Z-Scarf Osteotomy
Charles J. Gudas
HISTORICAL REVIEW
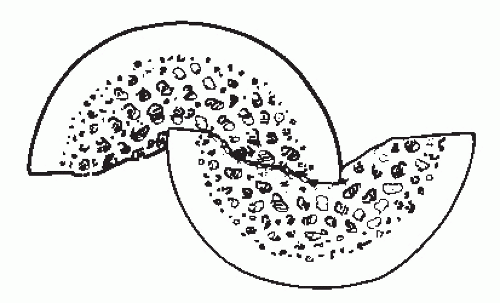
A midshaft osteotomy for the correction of hallux valgus was originally described by Meyer (1) in 1926. The procedure performed was a noninterlocking midshaft first metatarsal osteotomy performed in the sagittal plane without internal fixation. Burutaran (2) described a sagittal plane nontranslational midshaft osteotomy in 1976. From the 1970s to 1980s, osteotomies of the first metatarsal shaft were usually performed in the proximal or distal metaphysis of the bone with minimal internal fixation. In the early 1980s, AO techniques were used at the University of Chicago for stabilization of various noninterlocking osteotomies including the Ludloff and Mau osteotomy. In 1983, Zygmunt and Gudas devised an interlocking transpositional midshaft first metatarsal osteotomy that would allow multiple internal fixation devices to stabilize the osteotomized fragments (Fig. 30.1). Given the configuration of the osteotomy, the Z-Scarf osteotomy was designed to be more stable than the Mau or Ludloff procedure because of the interlocking parallel bone cuts. Barouk (3,4,5 and 6) popularized the procedure from 1900 to 2000 in Europe and the United States. Borrelli and Weil (7) described the procedure as a Scarf cut, which is a woodworking term to describe a joint made by chambering or cutting the ends of two pieces of wood to be joined. The angled cut on each piece is made to correspond to each other so that the pieces joined are flush. The osteotomy was designed to have the ability to correct both the intermetatarsal angle (IMA) and the distal metatarsal articular angle (DMAA). Given the configuration of the osteotomy, plantarflexion, lengthening, or shortening of the first metatarsal could also be achieved.
EVALUATION/DIAGNOSIS/FUNCTIONAL ANATOMY
Preoperative evaluation of a patient, in whom a Z-Scarf osteotomy is contemplated, should include a thorough weightbearing and non-weight-bearing examination of the foot and lower extremity to determine functional and biomechanical factors that affect the formation of hallux valgus and may have an impact on the successful outcome of the Z-Scarf procedure.
Examination of the foot and ankle should include analysis of hypermobility and pronatory factors and the Achilles complex for any contracture, if present. Grebing and Coughlin (8,9 and 10) noted that 81% of controls and 67% of those patients with hallux valgus had 10 degrees or less of ankle dorsiflexion. No correlation was found by the two authors in relation to ankle dorsiflexion and the magnitude of hallux valgus. Coughlin and Jones reported an incidence of 12% having less than 5 degrees of ankle dorsiflexion and 54% having less than 10 degrees of ankle dorsiflexion in patients with moderate or severe hallux valgus. In their study of 122 feet, no Achilles lengthenings or gastrocnemius slide procedures were performed (8).
Hypermobility of the metatarsocuneiform joint may have an effect on the overall outcome of distal or midshaft osteotomy. King and Toolan studied first ray hypermobility by manual and x-ray examination and concluded that there may be an association between first ray hypermobility and hallux valgus formation. Coughlin and Jones further reported a 23% incidence of radiographic gapping on the plantar aspect of the first metatarsocuneiform joint, which may or may not be related to first ray hypermobility (8). They subsequently concluded that hypermobility may be secondary, rather than a primary cause of hallux valgus (9). Therefore, ligamentous laxity and pronation should be assessed prior to performing this procedure.
Beighton and Bird developed a nine-point ligamentous laxity scale, examining the elbow, knee, little finger, and hands. A score of greater than six points demonstrated generalized ligamentous laxity. Beighton concluded from this study that 90% of males and 80% of females scored two or fewer points. In the author’s experience, generalized ligamentous laxity in adult patient populations is rare, but if present may necessitate a midfoot fusion technique rather than a midshaft osteotomy procedure. Pronation of the foot is another consideration on the forces generated across the osteotomy site during and after healing of the osteotomy occurs.
Many studies have been performed on the incidence of hallux valgus and pronation of the foot. Hohmann (11) asserted that hallux valgus always occurred secondary to a pronated foot. Grebing and Coughlin (8,9 and 10) reported a twofold increase in the incidence of pronation associated with hallux valgus formation, but found no correlation between the hallux valgus angle and pes planus or between pes planus and first ray hypermobility.
Radiographic evaluation should include analysis of osteopenia, evidence of arthrosis of the first metatarsal phalangeal joint or the first metatarsocuneiform joint, hallux valgus angle, first and second IMA, distal metatarsal angle, hallux interphalangeal angle, analysis of joint congruency, first metatarsal medial cuneiform angle, metatarsus adductus angle, radiographic gapping of the plantar first metatarsocuneiform joint, and length and width measurements of the first metatarsal to ascertain if there is enough “room” for the osteotomy. In females, the distal and proximal metaphyseal width should measure 15 to 20 mm. In males, the metaphysis width should measure 20 to 25 mm. In females, the midshaft measurement should measure at least 12 mm, and in males 14 mm. These measurements should allow adequate space within the first metatarsal to adequately perform the osteotomy (Fig. 30.2). In juvenile or adolescent hallux valgus, the epiphyseal plate location in the base of the first metatarsal and base of the proximal phalanx must be precisely measured both preoperatively and intraoperatively to avoid damage to the epiphyseal plate. Functional analysis should also include range of motion of the first metatarsophalangeal joint.
The presence of metatarsalgia beneath the second and third metatarsal heads should be determined prior to surgery.
Associated deformities such as contracted second and third metatarsophalangeal joints with hammertoe formation often accompany severe hallux valgus and should be factored into the decision concerning overall correction in addition to the first metatarsal osteotomy.
Associated deformities such as contracted second and third metatarsophalangeal joints with hammertoe formation often accompany severe hallux valgus and should be factored into the decision concerning overall correction in addition to the first metatarsal osteotomy.
 Figure 30.1 Radiographic example of a 20+-year postoperative interlocking transpositional midshaft first metatarsal osteotomy as devised by Zygmunt and Gudas in 1983. |
The severity of the deformity can be graded into mild (Grade 1), hallux valgus angle less than 20 degrees, moderate (Grade 2), hallux valgus angle 20 to 40 degrees, severe (Grade 3), 40+ degrees.
CRITERIA/SELECTION OF PROCEDURE/CONTRAINDICATIONS
The Z-Scarf osteotomy was designed to be a bridging osteotomy between a proximal and distal osteotomy. The Z-Scarf procedure is usually performed in patients with moderate and severe hallux valgus. The Z-Scarf osteotomy is also indicated in patients with adequate bone stock. In patients with osteopenia, the osteotomy can damage the integrity of the first metatarsal causing later fracture, malposition, troughing, and collapse of the first metatarsal resulting in joint impingement and stiffness of the first metatarsophalangeal joint with increased incidence of lateral metatarsal transfer lesions, as well as loosening or instability of the hardware. Bone troughing is created when the osteotomy is performed mostly in diaphyseal bone allowing the displaced cortices of bone to collapse into the medullary canal causing elevation of the distal fragment (Fig. 30.3).
As previously mentioned, the first metatarsal must be wide enough to adequately perform an osteotomy that will fully correct the deformity. Transposition and translation of the osteotomy fragments are obviously limited by the width and length of the first metatarsal, the narrower the bone, the less the ability to rotate or translate the plantar osteotomy fragment. Regarding IMAs, the Z-Scarf osteotomy is also indicated for those between 13 and 20 degrees. IMAs below 13 degrees are often best treated with a Chevron procedure. IMAs above 20 degrees are best reduced with a proximal osteotomy, Lapidus fusion, double osteotomy, or fusion of the first metatarsophalangeal joint. DMAA angles of 6 and 15 degrees can also be addressed with the Z-Scarf osteotomy depending on the width of the metatarsal and the angulation of the dorsal and plantar bone cuts. Care must be taken to avoid overreduction of the DMAA angle, which may result in decreased IMA reduction and incomplete reduction of the deformity. A relatively short first metatarsal length pattern is also an indication for this procedure. Careful preoperative measurements will allow the surgeon to compensate for the bone saw blade width to preserve the length of a short metatarsal. The presence of an open epiphyseal plate is not a contraindication to this procedure. Care must be taken to adequately measure the exact location of the proximal epiphyseal plate prior to performing the procedure. Excellent results have been obtained with this procedure in adolescent bone, but the author would caution the use of this procedure under the age of 10 years due to the high recurrence rate and potential damage to the juvenile epiphyseal plate.
 Figure 30.2 Surgeon making width measurements of the first metatarsal to ascertain if there is enough “room” for the osteotomy. |
Contraindications to the Z-Scarf osteotomy include operator inexperience with the performance of the procedure. The operating surgeon should have some prior experience involving saw bone or cadaver experience prior to actually performing the procedure. This will minimize intraoperative and latent complications of the Z-Scarf osteotomy. This procedure should be used with care in women over the age of 55 and men over the age of 60. Successful performance requires adequate bone
stock without evidence of osteopenia. Limited metaphyseal-diaphyseal bone width measurements, as discussed earlier, in both males and females are a contraindication for this procedure. There must be sufficient bony volume to adequately perform a complete osteotomy. Obesity and inability to maintain nonweight status is also a contraindication. In the author’s experience, the best results are obtained from a Z-Scarf osteotomy with limited or non-weight-bearing for 4 weeks after the procedure. The main reason for limited or non-weight-bearing is to protect the type of internal fixation currently utilized. In patients with less than optimum bone, fixation techniques involving neutralization with limited compression are utilized to avoid collapse and troughing of bone. This can be achieved by insertion of a noncompressive headless cannulated screw into the first metatarsal head with the addition of one or two regular cannulated on noncannulated compression screws proximal to the first screw in the proximal midshaft of the proximal osteotomy site. Moderate joint arthrosis is a contraindication to this procedure. In mild hallux limitus, this procedure may be performed if plantarflexion of the first metatarsal head fragment can be achieved with the osteotomy cut.
stock without evidence of osteopenia. Limited metaphyseal-diaphyseal bone width measurements, as discussed earlier, in both males and females are a contraindication for this procedure. There must be sufficient bony volume to adequately perform a complete osteotomy. Obesity and inability to maintain nonweight status is also a contraindication. In the author’s experience, the best results are obtained from a Z-Scarf osteotomy with limited or non-weight-bearing for 4 weeks after the procedure. The main reason for limited or non-weight-bearing is to protect the type of internal fixation currently utilized. In patients with less than optimum bone, fixation techniques involving neutralization with limited compression are utilized to avoid collapse and troughing of bone. This can be achieved by insertion of a noncompressive headless cannulated screw into the first metatarsal head with the addition of one or two regular cannulated on noncannulated compression screws proximal to the first screw in the proximal midshaft of the proximal osteotomy site. Moderate joint arthrosis is a contraindication to this procedure. In mild hallux limitus, this procedure may be performed if plantarflexion of the first metatarsal head fragment can be achieved with the osteotomy cut.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree