Acetabular fractures
INTRODUCTION
Background
Fractures of the acetabulum in elderly patients are becoming increasingly common due to a progressively ageing population. Elderly patients represent the fastest growing subset of the UK population as a consequence of improved healthcare, better living standards and greater general health awareness.1 As well as an increasing life expectancy, these patients remain more active and have greater physical demands. Acetabular fractures in this group of patients are challenging to manage as they frequently consist of complex fracture patterns in the presence of reduced bone mineral density, pre-existing hip disease and medical comorbidities. Due to greater expectations from treatment, there is a higher demand on healthcare resources with clear socioeconomic implications. Whereas older age once represented a contraindication to surgical treatment, an increasingly active and socially demanding elderly population has caused a paradigm shift in practice towards operative management of these complex injuries. Conservative management traditionally involves prolonged bed rest, which is strongly associated with higher rates of mortality and morbidity due to the risk of nosocomial infection, pressure sores and venous thromboembolism.2 In addition, recent advances in surgical techniques and implant technology make operative treatment a more feasible option with more predictable outcomes.
Anatomy
The word ‘acetabulum’ is etymologically derived from Latin and literally means ‘vinegar cup’. It forms the proximal part of the hip girdle and articulates with the head of the femur within a synovial ball-and-socket joint. It is formed by a confluence of the ilium, ischium and pubis which make up the innominate bone. It is further divided into the anterior and posterior columns which have an inverted ‘Y’ configuration (Figure 33.1). The anterior column is comprised of the anterior half of the ilium superiorly and extends to the pubic symphysis inferiorly. The posterior column is comprised of the posterior half of the ilium superiorly and extends to the ischium inferiorly. The cotyloid fossa is a recessed non-articular part of the floor of the acetabulum which provides the attachment of the ligamentum teres. The medial wall of the acetabulum is known as the quadrilateral plate, which is thinner than the superior weight-bearing surface and is therefore more susceptible to fracture in the elderly population. A thick labrum normally circumscribes the edge of the acetabulum and contributes to stability of the hip joint. Running inferiorly is the transverse acetabular ligament which acts as a tension band during loading of the hip joint.3 The acetabulum has a natural inclination of 40–48 degrees and is anteverted by 18–21 degrees. The vascular supply is provided by the corona mortis which is an anastomosis of the external iliac and internal iliac arteries via the epigastric and obturator arteries, respectively.
Mechanism of injury
Acetabular fractures have a bimodal distribution. High energy blunt trauma accounts for the majority of fractures in young patients, while low energy trauma is primarily responsible for these injuries in elderly patients. These most often occur following a fall onto the side of the hip with forces transmitted via the greater trochanter through the femoral neck. These forces are then conveyed to the acetabulum usually leading to atypical fracture patterns. While simple falls from standing height are the most common presentation in older patients, fractures of the acetabulum may also be the result of high energy trauma, for example, road traffic accidents. These may involve concomitant injures to the ipsilateral intertrochanteric region, femoral neck or pelvis. In the absence of trauma, insufficiency fractures of the acetabulum may occur in the presence of reduced bone mineral density and may be difficult to diagnose. A high index of suspicion can lead to an early diagnosis and improve outcomes in these patients who can usually be successfully managed conservatively.4 Pathological fractures of the acetabulum most often occur in the presence of metastatic deposits in this age group and can be extremely disabling.5 A full narrative on the management of pathological fractures is outside the scope of this chapter but it is important to treat these patients with a multidisciplinary team approach involving orthopaedic bone tumour surgeons, oncologists, occupational therapists and physiotherapists in order to provide a full assessment of treatment goals and reconstructive options.
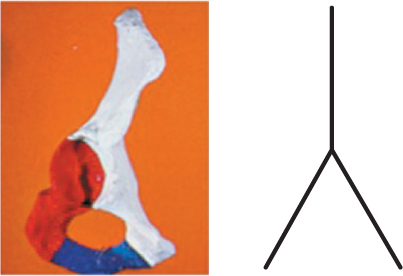
Figure 33.1 Inverted Y representing column theory. Red: posterior column; white: anterior column.
Aims and objectives
Following clinical and radiological assessment, certain factors must be considered before selecting an appropriate management strategy. These include analysis of fracture displacement and available bone stock for reconstructive surgery as well as a thorough assessment of the patient’s cognitive status and functional demands. Due to the great variability in patient characteristics and expectations from treatment, the management plan must be individualized according to the patient’s personal requirements. This can be challenging as many elderly patients have complex medical comorbidities and social needs. In addition, certain fracture characteristics specific to the elderly population can make surgical management extremely demanding. The aim of this chapter is to provide an overview of the epidemiology, classification, radiological assessment and treatment of acetabular fractures in the geriatric population.
EPIDEMIOLOGY
The epidemiology of acetabular fractures has rarely been investigated and is therefore difficult to accurately describe. Accounting for all age groups, the annual incidence of acetabular fractures in the UK population has been estimated by Laird and Keating to be three patients per 100,000 per year.6 The dataset in this epidemiological study involved a total of 351 patients over a 16-year period of whom 231 (65.8%) were males and 120 (34.2%) were females. Over time, there was an increase in the mean age of the patients from 46.8 years to 53.7 years but this did not reach statistical significance. An increase in simple falls as the mechanism of injury was also observed and this may have been a due to the increasing mean age at which these injuries were seen. There was also an increase in the proportion of females with these injuries and importantly, there was a significant reduction in mortality.
A prospective epidemiological database study of 1,309 displaced acetabular fractures gathered over 27 years in the United States revealed that 235 (17.9%) patients were aged over 60 years.7 During the first half of the study period, 62 (10%) patients were over 60 years while during the second half, 174 (24%) patients were in this age group. This reflects a 2.4-fold increase in the prevalence of acetabular fractures in elderly patients. In this group, simple low energy falls were the mechanism of injury in 117 (49.8%) patients while high energy injuries, such as road traffic accidents, were responsible for injury in 88 (37.4%) patients. It is noteworthy that while acetabular fractures were associated with other injuries, such as chest and abdominal injuries, in 527 (49.1%) patients less than 60 years of age, only 70 (29.8%) of the older patient group sustained a concurrent injury. This may be explained by the fact that elderly patients with acetabular fractures usually have low energy injuries and are therefore less likely to suffer from polytrauma. Of those who did present with a concurrent injury, older patients were more likely to suffer coexisting limb injuries rather than the visceral injuries seen in their younger counterparts.
CLASSIFICATION
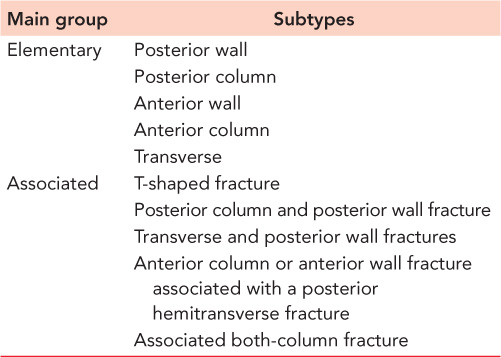
Letournel classification
Numerous classification systems have been used to describe fractures of the acetabulum but the most well known is that of Letournel.8,9 This anatomical classification is based on the radiographic evaluation of the anterior and posterior columns of the acetabulum. It is useful in describing and communicating fracture patterns and also aids in planning the surgical approach. Multiplanar computed tomography (CT) scanning offers substantially improved interobserver agreement when compared to plain radiography.10 According to this system, fractures can be divided into two main groups with each group further divided into five subtypes (Table 33.1). In general, the position of the femoral head at the time of impact dictates the type of fracture. If the hip is in a position of external rotation then the anterior column is likely to be injured, while in internal rotation an injury to the posterior column is more likely to occur. In the abducted position a low transverse fracture is more common, while in the adducted position a high transverse fracture is more likely to occur. With respect to the so-called associated fracture patterns, it is important to understand the key principles behind their nomenclature. If both columns are fractured, this is known as a transverse fracture (separating the innominate bone into two segments, that is, superior iliac and inferior ischiopubic) but if both columns are fractured and separated from one another, this is called a T-shaped fracture. This is in contrast to the complex both-column fracture in which both columns are fractured and separated from each other but there is also dissociation of the articular surface from the innominate bone and central dislocation of the femoral head. A radiological analysis of 647 acetabular fractures revealed that posterior wall fractures (24.2%) were the most common of the elementary patterns while transverse and posterior wall fractures (20.7%) and both-column fractures (20.2%) were the most common of the associated patterns.9
Table 33.1 Letournel classification
AO comprehensive classification
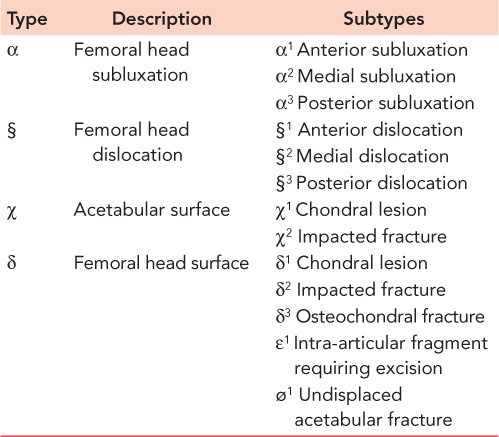
In order to standardize the nomenclature regarding acetabular fractures and introduce factors which could influence surgical decision-making, Tile modified this system to include a number of prognostic indicators such as subluxation, dislocation, intra-articular comminution and articular surface involvement. In this description, three main groups of fracture are categorized alphabetically according to the AO comprehensive classification (Table 33.2).11 Type A injuries are partial articular fractures which involve a single column and are further subdivided into posterior wall fractures, posterior column fractures and anterior wall or anterior column fractures. Type B injuries are also partial articular fractures but these involve both columns and are further subdivided into transverse fractures, T-shaped fractures and anterior column plus posterior hemitransverse fractures. Type C injuries are complete articular fractures with separation of the articular surface and are analogous to the both-column fractures described by Letournel. These are further subdivided into a high type, a low type and a type which involves the sacroiliac joint. Further fracture characteristics can be added as qualifiers in order to guide prognosis (Table 33.3).
Table 33.2 AO comprehensive classification
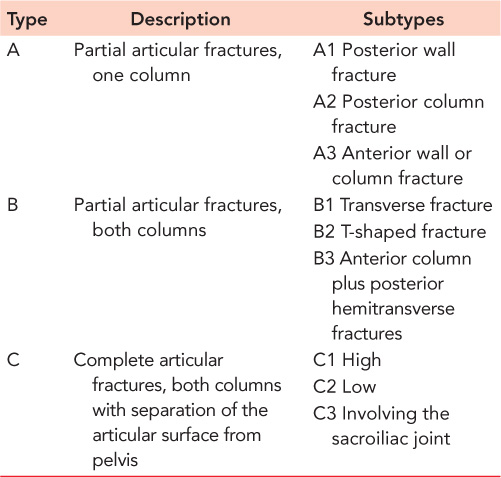
Table 33.3 Qualifiers of AO classification
Special considerations in the elderly
The fracture patterns described by both Letournel and Tile typically relate to younger patients who have been involved in high energy trauma. Elderly patients with osteoporotic bone are more likely to present with atypical fracture patterns which do not necessarily conform to either of the described classification systems. In their study of 1309 acetabular fractures, Ferguson et al. reported that displaced fractures of the anterior column were significantly more common in the elderly population compared with younger patients (64% vs 43%).7 Overall, elementary fractures were less common than associated fractures with complex both-column fractures occurring most frequently. Features specific to the elderly population were a separate quadrilateral plate component and roof impaction in the anterior fractures and comminution and marginal impaction in posterior wall fractures. Similarly, Ochs et al. found in a large trauma database study that there were more anterior wall, anterior column and anterior column with posterior hemitransverse fracture types in patients over 60 years of age.12 In addition, central fracture-dislocations of the femoral head with medial displacement of the quadrilateral plate are more common in the elderly population and are frequently encountered in combination with associated fracture types (Figure 33.2).13

Figure 33.2 Central fracture-dislocation of the left femoral head with quadrilateral plate injury and articular impaction.
These observations can be explained by the presence of osteoporotic bone in the elderly cohort. As the severity of osteoporosis increases, characteristics such as comminution, impaction and loss of articular cartilage are more commonly encountered. These features are recognized as being poor prognostic indicators and correlate with worse clinical outcomes. Many of the complex fracture patterns frequently seen in the geriatric population are not easily defined by any current classification system. However, in the presence of good bone quality, more typical fracture patterns as seen in younger patients can be expected and therefore, the Letournel system can be reliably utilized.
RADIOLOGY
The diagnosis of fractures of the acetabulum is primarily radiological as elderly patients who present following a fall from standing height are at risk of multiple fractures of the pelvis and proximal femur. Therefore, plain radiography including an initial anteroposterior view of the pelvis and affected hip is mandatory. A lateral view of the proximal femur should also be taken in order to avoid overlooking a concurrent femoral neck fracture. Inlet and outlet pelvic views are also warranted if pelvic ring or sacral injuries are suspected. There are six important landmarks on the anteroposterior radiograph of the pelvis that are relevant to acetabular anatomy. These help identify the fracture lines and guide classification (Figure 33.3). They are:
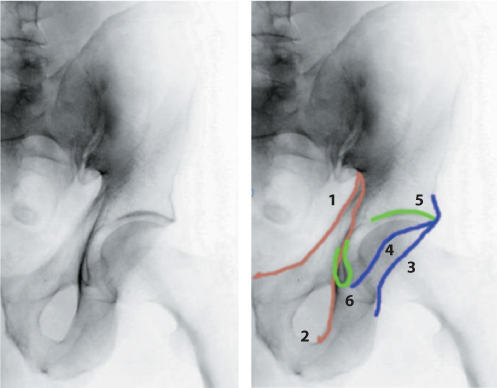
Figure 33.3 Radiographic landmarks.
The iliopectineal line (1) – this represents the arcuate line and runs along the inner aspect of the pelvic brim from the greater sciatic notch to the pubic symphysis. A break in this line signifies a fracture to the anterior column.
The ilioischial line (2) – also known as Kohler’s line, this is formed by the posterior aspect of the quadrilateral surface of the ilium and extends from the greater sciatic notch vertically down to the inner aspect of the obturator foramen. A break in this line represents a fracture to the posterior column.
The posterior and anterior walls (3 and 4, respectively) – these are usually seen with the anterior wall superimposed over the posterior wall which projects more laterally due to normal acetabular anteversion. An abnormality of either landmark indicates a wall fracture. If the lines demarcating the edge of the two walls ‘cross-over’ then this may indicate a retroverted acetabulum due to pre-existing hip dysplasia.
The roof of the acetabulum (5) – also known as the dome or ‘sourcile’, this being French for ‘eyebrow’. This radiographic marker represents the subchondral area of the weight-bearing portion of the superior acetabulum. A roof arc angle of greater than 46 degrees confirms the presence of an intact weight-bearing surface.14
The radiographic teardrop (6) – this is formed by a condensation of the innominate bone at the inferior end of the acetabulum and is normally U shaped. It consists of medial and lateral limbs. The medial limb is formed by the anteroinferior portion of the quadrilateral plate and is continuous with the ilioischial line. The lateral limb is continuous with the floor of the acetabulum superiorly and represents the inferior aspect of the anterior wall.

Figure 33.4 Anteroposterior view of a transverse left acetabular fracture in an elderly patient.

Figure 33.5 Obturator oblique view of a transverse left acetabular fracture.
Judet et al. also recommended the use of additional obturator and iliac oblique views following identification of an acetabular fracture on the initial anteroposterior radiograph (Figure 33.4).8 The obturator oblique view (Figure 33.5) is taken by rolling the patient into 45 degrees of internal rotation thereby raising the injured side. This shows the obturator foramen en face and allows clearer imaging of the anterior column, the posterior wall and part of the iliac wing. The iliac oblique view (Figure 33.6) is taken by rolling the patient into 45 degrees of external rotation thereby raising the uninjured side. This shows the iliac wing en face and allows clearer imaging of the posterior column and the anterior wall. By convention, the beam is centred on the pubic symphysis so that both acetabuli can be visualized. Therefore, an obturator oblique view of one acetabulum will also show an iliac oblique view of the contralateral side on the same film and vice versa. Careful evaluation of all three of these acetabular views can help to identify the bony fragments and classify the fracture pattern. An important feature is the ‘spur sign’ (Figure 33.7) which is pathognomonic of a both-column fracture with associated medial displacement of the hip joint and is classically seen on the obturator oblique view.15 A fragment of ilium remains attached to the sacroiliac joint but is separated from the fractured acetabulum resulting in a characteristic appearance. The ‘gull sign’ (Figure 33.8) is a double density also usually seen on plain radiography and represents marginal impaction of the superomedial joint surface. This sign has been associated with poorer outcomes following internal fixation of acetabular fractures in elderly patients.16

Figure 33.6 Iliac oblique view of a transverse left acetabular fracture.
Further imaging in the form of CT scanning with 2–3 mm intervals is nearly always recommended, but especially when operative management of displaced fractures is being considered. Not only does this provide more detail with respect to fracture anatomy, but it also offers multiplanar imaging which can be extremely useful when planning surgical reconstruction. Furthermore, small intra-articular fragments can be more accurately identified and this may highlight the need for operative intervention. Due to the additional detail provided, other critical features can be defined and assessed with greater precision, for example, extent of fracture comminution, available bone stock, marginal impaction of the articular surface and concurrent occult fractures of the pelvis and proximal femur. Where possible, three-dimensional reformatting is recommended and can assist in preoperative planning for internal fixation. Unless pathological fractures of the acetabulum or pelvic girdle are suspected, magnetic resonance imaging is not routinely advocated in the primary assessment of fractures of the acetabulum. However, it may have a role in detecting insufficiency fractures in the presence of normal plain radiographs.
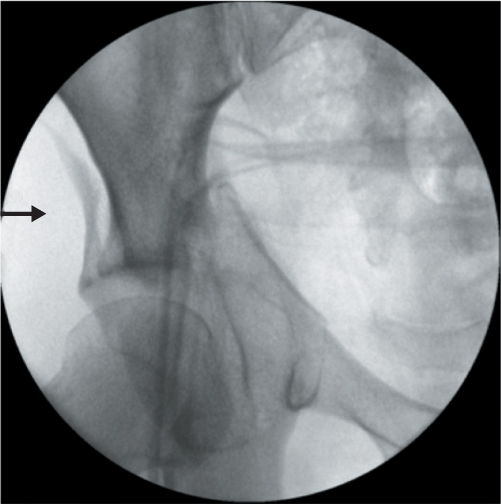
Figure 33.7 Spur sign.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








