Fig. 22.1
Posttraumatic osteolysis of the distal clavicle on the right side

Fig. 22.2
Zanca view and scapular Y view showing subtle erosions along the subchondral bone of distal clavicle

Fig. 22.3
Distal clavicular osteolysis after fixation of fracture of distal clavicle
22.4.2 Scintigraphy
Early in the course of DCO, Tc-99 scintigraphy will show marked increase in uptake in angiographic and blood pool phases in the distal clavicle. In addition there will be increased focal distal clavicular uptake in the delayed phase.
At times, there is also increased activity in the adjacent acromion [1]. But the difficulty with this bone scan is high sensitivity and very low specificity, which needs to be interpreted in the background of clinical findings. Some critics have pointed out that the metaphyseal end of all long bones demonstrates an increase in the uptake on scintigraphy, and the clavicle is no exception. A further increase in the uptake of that area can represent a simple increase in bone turnover, due to the stress applied by young individuals, and is a normal phenomenon [23]. It may be related to an increased blood flow and blood pooling.
22.4.3 Magnetic Resonance Imaging (MRI)
MRI demonstrates increased signal intensity associated with T2-weighted images, most notably on the fluid-sensitive STIR and fat-suppressed spin echo on the T2-weighted sequences.
Bone marrow edema in the distal clavicle is the most common manifestation of DCO and it has a high correlation to patient symptoms [12], but edema may also be seen in the acromion. Other common findings are osseous fragments and osseous irregularity [12], bulbous prominence of AC joint capsule, minimal joint effusion, and intra-articular bone fragmentation [12].
Undisplaced subchondral fracture in the distal clavicle (hypointense subchondral line centered within edema of distal clavicle) [24] is the most recently established finding (Fig. 22.4).
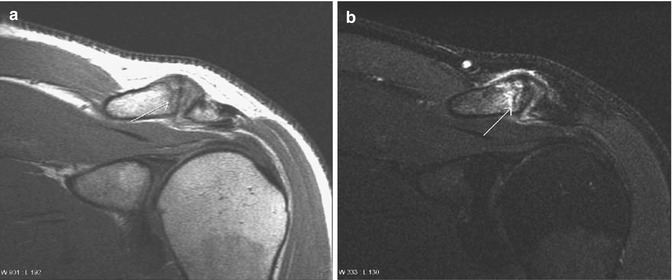
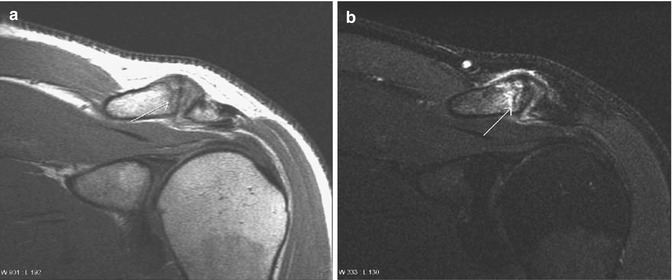
Fig. 22.4
Coronal oblique proton density (a) and fat-suppressed intermediate (b) MR images show extensive edema in the distal clavicle. Note the clearly visualized hypointense line (arrow), centered within the edema in the distal clavicle and consistent with a subchondral fracture. Also, there is minimal edema in the tip of the acromion. Fluid is present in the acromioclavicular joint
22.4.4 Ultrasound- or CT-Guided Injections of the AC Joint
Injection of Xylocaine or Sensorcaine (local anesthetics) into the AC joint may temporarily relieve the pain and can be used as a diagnostic tool. The greatest benefit may be that a positive temporary relief of pain can be seen as a diagnostic tool for confirming that the pain is indeed localized in the AC joint. Intra-articular corticosteroids with or without Hyaluron can be considered for short-term symptom relief, if patients do not respond to conservative treatment for 3 months [6]. However, they provide little long-term relief. Image-guided injection allows location of the best point on the skin, appropriate depth and needle inclination, and correct positioning of the needle tip [6].
22.5 Disease-Specific Clinical Pathology
22.5.1 Differential Diagnosis
Although DCO is a benign condition and straightforward to diagnose, some of the more important conditions should be excluded at the time of diagnosis. These include glenohumeral and subacromial injuries, multiple myeloma, rheumatoid arthritis, hyperparathyroidism, gout, scleroderma, septic or tubercular arthritis, osteoarthrosis of the AC joint, corticosteroid-induced arthropathy, primary and metastatic neoplasms, massive essential osteolysis (Gorham’s disease), rickets, progeria, eosinophilic granuloma, and cleidocranial dysplasia [25].
The diagnosis of DCO is usually made by history, physical examination, and plain radiographs.
Bone scans, MRI, and differential injections are helpful in patients with equivocal findings or other shoulder problems [21].
22.5.2 Natural History
The osteolytic process is variable in time but consistent in evolution. Lytic phase may continue for 12–18 months, resulting in 0.5–3 cm of bone loss from the distal clavicle and rarely the acromial end. Calcification of ligaments and subperiosteal reaction may occur. During the reparative phase, the distal clavicle becomes smooth and tapered with reconstitution of cortices but the AC joint remains permanently widened [17, 26].
DCO is a self-limiting disorder, with resolution within 1–2 years with activity modification. Although most patients respond to conservative management, with relief of symptoms along with partial or complete osseous restoration of the clavicle, symptoms often return with resumption of previous activity level [27]. There will be gradual cessation of symptoms from active lytic phase to burnt-out phase [17].
22.6 Treatment Options
Treatment methods for DCO are generally driven by symptomatology and disease stage. However, controversy does exist on the course of the disease, with some authors concluding that insufficient treatment predisposes and exaggerates the osteolytic process, whereas others believe that the eventual severity of bony damage is predetermined and directly related to the severity of the inciting event [16, 25].
22.6.1 Nonsurgical Treatment
Early diagnosis and treatment have been shown to successfully decrease clinical symptoms, halt the osteolysis process in some cases, and result in varying degrees of reversal and healing. A delayed diagnosis typically results in a permanently widened AC joint with varying degrees of mechanical dysfunction and pain [26].
Avoidance of provocative maneuvers, modification of weight-training techniques and behavior, immobilization of the affected extremity, cryotherapy, and nonsteroidal anti-inflammatory drugs (NSAIDs) constitute the basis of initial treatment. Corticosteroid injections have been used with limited success. Haupt has suggested several modifications in the young athlete’s weight-training program [2]. Most of the specific modifications of weight-training techniques involve narrowing the hand spacing on the barbell (less than 1.5 times the biacromial width) and controlling the descent phase of the bench press to end approximately 4–6 cm above the anterior chest. The narrower handgrip allows the athlete to make adjustments to the component angles of the bench press by maintaining shoulder abduction at less than 45° and shoulder extension at less than 15°. This then decreases the compressive force on the distal clavicle [28]. Haupt HA promotes a routine program in which the bench press, dips, and push-ups are eliminated. Alternative recommendations are the cable crossover, dumbbell decline press, and incline press with straight bar [2]. All pressing motions are performed with a narrow grip, no greater than 1.5 times the biacromial width.
The power clean, although a rather full-body functional exercise, does place significant stress on the AC joint during the “racking” phase. In this part of the exercise, the shoulders are shrugged, the elbows flexed, and then the shoulders are abducted to bring the bar up into a “racked” position. If the athlete is suffering from an AC joint injury, the power clean should be modified to allow only the pulling portion of the lift without racking the bar—an exercise termed a “power clean high pull” or “power pull.” The key to this motion is that the athlete still gains a lower extremity benefit but avoids additional AC trauma that can be associated with a mistimed lift. The preferred way to perform the exercise is to adjust the exercise machine or starting position so that the elbows are even with or above the frontal plane when beginning the lift and during repetitions (honing technique) [28].
Dietary supplementation of multiminerals, glucosamine, and chondroitin sulfate has also been recommended [26]. Alendronate (bisphosphonate) along with other conservative modalities [29] has been tried in a case report with successful resolution of symptoms and imaging findings. Conservative treatment options should be used as long as the patient will comply, with consideration of the patient’s symptoms and functional status [26].
CT-guided injections of the AC joint allow for selection of location of best access points on the skin, appropriate depth, and inclination of the needle to inject local anesthetic mixed with depot preparations of corticosteroids. Conservative care stresses the use of NSAID and cryotherapy of the AC joint after all workouts [2]. In a sense, continued physical activity and pathogenesis will result in a “self-surgery”; that is, the clavicle will be resected on its own.
Appropriate educations should be guided to at-risk individuals like collision sports athletes and contact sports athletes; using proper techniques when falling, tackling and weight-lifting. Also it is important to ensure proper use and fit of protective equipment. Finally the rehabilitation program should be completed with strength and endurance training for the rotator cuff muscles, deltoid, trapezius, and other scapulothoracic muscles.
Even immediate immobilization after the injury in traumatic DCO does not seem to decrease the early manifestations of osteolysis. Early treatment may, however, decrease the total amount of bone loss, help decrease the time of the lytic phase, initiate repair, and decrease clinical symptoms [30].
22.6.2 Surgical Treatment
General indications for surgery include recalcitrant and isolated acromioclavicular joint pain with point tenderness of the AC joint, evident abnormal signs with AC joint imaging, lack of response to conservative treatment, and an unwillingness to give up or modify weight or sports training or manual labor [1, 5, 16]. Distal clavicle resection (DCR) is the most common type of surgery for DCO. Once patients have been selected strictly for surgery based on appropriate indications, decision must be made whether to perform open DCR or arthroscopic DCR and how much of the distal clavicle should be resected.
Both open and arthroscopic distal clavicle resection have been successful in alleviating pain and returning patients to previous activity levels [1, 31]. While Cahill et al. reported excellent results with an open approach resecting 1–2 cm of the distal clavicle, where 37 of 40 patients returned to weight training or competitive sports [1], Ague et al. reported that arthroscopic resection of only 4 mm was effective [21]. Arthroscopic DCR is a minimally invasive procedure with maximum visualization, associated with less surgical morbidity and early rehabilitation; associated intra-articular injuries can be diagnosed and treated simultaneously.
It can be difficult to determine whether pain after a history of trauma to the acromioclavicular joint is caused by osteolysis of the distal clavicle or by subtle instability. Therefore, a careful assessment of acromioclavicular stability is mandatory before recommending surgery. This should include translation testing of the distal clavicle in the anteroposterior and superoinferior planes, as well as careful scrutiny of preoperative radiographs for evidence of prior low-grade acromioclavicular separation. In this setting, arthroscopic distal clavicle resection is a reasonable initial treatment option with low morbidity. However, the patient should be warned that open stabilization of the acromioclavicular joint may be necessary should pain continue after arthroscopic resection of the distal clavicle.
22.6.2.1 Open DCR
The rationale of the open DCR is that the pathological articular surfaces can be resected under direct vision in order to create a wide enough margin to prevent further acromion abutment on the clavicle. Either of the two skin incisions can be used, the strap and the horizontal [2]. The junction of the deltoid and trapezius fascia must be split to provide proper exposure of the AC joint. Classic Mumford procedure is carried out; that is, 1–2 cm of the distal clavicle as well as the acromion is resected. The inferior AC joint capsule can be incorporated into the repair of the deltoid and trapezius fascia in order to eliminate any potential dead space. Flatow and colleagues support the transferring of the coracoacromial ligament to cover the outer end of the clavicle in order to provide additional stability to the weight lifter [31].
The majority of follow-up studies have reported positive results when considering pain as a major indicator of success. Slawski and Cahill treated 12 active weight lifters and two manual laborers with open DCR. They reported that all patients returned to full sports activity and employment by an average of 9 weeks postoperatively and ultimately returned to a level of competition or productivity as good as or better than when they had been symptomatic. There were eight excellent and nine good results based on UCLA Shoulder Rating Scale [10].
Although the open procedure has been shown to produce good to excellent results clinically, the extensive tissue damage required to gain access to the AC joint has been linked to resulting muscle weakness [5, 32, 33] and disruption of the AC ligaments with abutment of the distal clavicle stump on the acromion with arm motion and instability of the AC joint with limited range of motion [31].
22.6.2.2 Arthroscopic DCR
Due to very obvious advantages of arthroscopic shoulder surgeries, it is not wise to compare arthroscopic DCR with open DCR and it is like comparing apples to oranges. Evidence has shown that 0.5–1.0 cm arthroscopic resections are comparable to the 1.5–2.0 cm resections performed during an open procedure [5, 34], suggesting optimal bone removal during arthroscopic DCR. There are two approaches—indirect (subacromial) or direct (superior). Both the approaches offer the advantages of decreased morbidity, with fewer postoperative restrictions on motion, earlier return to normal activity, and improved cosmesis. These early results are encouraging and warrant further examination of the treatment of this disease entity, an entity with a low prevalence as an isolated condition and which perhaps is becoming more prevalent in our society [21].
Subacromial (Indirect) Approach
The subacromial approach, first described by Ellman and Esch, preserves the superior AC joint ligaments and provides less chance for postoperative horizontal instability. It can be done in either lateral decubitus or beach chair sitting positions, depending on training and comfort of the surgeon. The technique uses anterior instrumental, posterior scope, and lateral inflow portals. A shaver is used to debride initially any obscuring bursa. Electrocautery is used to clearly demarcate the distal clavicle and minimize bleeding. Great care should be used not to disrupt the supporting ligaments and capsule. Once good visualization is obtained, a burr (usually 5–6 mm) is used through the anterior portal to clear any remaining osteophytes and to resect the distal clavicle from anterior to posterior. Modifications of this technique include burring from both the posterior and the lateral portals, as well as visualization through the three standard portals. Bone depth can be gauged using the known diameter of a burr; however, Tolin and Snyder recommend the routine use of two needles to demarcate the orientation of the joint, as well as to gauge the amount of bone resected, by measuring the distance between the two needles on the skin. Although some investigators recommend resecting a small portion of the medial acromion, most find it unnecessary. To aid in resection of the superior portion of the distal clavicle, manual pressure can be applied to bring the clavicle into the subacromial space. It has been suggested that failure of this technique is not due to the amount of bone removed but rather the result of uneven resection or disruption of the AC ligaments. This would lead to translation of the clavicle, resulting in an abutment on the acromion and cause recurring symptoms [35, 36]. This problem often happens after aggressive arthroscopic resection when care is not taken to preserve the stabilizing ligamentous envelope. Morrison and colleagues recommend beveling the posterior edge of the distal clavicle if this instability is recognized intraoperatively to avoid the resultant painful impingement [37].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








