Fig. 5.1
Water skiing mechanism of injury. As the boat accelerates, the upper torso is forcefully pulled forward, causing subsequent rapid eccentric hip flexion and knee extension against the resistance of the water and ski
Risk Factors for Proximal Hamstring Injury
Multiple risk factors have been reported for proximal hamstring injuries. In the National Football League, the preseason has been identified as the most vulnerable time frame for hamstring injuries due to relative deconditioning and weakness [7]. The most commonly described risk factors include previous hamstring injury [2, 8, 9], poor lower extremity flexibility [10, 11], core instability [12, 13], dehydration, strength imbalance [14, 15], fatigue [1, 16], and an inadequate warm-up [17]. A previous hamstring injury may lead to the formation of weakened scar tissue at the injury site, thereby lowering the capacity of the myotendinous unit to resist secondary injury [16, 18, 19]. Strength imbalance refers to either disproportionate hamstring-to-quadriceps strength in the same limb or the difference in hamstring strength between opposite lower extremities. With regard to the warm-up, increasing muscle temperature in order to prevent injury remains somewhat controversial but may increase the ability of the muscle tendon unit to resist strain [6, 17].
Clinical Presentation
At the time of an acute injury most athletes describe a sudden sharp pain in the posterior thigh or buttock. An audible or palpable pop may be associated with the pain. Classically described during the take-off phase of water skiing when the torso is pulled forward and the skis are pulled against the resistance of the water as mentioned earlier, this injury may also occur with sprinting, jumping, and kicking sports [4, 5, 20]. A smaller subset of individuals may describe progressive hamstring tightness eventually leading to an acute on chronic tear [6]. These injuries may present initially as discomfort with sitting [4, 6].
Differential Diagnosis
The differential diagnosis for proximal hamstring tendon avulsion includes the following [21, 22]:
Neurologic
Lumbar radiculopathy
Sciatica
Piriformis syndrome
Vascular
Arterial pathology (peripheral arterial disease/pseudoaneurysm/endofibrosis)
Venous pathology (pelvic deep vein thrombosis)
Compartment syndrome
Myotendinous
Hamstring strain or tear
Gluteal muscular tears
Traumatic/bony
Ecchymosis/bruising
Morel-Lavallee lesion
Ischiogluteal bursitis
Insufficiency fracture of pelvis (stress reaction)
Acute pelvic fracture
Apophysitis
Avulsion fracture of the ischial tuberosity
Sacroiliac joint pathology
On-the-Field Evaluation
Initial on-the-field or sideline evaluation of a suspected proximal hamstring injury should follow established trauma protocols, particularly if a fracture is suspected. Once the athlete is in a safe area (ideally on the sideline or out of the field of play) a more detailed and focused evaluation should be performed, including a thorough neurovascular examination. If the injury was not witnessed by the clinical evaluator, then the athlete, teammates, or coaches should be questioned to ascertain the mechanism of the injury. Further history taking should include a discussion of any previous injuries to the affected site.
Sideline physical examination should assess the point of maximum tenderness (i.e., origin, musculotendinous junction, mid-muscle belly, or distal hamstring). These areas should be further inspected and probed for any palpable soft tissue defects. Furthermore, the ischial tuberosity should be palpated for possible fracture. Motor strength should be assessed by grading the ability to flex the knee against resistance on a 0–5 scale. Knee flexion strength testing should be performed with the athlete prone and strength tested with knee at 90° of flexion, 45° of flexion, and at 0–10° of flexion. The athlete’s gait should be evaluated for pelvic drop, abnormal gait, ability to heel drag, and the ability to initiate a sprint. A stiff-legged gait may also be noted.
Evaluation of the tension of the distal portion of the hamstrings with the patient supine and with the hip and knee flexed to 90° is required for identifying proximal hamstring ruptures. The absence of palpable tension of the distal portion of the hamstrings, referred to as a positive bowstring sign, may be present. This sign suggests that there has been excessive lengthening of the proximal part of the tendons or complete proximal hamstring rupture [23].
Physical Examination
Physical examination in the office setting includes a repeat neurovascular examination to rule out lumbar spine and sciatic nerve pathology as well as any peripheral vascular concerns. The neurologic examination should also include assessment of the function of the tibial and peroneal branches of the sciatic nerve [21, 24]. When affected the athlete may experience a foot drop with possible ankle eversion weakness [25]. Additionally, a stiff-legged or antalgic gait may be noted when the patient is observed walking [4].
The thigh and buttock should be inspected with the patient prone. The evaluation should note any visible or palpable soft tissue defect. Severe ecchymosis is commonly present at the posteromedial thigh in the first 1–2 weeks following an acute tendon rupture (Fig. 5.2). The point of maximal tenderness should again be determined by palpation including palpation of the ischial tuberosity. Strength testing should again be performed prone with resisted knee flexion at 0–10°, 45°, and 90° of flexion and graded as described above.


Fig. 5.2
Photograph of ecchymosis of the posterior thigh 5 days after proximal hamstring rupture
The Reverse Plank test is a specific test that should be performed to evaluate hamstring function [4, 26]. This test (Fig. 5.3) is performed by having the patient supine and resting on the heels and flexed elbows. The core is contracted and the buttocks are lifted off the floor or examination table while the uninjured lower extremity is lifted forward. Pain and inability of the injured limb to elevate the buttocks off the floor is indicative of a hamstring injury. The standing heel-drag test is performed by having the patient drag the heel of the affected lower extremity against the friction of the floor in an anterior to posterior direction. The test is performed bilaterally with a positive result occurring when pain or discomfort is elicited at the ischial tuberosity of the injured limb [26].
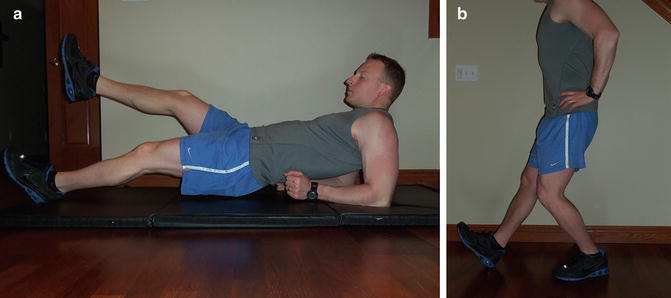
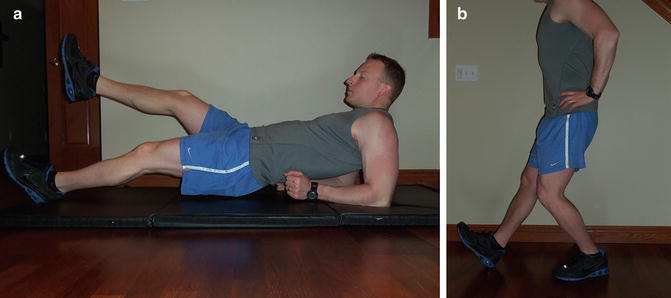
Fig. 5.3
(a) Reverse plank test. Examinee is supine and resting on the heels and flexed elbows. The buttocks are lifted off the floor or table while the uninjured lower extremity is lifted forward. Pain and inability of the injured limb to elevate the buttocks off the floor are indicative of a hamstring injury. (b) Standing heel-drag test. Examinee drags the heel of the affected lower extremity against the friction of the floor in an anterior to posterior direction. Test is positive when pain is reproduced at the ischial tuberosity
Multiple other special provocation tests have been described to evaluate for hamstring injuries [6]. The Puranen–Orava test (Fig. 5.4a) is performed with the patient standing with the hip flexed to 90° and the knee fully extended [6]. The examinee’s heel is held on a support by the examination table, a chair back, or railing. For the bent-knee stretch test the patient is supine and the hip and knee of the injured extremity are maximally flexed [6]. The examiner then slowly passively extends the knee. The modified bent-knee stretch test (Fig. 5.4) is also performed with the patient supine. The examiner maximally flexes the hip and knee and then rapidly extends the knee. For all tests described above, tendinosis, strain, or potential rupture of the hamstring is indicated by increased posterior thigh pain with extension of the knee. This series of examination tests has shown moderate to high validity and reliability for identifying hamstring injuries [6, 27].
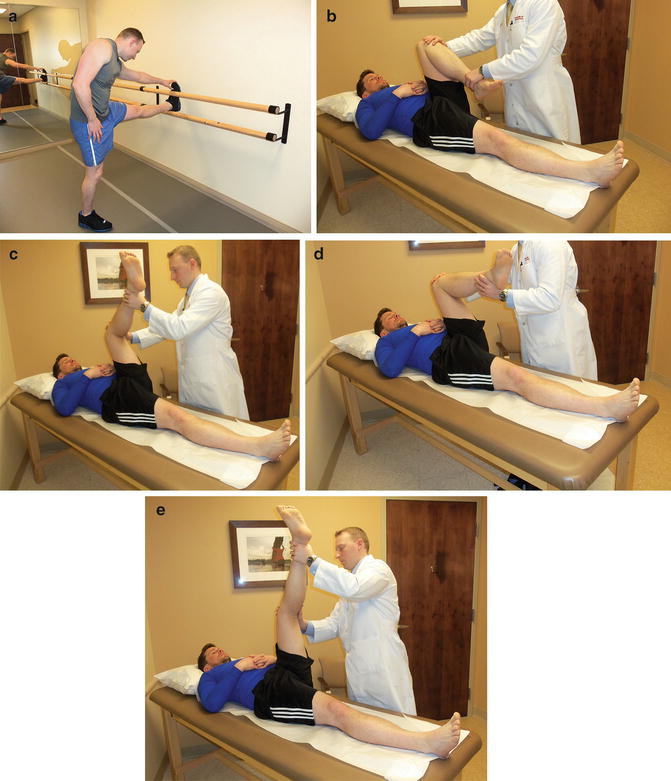
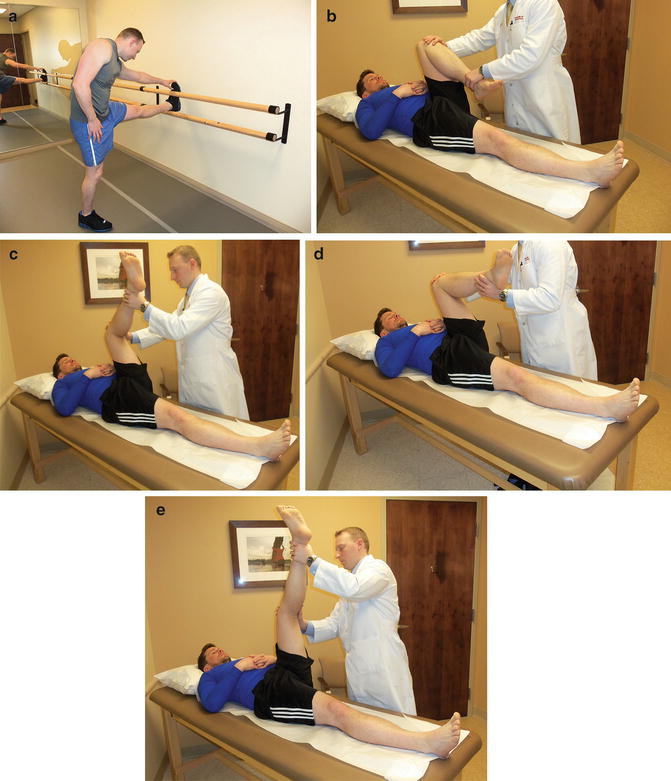
Fig. 5.4
(a) Puranen–Orava test. (b, c) Bent-knee stretch test. (d, e) Modified bent-knee stretch test
Imaging
Radiographs
Imaging evaluation in a patient with a suspected proximal hamstring injury should include an anterior/posterior X-ray view of the pelvis [4, 28]. Orthogonal views should also be obtained of the femur of the injured limb to confirm there is no associated proximal femur fracture present. Radiographs are typically normal but may be reveal an avulsion fracture of the ischial tuberosity [4, 28].
MRI
If radiographs are normal, magnetic resonance imaging (MRI) is recommended for making an accurate diagnosis. T2-weighted MRI series further assist in determining the pattern and severity of soft tissue injury including the number of tendons injured, complete versus partial rupture, chronicity, and the amount of tendon retraction (Fig. 5.5). Chronicity of the injury can be determined on T2 MRI based on the amount of fibrosis present [6, 29]. Additionally, MRI can determine the degree of soft tissue damage by defining the dimensions of abnormal T2 signal within and around the tendon substance, percentage of abnormal cross-sectional tendon substance, and extent of increased T2 signal intensity [30]. For proximal hamstring injuries, images should capture the ischial tuberosities and proximal thighs. Partial-thickness tears of the proximal hamstring complex may also be identified by a linear signal at the tendon–bone interface present on axial T2 images. This linear, crescent-shaped signal is referred to as the “sickle-sign” [26].
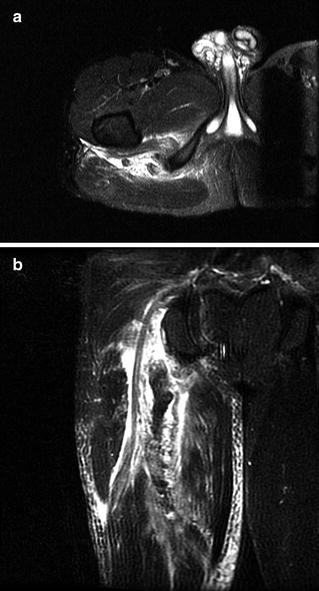
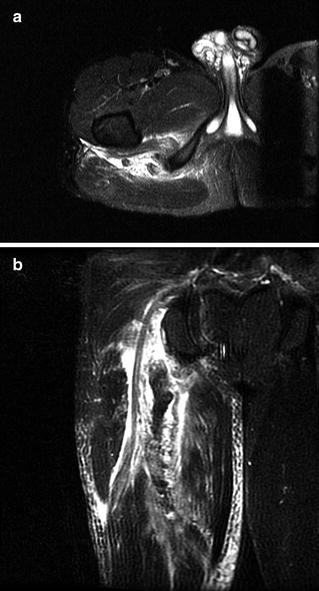
Fig. 5.5
(a, b) Axial and coronal cut T2 MRI demonstrating acute complete proximal hamstring avulsion tear with retraction
Ultrasonography
Recently ultrasound has increased in popularity and usefulness for identifying and classifying proximal hamstring ruptures. Ultrasonography has been demonstrated to be highly accurate in the acute setting for determining the extent and location of a hamstring tear [6, 18, 31]. This modality provides high-resolution imaging allowing for direct correlation with clinical examination and more immediate imaging [18]. The advantages of this technique include its relative inexpense, its high sensitivity and specificity, and its increasing availability in clinics and emergency department settings. The greatest disadvantage of using ultrasound for diagnosis of proximal hamstring tendon avulsion is that its accuracy is often dependent on the operator’s level of experience (Fig. 5.6).


Fig. 5.6
Longitudinal ultrasound image demonstrating retracted proximal hamstring avulsion rupture. Arrow points to biceps femoris stump
Classification
Hamstring injuries have been classified based on the anatomic site, pattern, and severity of the injury in the acute stage, as assessed by MRI or ultrasound [2, 6, 30, 32, 33]. Wood et al. described a clinical and anatomic classification system based on pattern of the tear and patient symptoms [1] (Table 5.1). Shelly and associates have described an MRI grading system for muscle injury that is commonly used to categorize hamstring injuries. In this system grade 1 is defined by a T2 hyperintense signal about a tendon or muscle without fiber disruption, grade 2 as a T2 hyperintense signal around and within a tendon with fiber disruption less than half the tendon width, and grade 3 as disruption greater than half its width [34]. Neither clinical nor radiologic classifications, however, have been precisely correlated with time to return to play after a hamstring injury.
Table 5.1
Classification of proximal hamstring tendon injuriesa
• Type I: Bony avulsion |
• Type II: Proximal MTJ tear |
• Type III: Incomplete avulsion |
• Type IV: Complete avulsion—w/o retraction |
• Type V: Complete avulsion—retracted |
A. + sciatic nerve symptoms |
B. − sciatic nerve symptoms |
A more detailed MRI scoring system has been devised by Cohen et al. [35] based on eight features. These include (1) player age, (2) number of muscles involved, (3) location of injury, (4) presence of insertional damage, (5) percentage of cross-sectional muscle involvement, (6) length of muscle retraction, (7) long-axis T2 sagittal plane signal abnormalities, and (8) presence of chronic changes. Recovery time >2 to 3 weeks was associated with multiple-muscle injury, >75 % cross-sectional involvement, presence of retraction, circumferential edema, and an MRI score of >15 [35]. This scoring system was found to be highly predictive of time missed from athletic participation [6].
Ischial Tuberosity Avulsion Fracture
Avulsion fractures of the ischial tuberosity typically occur in younger athletes particularly in the pediatric population as the child approaches skeletal maturity [36–38]. As with tendinous avulsions, these injuries typically result from a sudden forceful flexion of the hip joint while the knee is extended and the hamstring is contracted. Patients report sudden pain of the proximal, posterior thigh and a palpable or audible crack following a violent muscle contraction [22]. Clinical presentation typically includes localized pain and swelling, limited hip motion, and pain with sitting. Radiographs of the pelvis in the anterior to posterior plain should be performed for patients with suspected ischial tuberosity fracture and correlative clinical findings (Fig. 5.7). Fractures may be nondisplaced to widely separated with or without comminution. Occasionally a pseudarthrosis or an enlarged ischial mass may develop leading to chronic pain [39]. When radiographs are inconclusive, MRI or ultrasound may be required to evaluate soft tissue injury of the proximal hamstring as described above. As with all fractures, prompt and accurate diagnosis is essential for providing optimal treatment.


Fig. 5.7
AP pelvis radiograph demonstrating right ischial tuberosity avulsion fracture
Because of the limited literature on the treatment of ischial tuberosity avulsion fractures, there is no clear algorithm for the management of this injury [22, 37, 40]. Nonoperative treatment with activity modification and use of a cushioned seat are the mainstays of treatment for the vast majority of patients. An adequate period of rest and activity modification facilitates the best outcomes from conservative management [41]. Failure to heal with nonoperative treatment and/or displacement of greater than 2 cm are relative indications for surgery. However, there is no clearly defined amount of displacement that confirms the need for surgery [41]. A multitude of surgical options have been described to treat avulsions fractures including open reduction and internal fixation [22] and excision of the bony fragment [39] with or without repair of soft tissue to bone [41]. Potential complications of conservative treatment include nonunion of the avulsion fractures and “hamstring syndrome” in which shortening and fibrosis develop at the origin of the hamstrings [42]. An adequate period of rest and modified training seems to be important to facilitate optimal outcome of conservative treatment [41].
Most authors recommend operative treatment in fractures with displacement greater than 2 cm [41]. Ferlic et al. found that in the acute setting operative treatment led to excellent outcomes for displacement of fractures greater than 1.5 cm [41]. Gidwani and associates recommend early operative treatment in patients with displacement of more than 1 cm [43]. Multiple surgical options have been utilized including plate fixation and screw fixation [22, 43]. Surgical approaches via the gluteal crease or a modified Kocher–Langebeck approach may be performed with the patient placed prone and flexed or in the lateral decubitus position with the injured side positioned up and the limb draped free. Figure 5.8 demonstrates a displaced ischial tuberosity fracture post open reduction and internal fixation. Postoperative rehabilitation follows similar protocols as will be described later for tendinous avulsions.


Fig. 5.8
AP pelvis radiograph following fixation of ischial tuberosity avulsion fracture
Management of Proximal Hamstring Avulsions
As with ischial tuberosity avulsion fractures, early diagnosis and prompt treatment are the keys to the management of proximal hamstring avulsions. Activity level of the patient affects treatment decision-making with surgery being recommended more often for highly active patients. Delay in surgical treatment allows for greater tendon retraction making repair more difficult and increasing the risk of complications and inferior outcomes [44, 45]. Long-term sequelae of a neglected hamstring avulsion include pain, weakness, poor endurance, and sciatica due to tethering of the retracted muscle to the sciatic nerve [46]. A recommended treatment protocol is shown in Table 5.2.
Table 5.2
Treatment recommendations for proximal hamstring tendon avulsions
Single-tendon avulsion (with retraction 1–2 cm) |
Nonoperative treatment |
Return to sport at approximately 6 weeks postinjury |
Two–tendon rupture: Controversial (literature not well established) |
Nonoperative treatment for older (>50 years of age) and low-demand patients |
Surgical repair for: |
– Young patients (<50 years of age) |
– Athletically active patients |
– Tendon retraction >2 cm |
Three-tendon avulsion: |
Surgical repair |
Nonoperative Management
Nonoperative treatment is appropriate for proximal hamstring injuries involving only one tendon or if multiple tendons are involved but retraction is minimal [4]. This option is reserved for one- or two-tendon ruptures with less than 2 cm of retraction [4]. Nonoperative treatment is less successful for more significant injuries including complete three-tendon tears regardless of the extent of retraction [4, 6, 44, 45]. Less active patients, those with medical comorbidities, and patients unable to comply with postoperative rehabilitation are also indications to manage these injuries nonoperatively [6]. One notable complication of nonoperative treatment is hamstring syndrome. This is characterized by posterior buttock pain, discomfort with sitting, and worsening pain when performing hamstring stretching and strengthening exercises [6, 47].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







