41 Acute Monoarthritis
Inflammatory arthritis causes morning stiffness and pain with restricted joint movement.
Pain worsening after movement usually indicates mechanical joint pain.
Soft tissue disorders usually produce pain in a periarticular distribution.
Acute monoarthritis presentations (developing suddenly) are usually related to trauma.
Synovial fluid analysis is the most valuable laboratory test in acute monoarthritis.
The sudden onset of monoarthritis in a synovial joint is a significant clinical event. The most serious cause is joint infection because of associated mortality (≈15%) and probability of impaired long-term function. However, the commonest of the differential diagnoses (Table 41-1) is trauma or inflammation. Each presentation of monoarthritis requires immediate investigation and treatment to limit pain and prevent joint destruction. The British Society of Rheumatology and British Orthopaedic Association generated guidelines (Figure 41-1) to assist physicians in the diagnosis of the acutely swollen joint1 based on history, examination, radiologic, and blood and synovial investigations.
Table 41-1 Causes of Acute Joint or Periarticular Pain*
| Common Acute Monoarthritis |
| Trauma or Internal Derangement |
| Acute Monoarthritis of Polyarthritis |
| Monoarthropathies from Noninflammatory Disease |
| Synovial Diseases |
| Acute Monoarthritis of Systemic Disease |
| Soft Tissue Lesions |
| Bone Diseases |
* This table shows the causes of inflammation in any one joint (monoarthritis) and pain around the joint that presents without inflammation (monoarthropathy).
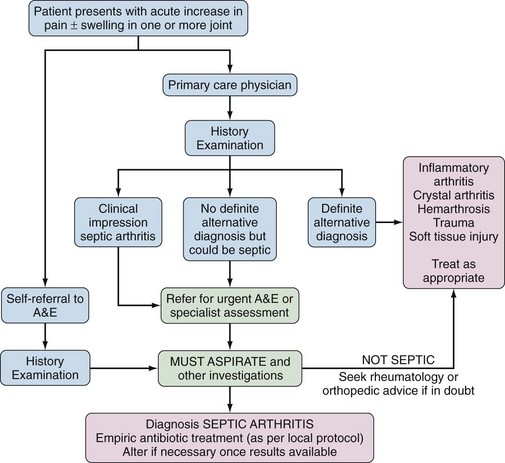
Figure 41-1 British Society for Rheumatology and British Orthopaedic Association guidelines for management of the acutely swollen joint.1 A&E, accident and emergency department.
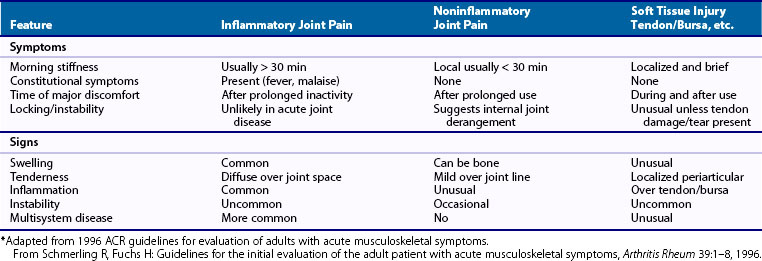
History
One should examine the patient’s age, occupation, and social, drug, travel, and sexual history. Pain and joint stiffness, its diurnal variation, and aggravating and relieving factors should be sought, and a history of swelling should be established. Specific features of relevance include trauma, joint locking, and presence of systemic symptoms (fevers, sweats, rigors, and weight loss). Inquiring about ocular, oral, respiratory, gastrointestinal, or skin symptoms can facilitate the diagnosis. Inquiring about ocular, oral, respiratory, gastrointestinal, or skin symptoms can facilitate the diagnosis if the monoarthritis is a presentation of a chronic arthropathy, related inflammatory disease, postinfectious phenomenon, or connective tissue disease. Table 41-2 summarizes symptoms and signs that characterize patients with inflammatory or noninflammatory joint disease and soft tissue disorders2 to help initial evaluation.
Examination
The Regional Examination of the Musculoskeletal System (REMS) can be used to identify monoarticular abnormalities.3 Physicians should look, feel, and move joints to assess function—comparing the affected joint and normal side and for evidence of more widespread disease. In any acutely swollen joint, examination should include looking for local signs of inflammation (pain, erythema, swelling, heat, and loss of function). Any patient with preceding arthritis should be assessed for chronic changes to joint structure and disability. Local synovial swelling and/or effusion, joint instability, limited movement, and deformity of any single joint necessitate detailed investigation. Local monoarticular tenderness without swelling could indicate enthesitis, tendinitis, bursitis, or bone disease. A complete examination should look specifically for ocular signs, skin rashes, ulcers, and nodules.
Investigations
Imaging Studies
A range of imaging studies assist in diagnosis of acute monoarthritis.4
1. Plain radiographs identify soft tissue swelling, calcium in periarticular tissues, fractures, local bone disease, and loose bodies, as well as destructive changes in long-standing arthritides.
2. Computed tomography (CT): CT scanning better identifies fractures, bone diseases, and intra-abdominal and chest pathology. It is useful when magnetic resonance imaging (MRI) is contraindicated. In acute arthritis, CT scan can show osteomyelitis over and above acute inflammation.
3. Musculoskeletal ultrasound (US): US is increasingly reliable for use in rheumatology practice provided practitioners are appropriately trained.4 US is quick, efficient, and cheap and as effective as MRI and clinical examination in detecting synovitis5 and soft tissue damage in acute shoulder injury.6 In acute monoarthritis US can show loculated synovial fluid to better target aspiration and injection,7 and power Doppler views can demonstrate increased blood flow in active synovitis.8 US is recommended for detection of synovitis by the European League Against Rheumatism (EULAR) in early arthritis.9
4. MRI: Although it is the best technique for soft tissue imaging, MRI is time consuming and costly. MRI can diagnose internal ligament damage and tendon enthesitis and is most effective in identifying avascular necrosis of bone. MRI is also useful when identifying the extent of inflammation in acute monoarthritis and subclinical joint involvement. EULAR also suggests MRI for diagnosis of acute early arthritis.9
5. Arthrography: Imaging internal joint structure after injection of radiopaque solutions in association with CT scanning is useful for hip cartilage tears and in situations when MRI is not feasible.
6. Radionuclide scans. Bone scanning with technetium-labeled methylene diphosphonate identifies osteoid osteomas, bone sarcomas, bony metastases, osteomyelitis, and stress fractures not seen on plain radiographs. Bone scintigraphy is helpful when excluding bone and joint disorders in patients with chronic pain syndromes. Although not specific in acute arthritides, bone scans show differences in the pattern of joint involvement between inflammatory conditions and osteoarthritis. Labeled white cell scans can identify areas of infection, especially when the source of infection is uncertain in patients with septic arthritis.
Synovial Fluid
The most useful test in acute monoarthritis is examination of synovial fluid, which should be analyzed for color and cloudiness (Table 41-3). One should use microscopy to characterize the predominant cells, Gram stain to detect bacteria, and polarized light analysis to identify uric acid or calcium pyrophosphade dehydrate (CPPD) crystals.1 Identification of bacteria following synovial fluid culture can provide results even when a Gram stain is negative. Neisseria organisms are fastidious with low yields from culture, but polymerase chain reaction (PCR) can detect Neisseria-specific deoxyribonucleic acid (DNA).
Table 41-3 Synovial Fluid Characteristics in the Clinical Situations, with Imaging and Investigation Techniques Best Used to Identify the Cause
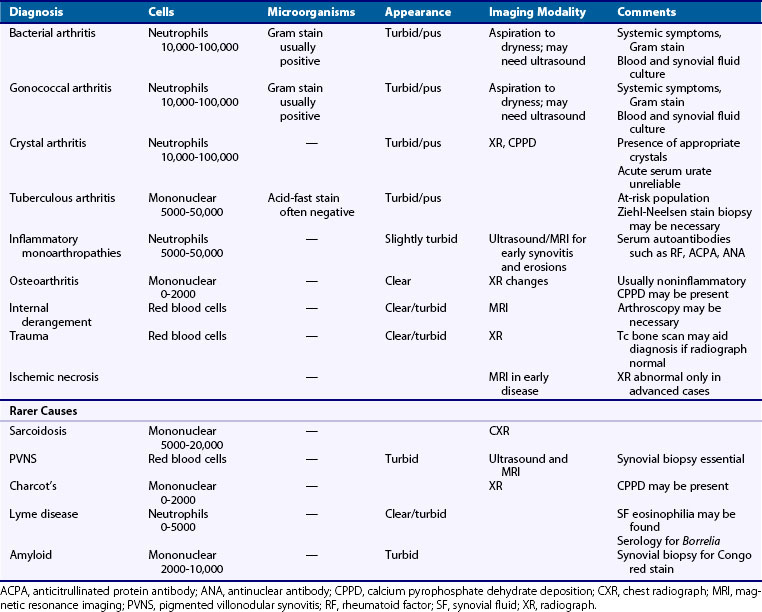
Many centers measure synovial fluid WCC, which may differentiate inflammatory and noninflammatory presentations but crucially fails to differentiate between inflammation and infection. Low synovial fluid glucose and high lactate10 and procalcitonin11 are found in septic arthritis, but evidence that these can separate infectious from inflammatory arthritis in a clinically meaningful way is limited. Bacterial identification in synovial fluid from patients with septic arthritis can be inhibited by prior antibiotic use, and hence a careful drug history should be elicited.12 CPPD crystals are difficult to detect, so in both cases a clinical diagnosis should not be excluded if symptoms, signs, and investigations are suggestive.
Synovial or Bone Biopsy
Arthroscopic synovial biopsy is rarely necessary, but in tuberculosis, sarcoidosis, amyloid, pigmented villonodular synovitis, lipoma arborescens, and foreign body synovitis it is often required for diagnosis.13 Proteomic and genomic assays begin to show differences in the synovium from chronic arthritides, so synovial biopsy use may increase in the future. Bone biopsy may be needed to identify tumors and relevant factors in nonresolving osteomyelitis.
Specific Diagnoses
Acute Monoarthritis
Septic Arthritis (Bacterial)
The presence of bacteria in synovial fluid or after culture is a medical emergency because the acute mortality of septic arthritis is approximately 15%.14 Large limb joints are most frequently involved,15 usually associated with underlying osteoarthritis or inflammatory arthropathies, especially RA.14,16 Patients are particularly at risk following joint surgery, arthroplasty, or intra-articular injection, as are patients with a distant infection, intravenous drug users,17 and those with underlying disease or drugs that impair the immune response.18 Recent studies have shown that the most deprived in our communities are also at risk.14
History often elicits an acute, painful, swollen monoarthritis, but it is noteworthy that more than 10% of patients with native joint infections present with polyarticular infection. At presentation, an identifiable distant site of infection may be found, but fever occurs in less than 50% and sweats/rigors occur in approximately 30%.14 Blood cultures may identify bacteria in patients where synovial fluid culture is negative. At presentation, ESR and CRP are almost invariably raised, but approximately 35% of all septic arthritis patients do not have a raised WCC, and when infection is in the context of underlying RA this figure rises to 50%. Impaired renal and liver function at presentation can predict a poorer outcome.14
Plain radiographs show soft tissue swelling, and ultrasound localizes synovitis and fluid collection to target aspiration. MRI may demonstrate additional osteomyelitis. Synovial fluid is usually cloudy with a high WCC, and Gram stain should be undertaken.1 Synovial fluid culture is mandatory, yielding an organism after culture in approximately 50% of cases—local protocols for antibiotic use should be instigated therefore before culture results are available. Organisms detected most commonly include staphylococci (Staphylococcus aureus and Staphylococcus epidermidis), streptococci, and gram-negative bacteria with an increasing prevalence of methicillin-resistant S. aureus.12,19 Prompt intervention can reduce mortality10,14; hence the joint must be aspirated to dryness, but this can usually be done without recourse to surgical intervention.20
Interestingly, results from history, examination, routine investigations, and outcome are identical when comparing patients with bacteria-proven septic arthritis with those where a clinical diagnosis of septic arthritis is made but where bacteria cannot be isolated.12 Hence absence of systemic symptoms and normal investigations should not negate a strong clinical diagnostic suspicion.
Infection with Neisseria gonorrhoeae can be asymptomatic but should be suspected in sexually active patients presenting with migratory arthralgias, tenosynovitis, skin rashes, and vesicles. Untreated Neisseria infection can also lead to destructive arthritis. Most patients will be febrile with a raised acute phase response and blood WCC, but as with other bacterial causes of septic arthritis these may be normal at presentation.21 Investigations should include swabs from the urethra, cervix, pharynx, and rectum, inoculated immediately on Thayer-Martin medium. In contrast with other bacteria, polymerase chain reaction has been used on synovial fluid to improve positive results.22
Crystal Arthritis
Gout
Podagra is the classic monoarthritis of the first metatarsophalangeal joint, but other lower limb joints can be affected.23 Patients tend to be obese males, aged 40 to 50 with hypertension, and consumers of excess alcohol.24 Increasingly, postmenopausal females with low estrogens and who take loop diuretics for hypertension are predisposed to gout. Tophi are indicative of the diagnosis.
Fever is present in 34% of patients, especially in polyarticular presentations.25 In acute settings, blood WCC, ESR, and CRP are raised and to this extent gout mimics septic arthritis. Serum uric acid may be raised, but levels are low in 33% during acute attacks.26 Renal and liver function should be assessed. Needle-shaped uric acid crystals (that are negatively birefringent under polarized light) are present in synovial fluid or tophi aspirate and confirm the diagnosis.27 Synovial fluid should be examined for bacteria to exclude concomitant septic arthritis.
Routine radiographs frequently show no bony abnormalities but may identify erosions after repeated or prolonged attacks. Diagnostic ultrasound and MRI can identify synovial fluid for aspiration, tophi, and erosive disease.28
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree