Absorbable Biomaterials
Adam S. Landsman
Absorbable biomaterials have filled an important niche among the devices designed for repair of fractures and reconstructive surgery. When considering absorbable devices, most surgeons tend to think of bony repair, but new products used for soft tissue augmentation are also available. Technically, absorbable suture materials should probably be considered to be the first absorbable biomaterial, but this is not the focus of the current chapter. Absorbable biomaterials can be roughly divided into materials designed for fracture and osteotomy stabilization and for soft tissue repair and augmentation. These areas will be looked at from the perspective of the foot and ankle surgeon.
Biomaterials that absorb following implantation have many advantages. Absorption and incorporation or dissolution of the device results in a gradual transfer of mechanical loads from the device itself to the surrounding tissues. As a result, problems such as stress shielding, which is associated with exceptionally rigid devices, and pain associated with bulky or irritating hardware are diminished over time. Absorbable devices are also radiolucent, which may be helpful when assessing fracture healing or osteotomy position. Because of the ability to modify absorbable devices without the fear of metallic fragmentation, these devices can be ground or cut during surgery, and this opens up a whole new array of options to the creative surgeon. Finally, absorbable products also enjoy a high acceptance rate among patients who would otherwise worry about the presence of permanent implants that may require subsequent surgeries for removal.
There are also some drawbacks associated with the use of absorbable biomaterials. In general, absorbable materials are much weaker than nonabsorbable devices (1,2). It has been shown that absorbable devices show loss of strength, well ahead of the time when the device is completely absorbed. Therefore, it is imperative that a device retains sufficient strength to allow the adjacent bone or soft tissues to fulfill their roles in the healing process before the mechanical integrity of the implant is lost. Most absorbable orthopedic devices will retain sufficient strength for up to 8 weeks, before there is a significant loss in strength. If one considers the healing process in bone, by the 8th week, bone callus has formed, and the fracture or osteotomy site is stable. In theory, the implant is no longer needed at about the time it begins to break down. This also holds true for absorbable anchors used to attach soft tissue to bone. These biotenodesis devices only need to stabilize the soft tissue, until it attaches to the adjacent bone, and only need to hold beyond the breaking strength of the suture used to attach the anchor to the soft tissue.
Early versions of absorbable screws and pins were plagued with reports of sterile sinus formation, fibrous encapsulation, and osteolysis localized to the area surrounding the absorbable implant (3,4 and 5). In general, these types of reactions are attributed to excessively rapid breakdown of early types of polyglycolic acid in the implants. Current absorbable devices counteract this problem with the addition of copolymers that slow the breakdown process and use other types of polymers such as poly-L-lactic acid. Degradation occurs through the process of hydrolysis and macrophage responses, leaving behind only water and carbon dioxide. By making these modifications, modern devices will not show appreciable degradation for months to years, as opposed to weeks for the early devices (6,7).
In this chapter, several implantable biomaterials used by the foot and ankle surgeon are examined. Absorbable screws and pins offer an effective and long-lasting, but not permanent, way to repair fractures and stabilize osteotomy sites while bony healing occurs. Absorbable arthroereisis plugs can be inserted into the subtalar joint in a relatively young patient with a flatfoot deformity while the bony structure is developing, with less potential needed for removal, as the plug resorbs over time. Finally, collagen bioscaffolds are examined. This relative newcomer to the foot and ankle surgeon’s tool kit is critical for tendon and ligament repair, and appears to have promising benefits in joint resurfacing and fat pad augmentation, as well as tendon and ligament reinforcement.
IMPLANT SELECTION
In the case of an absorbable device, selection of the proper implant has to take into account the strength of the device and the period of time when fixation or stabilization will be needed. There may also be physical constraints associated with the placement of the device.
ABSORBABLE SCREWS AND PINS
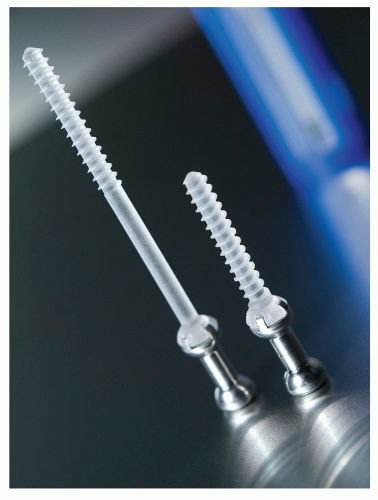
Absorbable screw and pin fixation has become readily available in the last decade, although their use lags far behind that of traditional metallic implants. It is important to understand the trade-offs associated with absorbable devices when compared with metallic implants. When assessing a screw, the material strength is only one potential measure. In actuality, the holding power and compression achieved by the screw are dependent on the thread geometry and ability to integrate with the surrounding bone, rather than the actual material. Thread shape, spacing, and depth are frequently described in terms of profile, pitch, and diameter. Although the absorbable screw can mimic some attributes of a metal screw, there is an inherent weakness in the actual material that limits the options. For example, cannulation of very small diameter screws causes substantial weakening of the absorbable implant. Similarly, self-tapping absorbable screws have threads that are not as stiff as those found in metallic screws, and require tapping to cut their way into the adjacent bone (Fig. 3.1).
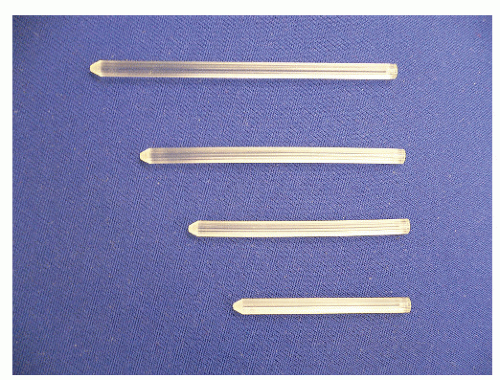
Like absorbable screws, absorbable pins cannot achieve the stiffness (resistance to bending) or the sharp tip of their metallic counterparts (1,2). As a result, there is a need to predrill
when inserting absorbable pins. Some designs involve a gradual taper of the absorbable pin, which allows them to fit more tightly as it is inserted deeper into the bone. Because predrilling is necessary, the number of sites where this type of fixation can be used may be restricted (Fig. 3.2).
when inserting absorbable pins. Some designs involve a gradual taper of the absorbable pin, which allows them to fit more tightly as it is inserted deeper into the bone. Because predrilling is necessary, the number of sites where this type of fixation can be used may be restricted (Fig. 3.2).
Despite the mechanical issues described above, there are several positive aspects to using absorbable screws and pins. At the time of insertion, if there are any areas where the fixation is impinging or too prominent, the device can be simply ground down, without worries associated with metallic fragmentation. Any particles remaining after irrigation will simply dissolve. This allows for a smoother profile at the bony surface.
After initial insertion, hydrolysis begins, and there is a slight swelling of the absorbable device during the first few days after implantation. This causes the device to fit more snugly than it did at the time of insertion. As hydrolysis progresses, there is a gradual shift in load bearing from the device to the adjacent bone. Thus, as the fracture or osteotomy site begins to heal, the device gradually dissolves. This becomes critical in cases in which extended use of a rigid device actually weakens the adjacent bone. In order to maintain its density, bone must be stressed, and the stiff device carries some of the mechanical load normally carried by the bone. As a result, the device shields the bone from a portion of the stress applied, resulting in reduced bone density over time. This stress shielding effect can be very pronounced in the case of an ankle fracture, for example, where there is a risk of refracture.
Although costs associated with absorbable devices frequently prevent surgeons from using them, the cost differential for specialized screws (i.e., low profile, cannulated, or variable pitch) and absorbable devices as well as absorbable and metallic arthroereisis devices has decreased dramatically over the last 5 years. Nonetheless, cost differences between traditional metal Kirschner wires (K-wires) and absorbable pins remain substantial.
There are many applications in which the use of absorbable wires and/or screws would be appropriate. It is important to recall that the mechanical force needed to bend an absorbable device is less than the force needed to bend a steel or titanium device of similar diameter. However, this flexibility difference is greatly diminished when very small pieces of absorbable material are used, such as in the threads of a screw. In fact, the thread geometry, and by extension, the amount of bone trapped within the threads, is a much more important determinant of the holding power of a screw. Laboratory data have demonstrated that there is no significant difference in the holding power—and therefore in compression—generated by absorbable screws as compared with equally sized steel screws inserted into corticocancellous bone models (8,9 and 10). However, these materials differ in their ability to resist shear and repetitive (fatigue) loads.
When comparing steel wire fixation (i.e., K-wires) with absorbable devices of the same diameter, the smooth K-wire will be much more resistant to bending than the absorbable device. However, both devices are extremely strong when placed in a position where shear is the primary loading modality.
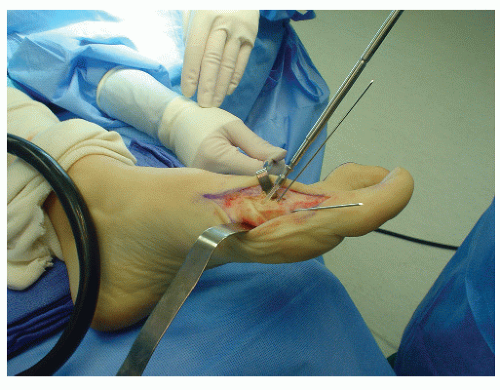
In light of these differences in mechanical properties, what is the optimal use for an absorbable device, and when should it be avoided? Based on the 8-week window that exists before substantial absorption occurs, applications in which 8 weeks will be sufficient for achieving at least partial union should be selected. A first metatarsal osteotomy performed with an intrinsically stable construct is a good choice for this type of screw fixation (Fig. 3.3). Compression is achieved, and there is little risk of shear or fatigue damage to the screw. There are several advantages in this case over steel fixation. First, remodeling of the screw head can be done safely, simply by grinding away any prominences. If the placement of the screw caused the tip to interfere with the sesamoids, it is comforting to know that the screw will eventually absorb, automatically eliminating this problem. Second, there is usually no need for additional procedures
due to painful retained hardware. Third, the devices are nearly radiopaque, making it easier to assess bony union. Fourth, patient acceptance of absorbable devices is much higher than metallic devices. Fifth, the risks of stress shielding and stress risers around the fixation are reduced.
due to painful retained hardware. Third, the devices are nearly radiopaque, making it easier to assess bony union. Fourth, patient acceptance of absorbable devices is much higher than metallic devices. Fifth, the risks of stress shielding and stress risers around the fixation are reduced.
Similarly, absorbable pins are ideal for small bone fragment fixation in locations where the surgeon may have used traditional steel wires in the past. Unfortunately, in many cases in which a small fragment is fixated with steel, migration of the steel wire occurs due to micromotion of the fixation, and this results in a prominent device that ultimately requires a second procedure for removal. The absorbable device can simply be left in place, since it will dissolve completely over time.
Applications in which an absorbable screw or pin is exposed to repetitive shear forces will probably lead to early fixation failure, with all of the associated ramifications, including nonunions or malunions and fracture displacement. Classic examples of unstable fractures in the foot and ankle include comminuted fractures of the fibula or midfoot osteotomies subjected to early weight-bearing. However, intrinsically stable fractures and osteotomies or fractures protected with casts, guarded ambulation, or other modalities can be treated quite effectively with absorbable devices.
ARTHROEREISIS PLUGS
Arthroereisis implants can be an especially good place to use absorbable materials. Complications associated with the use of arthroereisis plugs in adults for the treatment of posterior tibialis tendon dysfunction, pathologic pes planus, and Kidner foot are numerous, and removal may be required in up to 50% of the cases due to pain associated with hindfoot (subtalar joint) stiffness. Typically, the correction is outstanding initially, but the hardness of the device leads to deep pain and patient intolerance, and the plug ultimately requires removal. When an absorbable device is used, the device can remodel and diminish in size with time, leaving the corrected position behind as soft tissues fibrose and take over the stabilizing process (11). Also, in the initial phases, the absorbable device is softer than comparable steel devices.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree