Fractures and Related Conditions: Fundamentals
DIANE M. KOSHIMUNE, FRANK A. SPINOSA, ROBIN C. ROSS, AND ROBERT A. CHRISTMAN
Based on the history and physical exam, if an underlying fracture is suspected, radiography may be an excellent resource to rule in or out osseous pathology. The clinical information can help to narrow the structures to be examined. Additionally, information regarding the mechanism of injury, if applicable, can specify further the type of pattern you would expect to see.
Ordering the appropriate views to show the specific structures in question is particularly important. At least two, occasionally three, views may be necessary to show the level of angulation or displacement that is present in different planes. (See Chapter 10 for more information on selecting the best views to see a particular osseous site.) Occasionally, radiography may be unable to reveal occult or hard to visualize fractures. Proceeding to additional advanced imaging studies such as computed tomography (CT), magnetic resonance imaging (MRI), or bone scintigraphy may be necessary.1–5
Recognizing a break (or discontinuity) in the osseous structure is the first step; however, the ability to describe the fracture pattern will help in documentation, treatment planning, and discussions with other practitioners. Descriptive information can offer very different impressions of the presentation. For example, “fracture of the hallux” focuses attention to the location when viewing the image, but does not describe the nature of the fracture pattern. Noting directionality of the fracture line, displacement, and angulation of the distal fragment and whether or not there is articular involvement, dislocation, or fragmentation can paint a very specific picture without viewing the image itself. By using appropriate terminology, a great amount of information can be imparted accurately and efficiently.
FRACTURE TERMINOLOGY
A fracture pattern may be described as open or closed. This designation indicates whether or not a bone fragment has violated the overlying soft tissue envelope, lacerating the soft tissue and protruding through the skin. An open fracture is considered a surgical emergency, requiring rapid response to irrigate the involved tissues and, if possible, reapproximate the fracture ends.2,5–7 In 1976, Gustilo and Anderson8 published a retrospective study involving open tibial fractures, providing a framework for classifying the different patterns and recommending treatment protocols, including antibiotic coverage. Occasionally, the terms compound and simple fracture are used to describe the same relationship, whether or not the underlying bony structures are exposed through the skin. It should be noted that this designation of open or closed is a clinical one and will not usually appear in a radiographic report.9
A simple fracture may be defined as a closed fracture, but the term also indicates that there is only a singular fracture line, creating two distinct fracture segments (Figure 15-1). This is in contrast to a comminuted fracture, which involves two or more fracture lines in the same bone resulting in three or more fracture segments (Figure 15-2).2,6 Harkess7 suggests that high-velocity missiles create a significant disruption to the soft tissue and underlying bone resulting in a comminuted pattern. Additionally, the fractured particles may become secondary missiles, further disrupting the anatomy.8 If a triangular fracture fragment results from a comminuted fracture, this is referred to as a butterfly fragment (Figure 15-3A).4,6 In contrast, if two fracture lines create a discrete or isolated segment along the shaft of a long bone, this is referred to as a segmental fracture (Figure 15-3B).4,6,9

FIGURE 15-1. Simple fracture, third metatarsal, directed transversely at the junction between the middle and distal thirds of the shaft. The distal segment relative to the proximal is slightly displaced medially and angulated laterally.

FIGURE 15-2. Comminuted fracture, fifth metatarsal distal half diaphysis. At least four fracture segments are present.
A fracture can be complete or incomplete. A complete fracture involves all cortices of the bone, whereas an incomplete fracture does not. Incomplete fractures are typically stable and often occur in children or in individuals who have “softer” bone as a result of disease (i.e., Paget disease or osteomalacia). Common patterns of incomplete fractures are greenstick and torus fractures. A greenstick fracture results in opening of one cortex on the convex side due to angular stress while maintaining the integrity of the remaining cortex (Figure 15-4). A torus fracture is a compression type fracture where the cortex appears to “buckle” on the concave side in response to angular stress (Figure 15-5).2,3,5,6
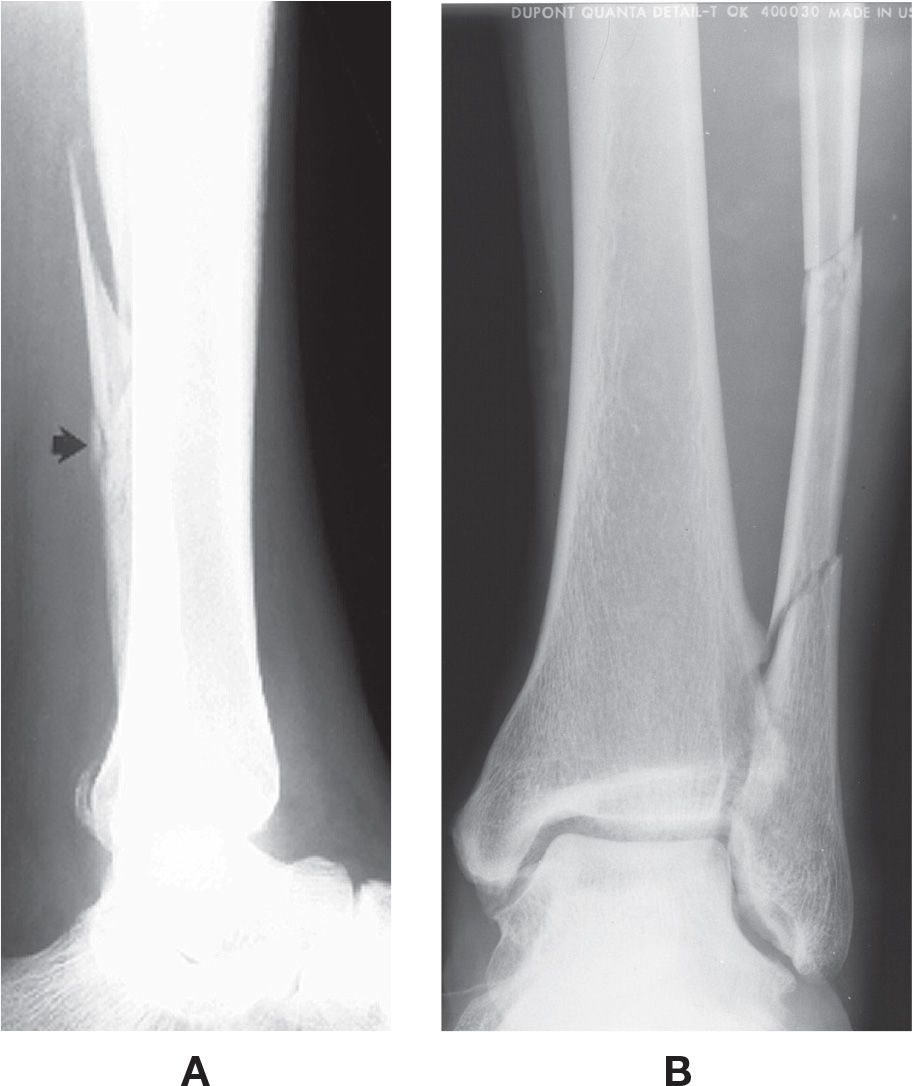
FIGURE 15-3. Comminuted fracture. A: Butterfly fragment (arrow), distal fibula. B: Segmental.

FIGURE 15-4. Greenstick fracture, second metatarsal, middle third diaphysis. Only the medial cortex is broken (arrow); the lateral is intact.
An avulsion fracture occurs as the result of muscle, tendon, or ligament abruptly pulling a piece of bone off its origin or insertion.6,10 The resulting fracture line is typically transverse in configuration. For example, in lateral ankle trauma, the mechanism of injury (inversion) results in a significant pull of the fibular ligaments onto the fibula that breaks the bone as opposed to rupturing the ligament. An example of tendon involvement is at the fifth metatarsal base where the pull of the peroneus brevis during an inversion type injury results in a fracture of the styloid process (Figure 15-6). A fracture fragment, which often has an irregular jagged border, can usually be distinguished from an accessory ossicle, which typically has a smooth, cortical margin.9–13

FIGURE 15-5. Torus fracture, first metatarsal, proximal third diaphysis. Note the “buckling” of the medial and lateral cortices (arrows); no distinct fracture line can be seen.

FIGURE 15-6. Avulsion fracture, fifth metatarsal tuberosity. The tuberosity fragment (arrow) is displaced and distracted posteriorly.
A stress fracture results from numerous microfractures that gradually develop a fault in the bone where any singular force would not normally cause any damage.5,6 Some reports suggest that over 90% of stress fractures are located in the lower extremity with the most common location being the tibia.14 Radiographs are initially negative in up to 70% of cases. A high index of suspicion based on history and physical exam should be treated as if there is a stress fracture.14 During the early period, when radiographs appear normal, advanced imaging such as bone scintigraphy (bone scan), computed tomography, or magnetic resonance imaging can be ordered to confirm the diagnosis if necessary. Bone scintigraphy has high sensitivity; however, it is the least specific of the three advanced modalities.9
There are two types of stress fracture: insufficiency and fatigue.15 The insufficiency stress fracture occurs as a result of normal stress on abnormal bone; an example would be the older patient with osteoporosis walking his or her dog. The fatigue stress fracture involves normal bone that is stressed by abnormal forces. The latter are commonly observed in athletes, dancers, and those in the military, as well as in patients who suddenly increase their activity levels, especially with rigorous physical training. Stress fracture of the metatarsal is commonly found in military recruits due to intensive training; this is referred to as a march fracture.14,16

FIGURE 15-7. Cancellous bone stress fracture, fourth metatarsal head. Note the ill-defined increased density directed transversely across the head/neck (arrow).
Radiographically, stress fractures have been described as either a compression or distraction fracture.17 The compression fracture demonstrates a transverse increased density in cancellous bone (Figure 15-7). The distraction fracture, in contrast, demonstrates a periosteal reaction, indicating the presence of cortical disruption (Figure 15-8).
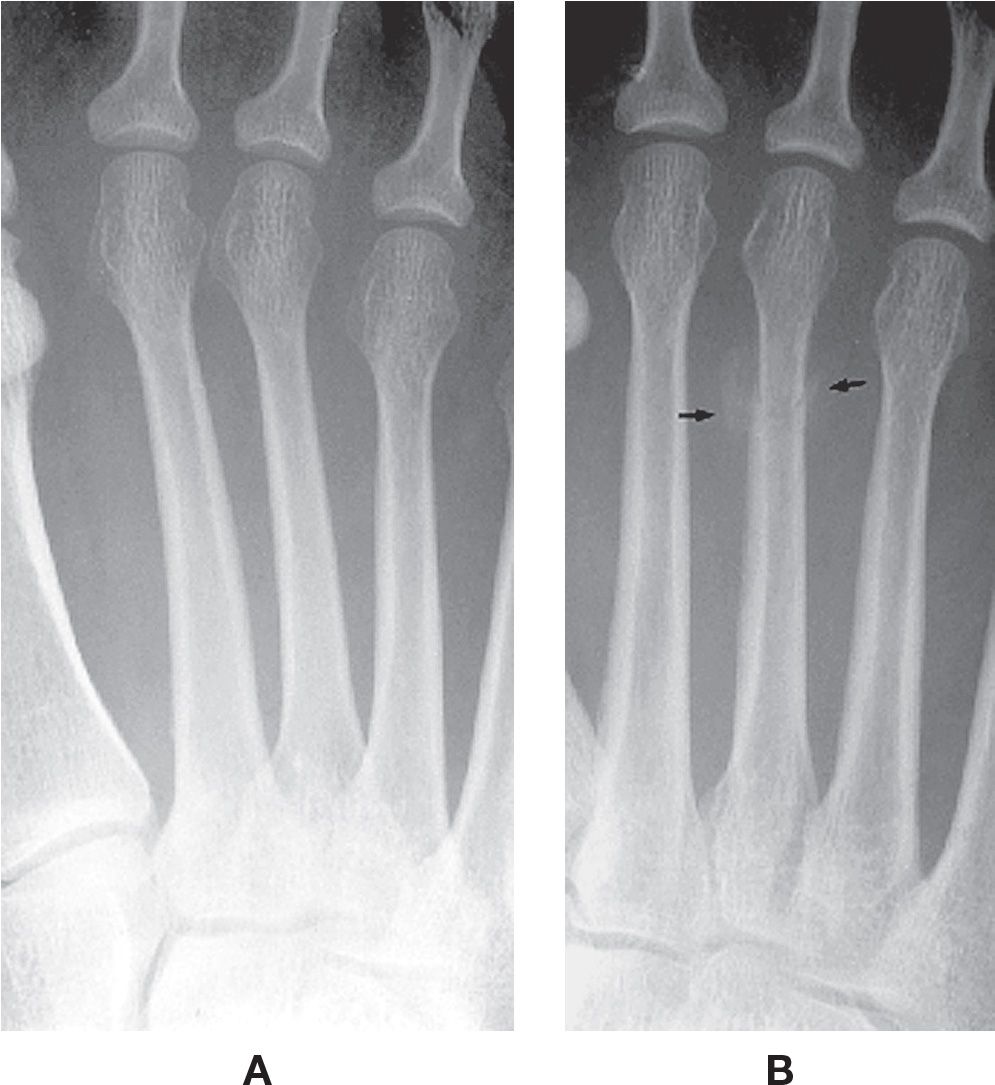
FIGURE 15-8. Cortical bone stress fracture, third metatarsal distal third diaphysis. A: Initial, normal radiograph. B: Two weeks later. Note the periosteal reaction along the margins of the fracture site (arrows).

FIGURE 15-9. Pathologic fracture, fourth toe proximal phalanx. A previously unidentified soft tissue tumor caused pressure atrophy of the adjacent bone over the course of years. The patient stubbed her toe, resulting in fracture of the weakened bone.
A pathologic fracture is one where the involved bony structure is weakened by a disease process (Figure 15-9). In other words, the force causing the fracture would not have resulted in a disruption to the structure if applied to healthy bone. Occasionally, an underlying bony pathology such as a tumor can be found incidentally when radiographically evaluating for fracture.6,18
In osteoarthritis, small osteocartilaginous fragments referred to as loose osseous bodies or “joint mice” may be observed (Figure 15-10). These small chips of bone usually develop as a result of previous trauma. Osteochondritis dissecans is a presentation that results from trauma or spontaneous necrosis. The lesion is a necrotic, subchondral bone fragment that is covered with cartilage. Radiographically, there is a subchondral defect; the fragment may be incompletely or completely detached, with varying levels of displacement.9,19 It frequently affects the talar dome (Figure 15-11).
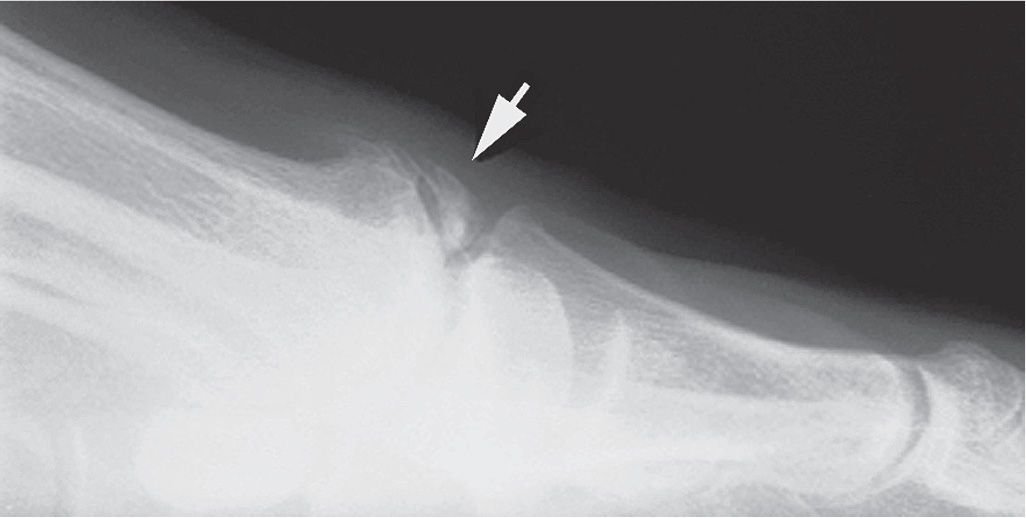
FIGURE 15-10. Loose osseous body (arrow), dorsal first metatarsophalangeal joint. Loose bodies are frequently seen at osteoarthritic joints.

FIGURE 15-11. Osteochondritis dissecans, talar dome superomedially (arrow).
Finally, descriptive words defining the fracture pattern are used to distinguish the level of displacement and angulation between fracture ends. The amount of displacement and angulation can affect treatment protocols. An undisplaced fracture has no alterations to the normal anatomical relationship between fracture fragments (Figure 15-12A).2,4,5 A fragment is considered displaced when it is greater than 2 mm in distance from the proximal fragment (Figure 15-12B). This relationship can be described using the level of apposition ranging from partial to absent (Figure 15-12C). Fragments can also be overlapping or simply distracted as in avulsion type fractures. Angular changes refer to alterations such that the longitudinal axis of the fracture fragment creates an angle with the longitudinal axis of the stationary fragment (Figure 15-13). These terms are further described and illustrated in Chapter 11.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








