Chapter 60 Acute Dislocations
Indications for Open Reduction
Open reduction of an acute dislocation usually is indicated in the following circumstances:
1. If anatomical, concentric reduction cannot be achieved by gentle, closed techniques with the patient under general anesthesia. Interposed soft tissues or osteochondral fragments may contribute to the irreducibility.
2. If a stable reduction cannot be maintained. Articular fractures often are unstable and must be reduced and fixed to ensure stability of the reduction.
3. If careful evaluation before closed reduction reveals normal neurological function and, after reduction, a definite, complete motor and sensory nerve deficit becomes evident.
4. If circulatory impairment distal to the injury is well documented before reduction and persists after reduction. Further assessment of the circulation is essential and should include arteriography.
5. If ischemia is persistent. Surgical exploration with appropriate management of the vascular injury is indicated.
Ankle
Dislocations of the ankle without fracture of either the medial or lateral malleolus or the anterior or posterior lip of the distal articular surface of the tibia are extremely rare. Usually, any dislocations that do occur are easily reduced by closed methods. Posterior dislocation of the fibula behind the tibia may contribute to difficulty with closed reduction and at times may require open reduction. Ruptures of the deltoid ligament, the anterior tibiotalar ligament, and the anterior and posterior talofibular ligaments occur alone or in combination. Controversy exists over acute ligamentous repair without evidence of fracture. Good-to-excellent results are possible without acute ligamentous repair; however, syndesmosis and mortise widening should be treated operatively if present. (For discussion of acute fractures of the ankle, see Chapter 54; of malunited fractures of the ankle, see Chapter 58; and of ruptures of the ligaments of the ankle, see Chapter 89.)
Patella
Acute Dislocations of the Patella
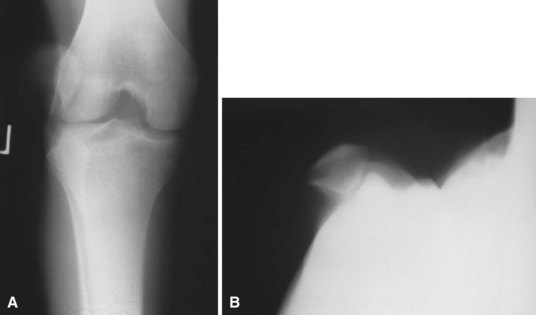
Acute dislocations of the patella usually are managed by closed methods (Fig. 60-1). The patella is almost always dislocated laterally, and extension of the flexed knee with pressure applied to the lateral margin of the patella results in reduction. The limb is immobilized in a knee immobilizer for 3 to 6 weeks and then motion is begun to prevent arthrofibrosis and to promote the formation of strong collagen along the lines of stress. Radiographs should be evaluated carefully to ensure that no osteochondral fragments are displaced within the joint. If a hemarthrosis is present, MRI is warranted to check for osteochondral fragments. One study demonstrated articular cartilage injury in 94% of patients; 72% had an osteochondral or chondral fracture, and 23% had patellar microfractures.
Arthroscopic techniques for the repair of the medial patellar retinaculum after acute patellar dislocations have been described, but we prefer the open method at our institution if repair is indicated (Fig. 60-2).
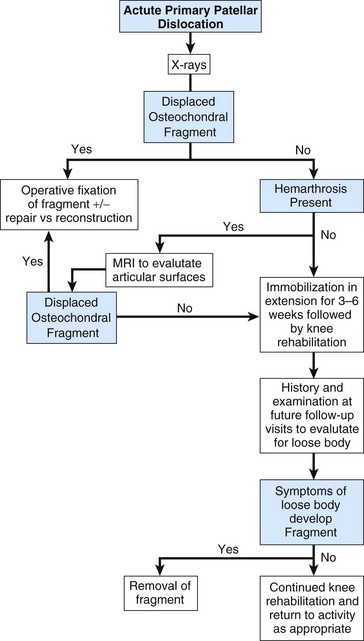
FIGURE 60-2 Algorithm for guiding the evaluation and management of acute primary patellar dislocation.
(Modified from Mehta VM, Inoue M, Nomura E, Fithian DC: An algorithm guiding the evaluation and treatment of acute primary patellar dislocation, Sports Med Arthrosc Rev 15:78, 2007.)
Open Reduction and Repair of Patellar Dislocation
 Through a medial parapatellar incision, explore the tear in the medial patellar retinaculum.
Through a medial parapatellar incision, explore the tear in the medial patellar retinaculum.
 Irrigate and explore the knee joint. Remove or fix any loose osteochondral fragments, and make a thorough search for any further loose fragments or intraarticular damage to the joint.
Irrigate and explore the knee joint. Remove or fix any loose osteochondral fragments, and make a thorough search for any further loose fragments or intraarticular damage to the joint.
 Repair any disruption in the vastus medialis muscle belly or in the medial patellar retinaculum.
Repair any disruption in the vastus medialis muscle belly or in the medial patellar retinaculum.
 Pay careful attention to that portion of the vastus medialis that originates in the region of the femoral adductor tubercle. If this origin has been disrupted and has retracted proximally, the angle of insertion of the vastus medialis muscle fibers into the patella is significantly changed. These fibers are vital to the prevention of recurrent lateral dislocation of the patella.
Pay careful attention to that portion of the vastus medialis that originates in the region of the femoral adductor tubercle. If this origin has been disrupted and has retracted proximally, the angle of insertion of the vastus medialis muscle fibers into the patella is significantly changed. These fibers are vital to the prevention of recurrent lateral dislocation of the patella.
 A lateral release may be performed if indicated.
A lateral release may be performed if indicated.
Grafting of the Medial Patellar Retinaculum
 Prepare a semitendinosus autologous graft or allograft.
Prepare a semitendinosus autologous graft or allograft.
 Center the skin incision between the medial edge of the patella and adductor tubercle.
Center the skin incision between the medial edge of the patella and adductor tubercle.
 Identify the extensor retinaculum.
Identify the extensor retinaculum.
 Make a small incision at the medial edge of the patella and just distal to the adductor tubercle.
Make a small incision at the medial edge of the patella and just distal to the adductor tubercle.
 Using a hemostat, pass the graft through a tunnel between the capsule and retinaculum.
Using a hemostat, pass the graft through a tunnel between the capsule and retinaculum.
 Secure the graft to the femur using suture, interference screw, or a suture anchor.
Secure the graft to the femur using suture, interference screw, or a suture anchor.
 After cycling the knee to ensure correct isometry, attach the graft to the patella with an interference screw or suture anchor.
After cycling the knee to ensure correct isometry, attach the graft to the patella with an interference screw or suture anchor.
 Repair the retinaculum with figure-of-eight sutures.
Repair the retinaculum with figure-of-eight sutures.
 Close the wound in layers and apply a controlled-motion knee brace.
Close the wound in layers and apply a controlled-motion knee brace.
Intraarticular Dislocations of the Patella
Intraarticular dislocations of the patella are rare and are of two types. The most common type is a horizontal intraarticular dislocation of the patella with detachment of the quadriceps tendon; the articular surface of the patella is directed toward the tibial articular surface (Fig. 60-3). In the other type, the patella also is dislocated horizontally but its inferior pole is detached from the patellar tendon and the articular surface faces proximally. These dislocations frequently are difficult to reduce by closed methods, and open reduction generally is required, along with repair of the extensor mechanism.
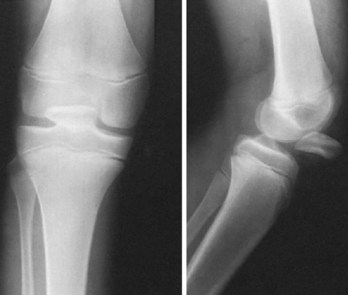
FIGURE 60-3 Intraarticular horizontal dislocation of patella. Quadriceps mechanism usually remains intact.
(From Brady TA, Russell D: Interarticular horizontal dislocation of the patella: a case report, J Bone Joint Surg 47A:1393, 1965.)
Open Reduction and Repair of the Extensor Mechanism
 Through a medial parapatellar incision, expose the dislocated patella, usually found in the intercondylar notch.
Through a medial parapatellar incision, expose the dislocated patella, usually found in the intercondylar notch.
 Replace the patella into its bed in the quadriceps or patellar tendon, and reattach it there with sutures. Placing the sutures through holes drilled in the patella may help secure the repair.
Replace the patella into its bed in the quadriceps or patellar tendon, and reattach it there with sutures. Placing the sutures through holes drilled in the patella may help secure the repair.
 Inspect the knee, and remove any loose osteochondral or cartilaginous fragments.
Inspect the knee, and remove any loose osteochondral or cartilaginous fragments.
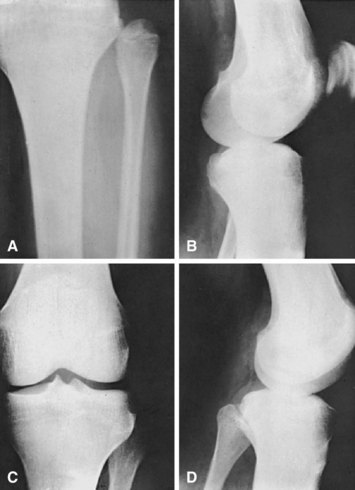
Knee
Dislocation of the knee has been considered a rare injury, but it seems to have increased in frequency over the years. It has been noted that the incidence might be higher than recognized because many knee dislocations are reduced at the scene of the injury without subsequent accurate reporting of this diagnosis (Fig. 60-4).
Knee dislocations usually can be reduced satisfactorily by closed methods. After reduction and in the absence of additional complications, aspiration of the hemarthrosis using sterile technique and immobilizing the knee in full extension are satisfactory temporary treatments. The neurocirculatory status should be checked frequently for 5 to 7 days. A large transarticular pin can be placed through the intercondylar notch of the femur into the intercondylar eminence of the tibia to provide immediate stability for knees that redislocate in a splint or after vascular repair (Fig. 60-5). Transarticular pins have been associated with pin track infection and breakage and should be used with caution. We have found a transarticular pin to be useful when the posterior capsule is completely disrupted, preventing concentric reduction in full extension. The pin is left in place for 4 to 6 weeks, and range of motion is begun. A knee-spanning external fixator can be used in open-knee dislocations with extensive soft tissue injury or in unstable knees after vascular repair. When it is certain that the circulation is not impaired, treatment can be selected for repair of the injured ligaments, as discussed in Chapter 45. Closed reduction may be impossible, however, especially when the dislocation is posterolateral. Blocking of reduction by the interposition of the joint capsule and “buttonholing” of the femoral condyle medially through a tear in the capsule have been reported. A torn tibial collateral ligament or pes anserinus tendon also can block reduction. When an irreducible dislocation is encountered, open reduction through a medial approach often is necessary; however, the approach usually depends on the type of dislocation. The entrapping and torn structures are released and repaired, and the postoperative care is the same as for ligamentous injuries (see Chapter 45).
Several surgeons have advocated early repair of all injured structures in order to obtain satisfactory outcomes. Only fair or poor results can be expected with nonoperative treatment. When open treatment is selected, the surgeon must be prepared to repair structures medially, laterally, anteriorly, and posteriorly as indicated. MRI can be a valuable tool in preoperative planning. Techniques for repair and reconstruction of the ligaments are found in Chapters 45 and 51.
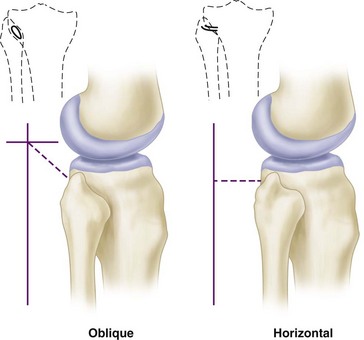
Proximal Tibiofibular Joint
Acute dislocation of the proximal tibiofibular joint is rare (Fig. 60-6). It usually is the result of a twisting trauma and may be seen in association with other injuries to the same extremity. Patients usually present with pain and a prominence in the lateral aspect of the knee. Injuries of the proximal tibiofibular joint frequently are overlooked. Patients with chronic dislocations or subluxation complain of popping and instability, which can be confused with a lateral meniscus injury. The proximal tibiofibular joint can be oblique or horizontal (Fig. 60-7). More motion is possible in horizontal joints, and the relative restriction of motion in oblique joints is presumably the reason why most injuries occur in them.
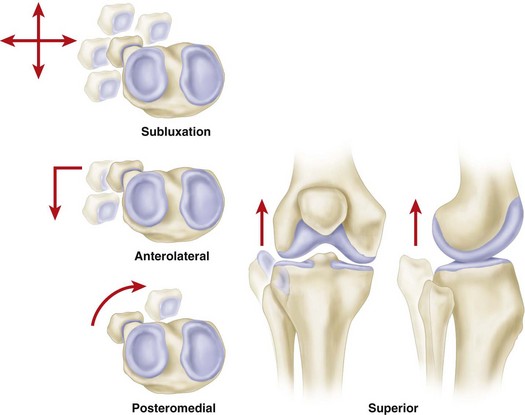
Ogden classified tibiofibular subluxations and dislocations into four types (Fig. 60-8): subluxation and anterolateral, posteromedial, and superior dislocations. Keogh et al. concluded after a cadaver study that the diagnosis of suspected dislocations of the proximal tibiofibular joint was best determined with an axial CT scan (Fig. 60-9).
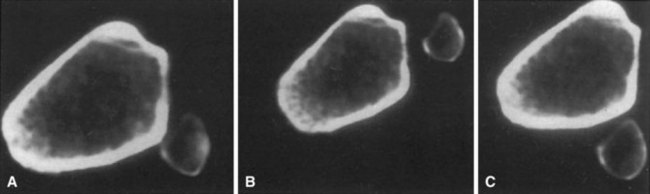
FIGURE 60-9 Axial CT scan of cadaver knee. A, Anatomical. B, Dislocated anteriorly. C, Dislocated posteriorly.
(From Keogh P, Masterson E, Murphy B, et al: The role of radiography and computed tomography in the diagnosis of acute dislocation of the proximal tibiofibular joint, Br J Radiol 66:108, 1993.)
Anterolateral dislocations (see Fig. 60-6) were the most common proximal tibiofibular dislocations in Ogden’s series. They usually were treated successfully by closed methods.
Hip
Hip dislocations are classified according to the position of the femoral head in relation to the acetabulum and according to associated fractures of the acetabulum and proximal femur. Posterior dislocations have been classified by Thompson and Epstein into five types: type I, with or without a minor fracture; type II, with a large single fracture of the posterior acetabular rim; type III, with a comminuted fracture of the rim of the acetabulum, with or without a major fragment; type IV, with fracture of the acetabular rim and floor; and type V, with fracture of the femoral head. Types II through IV with significant associated acetabular fractures are discussed in Chapter 56, and femoral head fractures are discussed in Chapter 55
Anterior dislocations also have been classified by Epstein as follows:
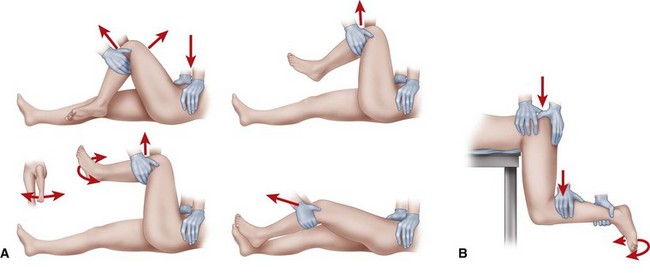
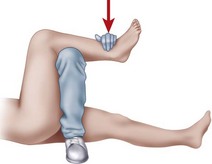
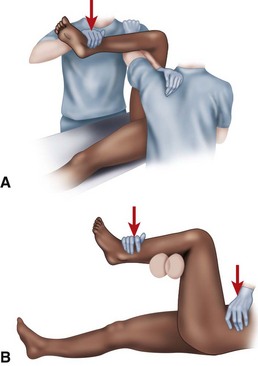
The following guidelines for treatment refer to hip dislocations without significant associated femoral head or acetabular fractures (Thompson and Epstein type I). Several methods of closed reduction have been used successfully, all of which generally consist of re-creating the injurious deforming force (for posterior dislocations—flexion, adduction, and internal rotation; for anterior dislocations—abduction and external rotation in extension). Traction in line with the affected femur and small amounts of rotation and abduction and adduction complete the reduction. The Allis maneuver is performed for posterior dislocations as previously described with the patient supine, whereas the Stimson maneuver is similarly performed with the patient prone (Fig. 60-11). Other reduction techniques involve levering the affected limb at the ankle over a fulcrum (Figs. 60-12 and 60-13). Regardless of the method chosen, only two or three attempts should be made at closed reduction. Multiple, increasingly forcible attempts at reduction could lead to an iatrogenic femoral head, neck, or shaft fracture or cartilaginous injury to the femoral head or acetabulum.
Open Reduction of Hip Dislocation
 Regardless of the direction of the dislocation, when the approach has been made, assess the capsule first.
Regardless of the direction of the dislocation, when the approach has been made, assess the capsule first.
 If the femoral head is buttonholed, extend the traumatic capsulotomy in a T-shaped fashion along the acetabular rim, carefully preserving the labrum, if possible.
If the femoral head is buttonholed, extend the traumatic capsulotomy in a T-shaped fashion along the acetabular rim, carefully preserving the labrum, if possible.
 Inspect the joint for intervening capsule, labrum, piriformis muscle, or bony fragments.
Inspect the joint for intervening capsule, labrum, piriformis muscle, or bony fragments.
 If necessary, retract or distract the hip manually or with skeletal traction applied through a fracture table or femoral distractor for better assessment of the joint.
If necessary, retract or distract the hip manually or with skeletal traction applied through a fracture table or femoral distractor for better assessment of the joint.
 When the joint has been cleared of debris, reduce the hip joint by releasing the traction.
When the joint has been cleared of debris, reduce the hip joint by releasing the traction.
 Repair the capsule along with the labrum.
Repair the capsule along with the labrum.
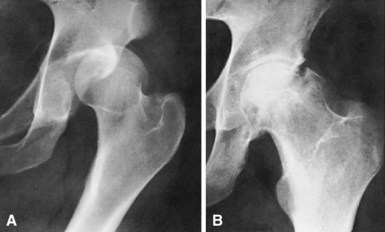
Complications
Osteonecrosis has been reported to occur in 4% to 22% of hip dislocations without associated femoral head or acetabular fracture (Fig. 60-14). Time to reduction plays a role in the development of this complication because multiple studies have shown a direct correlation between the time to reduction and the prevalence of osteonecrosis. In the best of circumstances, a percentage of patients develop avascular changes despite prompt reduction of a dislocated hip. Patients with posterior dislocations and multiple injuries are apparently at increased risk for the development of osteonecrosis. Most patients who develop osteonecrosis have symptoms within 2 years of injury, although late cases of osteonecrosis with radiographic changes delayed 5 years have been reported.
Pubic Symphysis and Sacroiliac Joints
Dislocations involving the symphysis pubis and sacroiliac joints occur only with high-energy trauma. Considerable force is required to overcome the complex ligamentous structures that provide stability to the adult pelvis. The relevant anatomy and appropriate diagnostic and treatment algorithms are included in Chapter 56.