elderly is increasing. In 2000 the incidence of ankle fractures in males aged ≥60 years was 83/105/year. This rose to 107/105/year in 2010/2011. The equivalent figures for females were 159/105/year and 213/105/year. In the super-elderly population the incidence of male ankle fractures rose from 55/105/year in 2000 to 99/105/year in 2010/2011. The equivalent figures for the super-elderly female group were 166/105/year and 174/105/year. This suggests that the males were more active and less frail in 2010/2011 than in 2000. It has been shown that smoking, polypharmacy and poor mobility are the factors that best predict ankle fractures in the elderly,6 but it would be reasonable to suggest that as the elderly get fitter and the population ages, ankle fractures will continue to increase in incidence and have a significantly greater impact on society.
CLASSIFICATION
In general, the Lauge-Hansen7 and AO/OTA8 classifications are used to describe the different patterns of ankle fractures, although they are suboptimal for elderly patients as they are less likely to guide treatment than in a younger patient population. In addition, the classic fracture configurations that characterize different fracture subtypes in the Lauge-Hansen classification are not always seen in elderly patients. Poor bone quality and the consequences of lengthy osteoporosis medication can alter the classic fracture patterns that are seen in younger patients. However, there are, as yet, no classifications for ankle fractures in the elderly.
The Lauge-Hansen classification7 is based on the position of the foot at the time of fracture (supination or pronation) and the direction of the deforming force (abduction, adduction, internal or external rotation). This gives four types of injury, these being supination external rotation (SER), pronation external rotation (PER), supination adduction (SA) and pronation abduction (PA). A number is then applied which refers to the progression through the stages of bone and soft tissue injury. The Lauge–Hansen classification is summarized in Table 42.1. The AO/OTA8 classification is derived from the earlier Weber classification and is a morphological classification. Type A fractures occur below the level of the inferior tibio-fibular syndesmotic ligaments. A1 fractures are unifocal lateral lesions. In A2 fractures there is an associated medial malleolar fracture and in A3 fractures there is an associated posteromedial fracture. Type B fractures are trans-syndesmotic fractures. In B1 fractures there is an oblique or spiral distal fibular fracture. In B2 fractures there is an associated medial malleolar fracture and in B3 fractures there is an associated posterior malleolar fracture. Type C fractures are rare in the elderly. These are supra-syndesmotic fractures with C1 fractures having a simple fibular fracture with damage to the anterior tibio-fibular ligaments. In C2 fractures the fibular fracture is multifragmentary and in C3 fractures the fibular fracture is located in the proximal fibula.
In open fractures (Figure 42.1) the Gustilo and Anderson4 classification is universally used, but it is not as predictive of outcome in the elderly as it is in younger patients. This is because of poorer skin quality and the state of the soft tissues. There is often difficulty in skin closure and soft tissue treatment can be a challenge because of the difficulties of surgery and the associated medical comorbidities in these patients. Open fractures in the elderly are discussed further in Chapter 13.
TREATMENT
The goals of treatment for this patient population are early mobilization and return to performing activities of daily living as the same comorbidities that may influence the mode of treatment can decompensate with a prolonged recovery and adversely affect patients’ outcomes from a general health perspective. Regardless of the chosen mode of treatment, the surgeon must emphasize medical optimization during the healing phase. This includes encouraging adequate sun exposure, a healthy diet with adequate protein and calcium intake, avoidance of alcohol and tobacco, and perhaps even arranging follow-up with a primary care physician to direct and encourage the above interventions. Patients must be counselled about the diagnosis and treatment of osteoporosis and when required a DEXA scan should be ordered. Osteoporosis is diagnosed by the presence of a fragility fracture, or if bone mineral density of the spine, hip or wrist is less than 2.5 standard deviations from the reference mean (T score of –2.5 or less). The United States Preventative Services Task Force (USPSTF) provides recommendations for routine screening of women aged 65 years or greater. Additionally, the USPSTF recommends this screening to begin at age 60 in high risk females based on several clinical considerations (body weight <70 kg, smoking, weight loss, family history, alcohol/caffeine use and/or low calcium/vitamin D).9
Table 42.1 Lauge-Hansen classification of ankle fractures
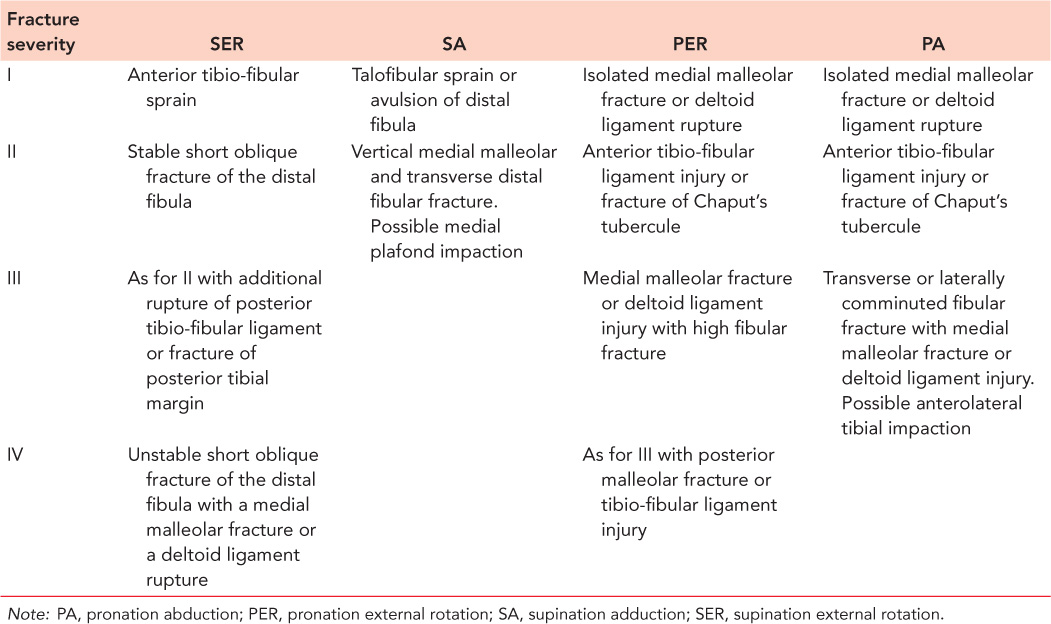
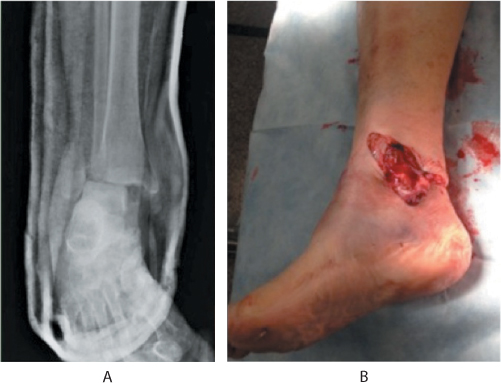
Figure 42.1 A 77-year-old woman who presented with an open Gustilo type II ankle fracture dislocation. (a) Anteroposterior (AP) radiograph of the ankle showing a lateral malleolar fracture. (b) Clinical photograph of the medial open wound exposing the medial malleolus.
NON-OPERATIVE MANAGEMENT
Non-operative management refers to the use of a cast or brace. It is often referred to as ‘conservative’ management due to the avoidance of surgical risk. However, one must appreciate that the use of casts or braces in the elderly population can result in adverse events. Diabetes and patients with frail skin are at risk of developing soft tissue damage, particularly if the cast or brace is poorly applied. Careful attention must be paid to provide extra padding over the bony prominences most at risk of skin damage, these being the medial and lateral malleoli and the heel. The cast should also be reinforced with more casting material in the elderly to avoid damage associated with weight bearing as it is often impractical for elderly patients to remain non-weight bearing.
Casts are often preferred to braces because of the ease of application and moulding. However, it should be remembered that plaster material undergoes an exothermic reaction that can severely burn patients. Lavalette demonstrated that increased plaster thickness, increased water temperature and unintentional insulation caused by placing a pillow beneath the splint during the setting process were all related to the generation of temperatures high enough to cause skin burns.10 This is especially important in elderly patients as their fragile skin and comorbidities place them at increased risk. Halanski et al. recommend using water temperatures lower than 24°C to reduce the risk of thermal injury.11 Splint material should be cut to the appropriate length and folding the splint material should be avoided. The splint should not be allowed to sit on a pillow or to have inadequate ventilation and it should not be over-wrapped with fibreglass casting material until it is completely cooled.11
The use of non-operative management in elderly patients with ankle fractures has changed in the last few decades. Beauchamp et al.1 compared operative and non-operative management in 126 patients over 50 years of age between 1976 and 1979. They stated that operative fixation achieved better reduction, but there was a higher complication rate in females. They stressed that patient satisfaction was very similar. Salai et al.12 stated that non-operatively managed patients had higher AOFAS scores after 3 years and that 33% of patients required hardware removal. They advocated the use of non-operative management if reduction could be maintained in a cast.
More recently Vioreanu et al.2 analysed 40 patients with non-operatively managed ankle fractures. The average age was 78.6 years and 28 (70%) were independent. They reported that 27.5% of the patients subsequently required surgery and 17.2% required re-manipulation. Only 45% of the patients returned to their pre-fracture activity level. They compared the group with a similar cohort of patients that had been managed operatively and recorded that 72% of their patients returned to their pre-accident activity levels.
The recent literature indicates that non-operatively managed displaced ankle fractures in the elderly are associated with poorer results than operatively managed fractures. We suggest that non-operative management is only used for undisplaced fractures or if the physical state of the patient means that they cannot undergo surgery. If it is to be used for displaced fractures, serial radiographs should be obtained after reduction to look for secondary displacement.
OPERATIVE MANAGEMENT
Operative management for ankle fractures in the elderly is associated with better results, but the surgeon has a number of challenges which differ from those encountered in younger patients. The poorer bone quality can make the usual methods of fracture reduction and fixation more difficult. For example, serrated reduction forceps, which are often used to reduce fibular fractures, can easily cause increased comminution with minimal force. Restoring length and rotation can be quite difficult and surgeons may have to rely on more indirect methods of reduction. In addition, comminution of the fracture fragments can make fracture reduction very difficult and the use of lag screws impossible. There are a number of operative techniques that can be used to treat ankle fractures in the elderly.
Conventional plating
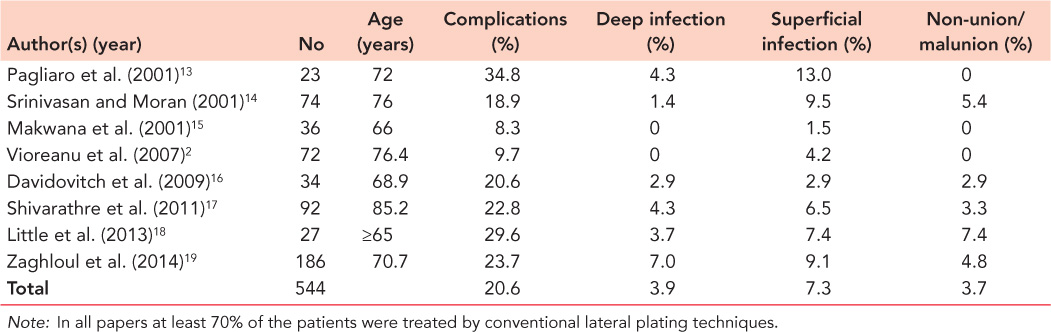
The standard technique used to treat ankle fractures in all ages is compression plating of the fibula with screw fixation of the medial malleolus and posterior malleolus, if required. In recent years different plates have been introduced, but compression plating and screw fixation remains in widespread use. The plates that are usually used are one-third tubular plates or dynamic compression plates. As has already been discussed, the results of plate fixation, combined with appropriate fixation of the medial and posterior malleoli, are better than those associated with non-operative management. A review of the results associated with plate fixation for ankle fractures in the elderly is presented in Table 42.2.2,13,14,15,16,17,18 and 19 It shows that the complications associated with plate fixation in the elderly range from 8% to 35%. The various studies in Table 42.2 list their complications differently but it should be understood that many of these complications are medical with deep venous thrombosis being a significant problem. Medical complications also occur in non-operative management. Table 42.2 shows that the surgical complications have a relatively low prevalence in elderly patients. The rates of deep infection, non-union and malunion are low and while the rate of superficial infection is higher, the papers indicate that it was usually successfully treated.
A number of studies have investigated functional outcome after plate fixation. Davidovitch et al.16 used the AOFAS score to compare patients <60 years of age with those aged ≥60 years. They showed no overall difference over a 12-month period, but older patients did report greater functional limitation than younger patients at 3 months, 6 months and 12 months. At 12 months after fixation 7.4% of patients aged >60 years reported functional limitation compared with 29% of patients aged <60 years. In a more recent study, Little et al.18 compared surgical treatment of SER IV ankle fractures (Table 42.1) in older and younger populations. They reported that despite the older patients having higher rates of diabetes and peripheral vascular disease, there were statistically better Foot and Ankle Outcome Scores in the geriatric population than in the younger population. They also reported that there was no significant difference in articular reduction, syndesmotic reduction, wound complications, postoperative infections or range of motion between the two groups. The literature suggests that 72–84% of elderly patients with ankle fractures return to their previous level of activity14,15,16,17,18 and 19 and Pagliaro et al.13 stated that 91% of patients were discharged home after initial fixation of the ankle fracture.
There is one study of plate fixation in the super-elderly.17 In this study 92.3% of patients were treated with conventional one-third tubular plates or dynamic compression plates and the remaining 7.7% had a locking plate. Table 42.2 shows that, as with the ≥65-year-old group, most of the complications were medical and that the prevalence of surgical complications was very similar to those seen in the elderly group of patients. The 30-day mortality was 5.4%. This rose to 8.7% at 3 months and 12% at 1 year. Despite the patients advanced age, 86% had returned to their pre-injury mobility by 3–6 months.
Locking plates
In recent years there has been considerable interest in the use of monoaxial and polyaxial locking plates to treat osteoporotic fractures. When screw purchase is poor, a fixed angle construct needs to be employed (Figure 42.2). In conventional plates part of the force created by screw insertion creates friction between the plate and the bone with the remainder left to resist the forces of physiological loading, such as weight bearing. In locking plating none of the screw force is used to create friction between the plate and the bone and thus the function of the construct is to resist physiological loading and maintain the alignment achieved at the time of fixation. In a cadaveric biomechanical model contoured locking plates for fibular fixation of osteoporotic bone were found to have higher torque to failure and maximal torque, compared with conventional non-locking methods.20 In theory this fixed angle construct may be advantageous in the elderly who may be less capable of complying with weight-bearing restrictions. It is, however, worth noting that failure of fixation with locked constructs occurs differently than with conventional plates. Instead of screw loosening and implant failure with loss of reduction, locked constructs undergo catastrophic failure. Since the screws are screwed into the plate, the screws rarely loosen and instead the bone around the screws tends to fail. This can result in catastrophic failure of the entire construct with cut-out and intra-articular penetration.21 Additionally, plate breakage can occur if there is insufficient working length or if non-locking screws are placed after locking screw insertion. Screw breakage may also occur below the plate due to the inability of the screws to loosen in response to repetitive axial loading.
Table 42.2 Complications listed in recent papers discussing use of plates in management of ankle fractures in the elderly
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








