Modalities
Therex
Ambulation
Manual therapy
Functional exercise
Acute (0–5 days)
RICE: rest, ice, compression, elevation (0–72 h)
None
Crutch ambulation for grade II/III strains
None
None
Repair (5 days–6 weeks)
NMES: neuromuscular electric stimulation to improve quadriceps activation
Early: (1–3) AROM, AAROM heel slides, quad sets, 4-way SLR, bike, core exercises
Normalize gait pattern
AAROM/PROM *pain-free range
Closed chain exercises with good volitional quad: step-ups, leg press, lunges
Remodel (7–12 weeks)
PREs: isotonic, isokinetic
Conditioning: jogging, bike, elliptical
Cross-friction; Graston; contraction/relaxation
Quad eccentrics, plyometrics
Return sport
WNL strength: isokinetic functional exercises
Interval running, sprinting
WNLs PROM quadriceps
Sport-specific exercises without pain
Acute Stages: 0–5 Days
In the first 24–72 h, follow the RICE (rest, ice, compression, elevation) principles to prevent worsening of the initial injury. They consist of the application of ice at 15–20 min intervals with 60 min between applications to lower intramuscular temperature and decrease blood flow (shown to be 50 %) along with compression and elevation, which also serve to minimize interstitial fluid accumulation [1, 6]. In the case of contusions, it has been recommended that, in addition to the application of ice and elevation, the knee be splinted in a brace or elastic compression wrap with the knee in a flexed position for the first 24 h to limit hematoma formation. The use of crutches is recommended in the acute stages for those athletes who have sustained a grade II or grade III tear or contusion to minimize additional stress to the injured muscle and where there is evidence of an antalgic gait pattern [1, 9, 10].
Repair Phase: 5–7 Days to 6 Weeks
The repair phase of muscle begins approximately 5–7 days after injury and can last up to 6 weeks [1, 8, 9]. It is during this phase when more active therapies may begin to facilitate healing without risking the deleterious effects of immobility, including muscle atrophy, and excessive scar tissue formation [11]. It has been shown that early mobilization facilitates the healing process with improved alignment and regeneration of myofibers [1]. Some early active therapies include (active range of motion [AROM], active assistive range of motion [AAROM]) heel slides, stationary bike, and walking on a treadmill to normalize gait pattern. Care should be taken to avoid overly aggressive ROM or exercises in the early phases, especially with larger injuries, as they can result in delayed healing and complications such as myositis ossificans [9, 12, 13]. The use of modalities such as therapeutic ultrasound and neuromuscular electrical stimulation (NMES) is warranted to decrease pain and to improve quadriceps muscle activation, as experimental studies have concluded that pain and effusion can lead to quadriceps inhibition [14]. Maintaining a level of aerobic fitness during the convalescent period should be considered with low-impact activities such as swimming and the use of upper body ergometer (UBE) to minimize effects of deconditioning [9].
The progression to strengthening exercises during the repair phase is based on biologic healing principles of the muscle and guided by symptoms. The early scar contains primarily type III fibers, but is replaced by type I fibers by around the tenth day and no longer represents the weakest part of the injury site based on experimental models [7, 15, 16]. The exercises should be relatively pain-free to avoid tearing the scar tissue bridge and proceeded by an active warm-up to reduce muscle viscosity, improve neural pathways, and improve elasticity.
The predominant strengthening exercises in the early repair phase consist of open kinetic chain exercises with isometric and multi-angled isometrics including quadriceps sets, multidirectional straight leg raises (SLR), and short arc knee extension with light to no resistance (Fig. 11.1a–c). The inclusion of resistance and closed kinetic chain exercises may be initiated when there is good volitional quadriceps contraction without evidence of a quadriceps extensor lag performing a straight leg raise and/or signs of an antalgic gait pattern [11]. Based on the size and severity of the injury, closed chain exercises may be started with partial weight bearing in limited ranges (leg press, shuttle) and progress to full weight bearing through full range (step-ups, squats). From the mid- to late repair phases, there is overlap between the repair and remodeling phases. It is at this juncture that larger controlled stresses can be placed across the injured muscle to help remodel the scar and improve the contractile strength of the regenerated muscle tissue. Exercises in this phase may include concentric and eccentric heel taps, lunges, sport cord resisted directional walking, BOSU ball squats, resisted kicking, and submaximal isokinetic knee extension (Fig. 11.2a–e). The continuation of variable resistance open kinetic chain quadriceps strengthening should continue as the specificity of open chain kinetic quadriceps exercises has been proven to have greater training effects in restoring quadriceps strength in anterior cruciate ligament (ACL) protocols compared to closed kinetic chain exercises [17].
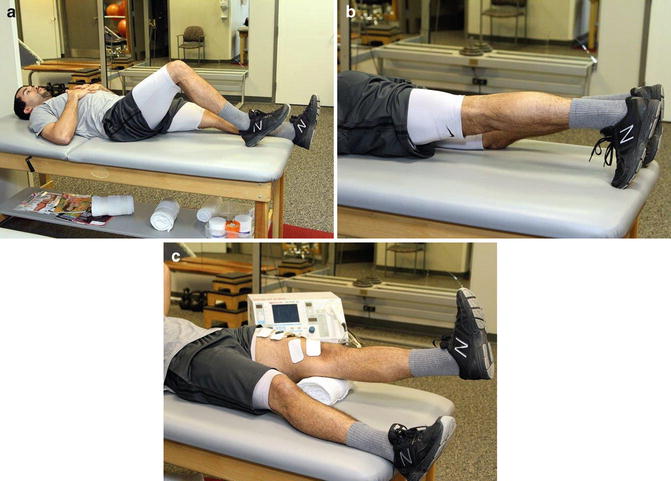
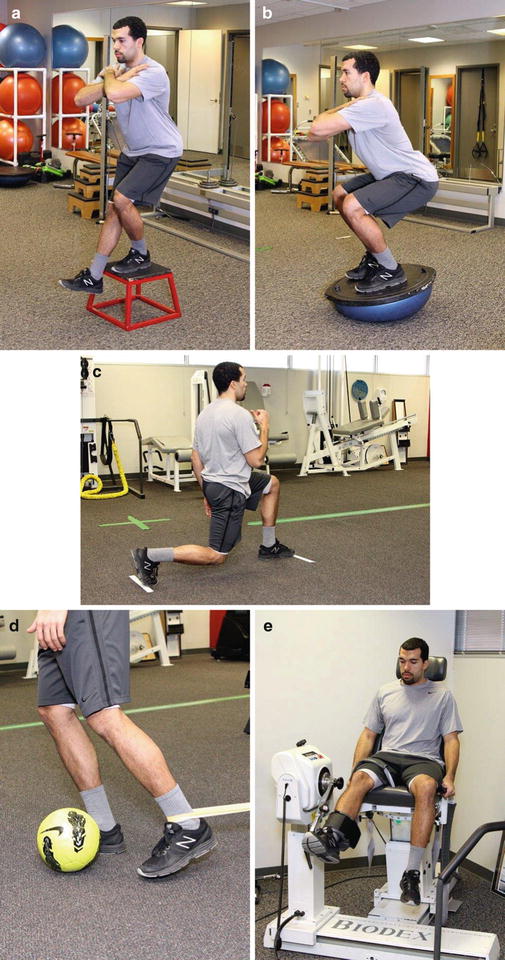
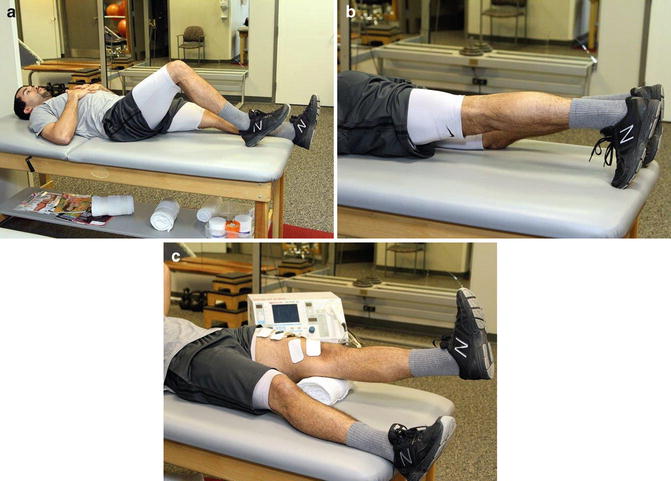
Fig. 11.1
(a) Heel slide. (b) Prone quadriceps set. (c) NMES: short arc quadriceps
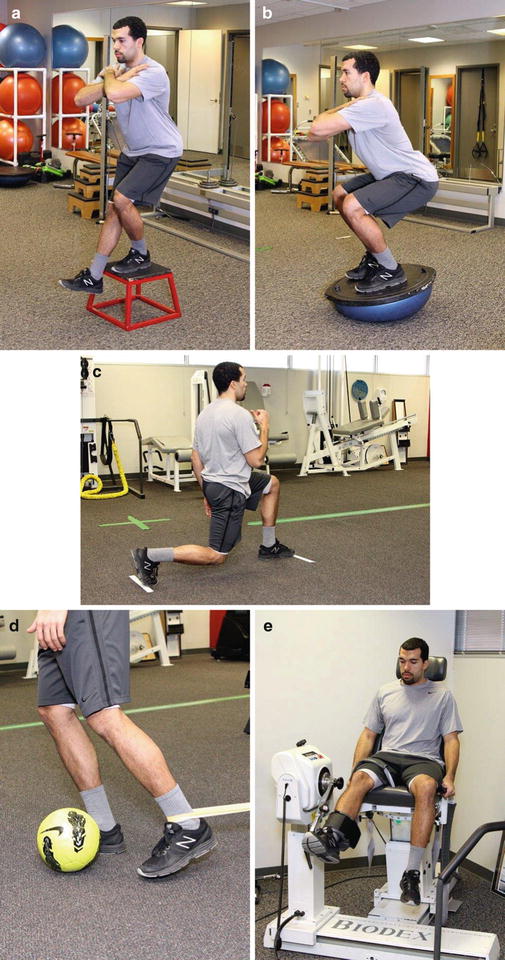
Fig. 11.2
(a) Heel taps. (b) BOSU squats. (c) Lunge. (d) Resisted kicking. (e) Isokinetic knee extension/flexion
Particular attention to form is necessary while the athlete performs exercises to avoid compensatory or substitution patterns, such as excessive hip flexion, pelvic drop, or knee valgus due to either pain or weakness in the quadriceps and proximal hip muscles.
It is also during the mid- to late repair phase where manual therapy techniques may be implemented to help realign the healing tissue and avoid restrictions of the muscle scar and connective tissue near the injury site. The incorporation of manual therapy such as cross-friction massage, instrumented techniques with Graston, PNF contract/relax, and static passive stretching will help remodel the scar tissue and restore tensile properties of the muscle (Fig. 11.3). The goals to progress to the next phase are achieving near-full pain-free ROM with passive knee flexion, good proprioception and neuromuscular control of the lower extremities and core, and no significant observable strength deficits during functional testing (squats, step downs).


Fig. 11.3
Soft-tissue technique
The inclusion of core exercises is important in the subacute phase and later phase of rehabilitation, as studies have shown a decreased incidence of lower extremity (thigh/groin) injuries in athletes participating in Australian rules football completing a preseason core training using real-time ultrasound while performing neuromuscular control exercises. The exercises were designed to target the transverse abdominis and multifidus while performing various postures and movement patterns. Those players participating in the program demonstrated an increased cross-sectional area of the targeted muscles measured through ultrasound and missed fewer games due to injuries than the control group [18, 19]. It is postulated that with fatigue of the core muscles, altered neuromuscular control leads to fatigue and increased stress/strain to the lower extremity muscles, especially those muscles with attachment to the pelvis [18, 19]. The inclusion of core exercises will assist in the recovery and help prevent lower extremity injuries [20, 21]. The trunk (core) muscles serve as a foundation for movement, acting in both a stabilizer role through local stabilizer muscles (transverse abdominis, multifidus, internal obliques) as well as a global role with the transference of forces through muscles of the trunk (rectus abdominis, iliocostalis) with integrated kinetic chain activities such as running and kicking [21]. The mechanics of kicking a ball while playing soccer, for instance, increases the internal movement of the quadriceps when the torso is inclined backwards and shifted laterally to the plant leg, while the kicking leg hip generates force through the hip and quadriceps. Engagement of the core muscles (transverse abdominis, multifidus, quadratus lumborum) helps to offset the potential strain caused by these high generating forces in the distal segments [1, 9, 14, 20–23].
Incorporating exercises such as abdominal bracing in both static and dynamic postures has shown to have higher EMG (electromyographic) values for the deep abdominal stabilizers than some other dynamic trunk flexion exercises such as sit-ups and curl-ups and so would be advantageous to incorporate the maneuver into exercises and training to help offset some of the potential deleterious forces to the quadriceps with sporting activities [1, 17, 24]. Other EMG studies have quantified percentage values for some of the traditional stabilization exercises targeting the multifidus and longissimus and found high-percentage maximum value isometric contraction (MVIC) values for prone lumbar extension to end range with applied resistance [22, 23], and a study using wire-inserted EMG found highest percentage activation of the transverse abdominis with alternating arm and leg from plank position [25] (Fig. 11.4).


Fig. 11.4
Plank with alternating arm and leg
Likewise, the hip muscles serve an (gluteus medius and maximus) important role with lower extremity stability and control. Studies have shown that a decrease in gluteus strength and activation patterns lead to suboptimal performance and alignment of the distal lower extremity, with increased knee valgus, femoral adduction, and internal rotation associated with various musculoskeletal disorders such as iliotibial band syndrome and patella-femoral pain [20, 23, 26]. The inclusion of gluteal exercises as part of the quadriceps rehabilitation should be integrated to optimize the function of the lower extremities with higher-level muscle demands and reduce the risk of suboptimal performance and risk of reinjury [20, 23]. Some exercises have been shown to have higher percentage activation targeting the hip abductors (gluteus medius/minimus) and hip extensors (gluteus maximus). A study by Boren et al. [27] analyzing percentage of MVIC for common exercises found the front plank with hip extension, side plank with hip abduction, and single-leg squat to have the highest combined activation of the gluteus medius and maximus out of 22 commonly prescribed hip exercises. Therefore, these high-value combined gluteal exercises should be considered as part of the quadriceps rehabilitation program to ensure kinetic chain restoration.
Remodeling Phase: 7 Weeks to 3 Months
The remodeling phase focuses on restoring full tensile strength, power, ROM, and endurance in the involved leg with a progression to more sport-specific exercises. The inclusion of higher-level exercises such as plyometrics, variable-speed eccentrics, and jump and landing exercises that are closely aligned to the physical demands of the quadriceps in sport. The incorporation of eccentric exercises is fundamental and has consistently been shown to increase the development of optimum length tension in the knee extensors [1, 28]. Functionally, the quadriceps is utilized frequently in an eccentric manner in sports to decelerate, as in the case of changing speed and direction and with the plant leg during an approach to kick a ball. Most quadriceps injuries are also thought to occur with eccentric movements during deceleration [1, 29, 30]. Therefore, it is imperative to incorporate eccentrics into the remodeling phase to prepare the muscle for return-to-play activities [1, 6, 9, 18]. Some of the exercises included in this phase are shuttle jumps, directional jumping, box jumps, reverse Nordic, sport cord deceleration, reverse lunges, pistol squats, and resisted side hops (Fig. 11.5a–f). A study by Brughelli et al. [31] showed a 6.5° shift in the knee extensors with a 4-week supplemental eccentric training program and no incidence of injury compared to a control group where there were incidences of central tendon injuries in soccer. The ability of the quadriceps to have an adaptive response has been shown to occur with eccentric training, whereby an initial drop in peak torque and delayed soreness was followed by a shift in the optimum angle after only the first bout of exercise [28]. Although there are not any eccentric protocols in the literature, it has been recommended that volume and intensity of eccentric exercises be incorporated gradually to avoid injuring the muscle. Delayed onset muscle soreness, which is common following eccentric exercises, should not persist for more than 1–2 days [11, 32, 33]. It is also recommended that eccentric exercises be performed at the end of the session due to the neuromuscular and strength impairments that occur immediately afterwards [1, 32].


Fig. 11.5
(a) Shuttle jumps. (b) Box jumps. (c) Reverse Nordic. (d) Sport cord deceleration. (e) Pistol squat. (f) Resisted lateral hops
Functional Return to Sport
Although there are no established criteria for return to sport following a muscle injury, with most of the supporting evidence being expert opinion [9, 34], there are some general guidelines. The guidelines include pain-free ROM and near-normal strength (isokinetic testing) preceded by good performance on field or functional performance tests [9]. Due to the frequent involvement of the rectus femoris with quadriceps injuries as well as the biarticular function as a hip flexor and knee extensor, strength and ROM testing for knee extension should then be done both with the hip flexed (in sitting) and the hip extended position in prone, if the rectus femoris is involved (Fig. 11.6). If available, the use of isokinetic testing can provide invaluable clinical objective measures to support performance on field tests. Isokinetic quadriceps strength has been shown to have a high correlation with single jump for distance [35]. Schmitt et al. [36] analyzed isometric quadriceps femoris strength for individuals returning to sport following ACL rehabilitation protocol. They found those individuals whose quadriceps deficit was greater than 15 % of the control leg performed worse during functional hop tests, which translated to worse self-reported functional measures than those athletes with less than 10 % deficits who performed well on functional field tests. Having knowledge of intrinsic risk factors to quadriceps injury such as a history of previous muscle injury or decreased quadriceps flexibility will allow the residual deficits to be addressed prior to initiating functional return-to-sport activities. A prospective cohort study by Haaglund et al. [37] found intrinsic factors such as previous muscle injury increased the risk of reinjury threefold in soccer teams over a 9-year span. Additionally, having a previous injury to a different lower extremity muscle group increased the rate of injury to the quadriceps and calf muscles due to altered biomechanics of running.









