In basic terms, a suture is a strand of material that can be used to bring soft tissues into apposition and to tie off or ligate blood vessels. Once implanted, sutures must provide strength at the wound margins during a critical period of wound healing, when tissue lacks sufficient strength to support itself (
1,
2). Until sufficient wound healing has taken place, the burden of all forces acting at the wound margin is placed solely on the suture. If the suture fails to maintain apposition of the wound margins, further soft tissue damage, loss of correction, or wound dehiscence may result.
The history of surgical suture goes back thousands of years. The earliest known written accounts of wound closure with sutures and needles are evidenced in ancient Egyptian scrolls dated 3500 BC (
3,
4). The earliest materials were fashioned from animal sinews, animal hair, and plant fibers (
3). Today, we use a variety of suture materials, natural and synthetic, absorbable and nonabsorbable, with single and multifilament strand configurations. They may be uncoated or coated, naturally colored or colored with FDA-approved dyes. Variables in the composition and construction of a suture affect everything from the ease with which the product is handled to its interaction and performance once inserted into the body.
The United States Pharmacopeia (USP) is the official compendium for defining and describing the physical characteristics of each suture material (
1,
5). These characteristics include strength, size, needle attachments, and ability of the material to absorb fluid (
1,
5). The USP also sets forth standards for the manufacturing, packaging, storage, sterilization, and labeling of sutures (
1,
5).
Sutures are sterilized with either ethylene oxide gas or ionizing radiation, usually from cobalt 60 (
1,
6). Both are considered cold sterilization because exposure to heat, as with an autoclave, may cause damage to the product or its packaging (
1,
6,
7 and
8). Some suture materials, such as cotton, must be sterilized with ethylene oxide gas, as ionizing radiation may damage its fibers (
6,
7).
Suture packaging is designed to protect the material from environmental factors such as light, oxygen, and moisture. Package design maintains sterility of the product and allows for an easy means of suture delivery to the sterile field of operation. Each package is labeled with information regarding the enclosed product to include the material from which the suture is made; whether it is coated or uncoated; suture type, either natural or synthetic, absorbable or nonabsorbable; its size, both metric and USP size designation; suture length; suture configuration; description of the needle; the number of sutures included; lot number; name of the manufacturer; trade name of the product; and expiration date (
5). Most sutures are packaged dry; however, collagen-based sutures are packaged wet, usually in alcohol, to prevent them from drying out (
7). “Pliabilized” nylon suture (Ethicon, Somerville, NJ), used for cosmetic and plastic surgery, is packaged premoistened, which makes it easier to handle (
6).
The USP divides sutures into two categories: absorbable and nonabsorbable (
5). These main categories can then be subdivided into natural and synthetic materials for each. An absorbable suture is one that will lose most of its strength within 60 days following implantation (
1). These sutures include catgut, polydioxanone (PDS), polyglactin 910, and polyglycolic acid (PGA) (
1). Absorbable sutures may be natural, of animal origin (collagen), or synthetic (
1) (
Table 4.1). These materials may be fashioned into monofilament or multifilament strands to offer the best handling and performance characteristics for that product. They may be of natural color or dyed to maximize their visibility. Absorption of the suture means that its presence in the soft tissues is temporary, as is its capacity to hold tissues together. The initial strength of an absorbable suture material is directly proportional to its thread diameter. The rate at which it loses its strength, however, is independent of its size and rate of absorption (
9). Absorption begins as a loss of tensile strength followed by a loss of mass of the implanted product. Some materials are present in the tissues long after they have lost their effective tensile strength. Therefore, familiarity of each absorbable sutures interaction with the body, its rate of absorption, and the rate at which it loses its strength must be weighed against the anticipated healing time for the tissues being sutured (
2).
The term
nonabsorbable is a relative term because many of the sutures that we consider to be nonabsorbable are in fact degraded in the tissue, although at a very slow rate (
1) (
Table 4.2). Some sutures are not subject to absorption no matter how long they have been implanted. These include stainless steel, polyester, polybutester, and polypropylene (
1). Nylon and silk, although classified as nonabsorbable, are absorbed over many months (
1,
10). Soft tissue reaction to nonabsorbable sutures is, overall, milder than that of the absorbable sutures (
Table 4.3). Nonabsorbable sutures may be coated or uncoated, multifilament or monofilament to maximize their handling properties. They may be uncolored or dyed to offer better visibility (
6).
SUTURE CONFIGURATION
Sutures may be described and differentiated in terms of their fiber arrangement. The physical configuration of a suture refers to whether it is fashioned as a monofilament or a multifilament structure (
1) (
Tables 4.1 and
4.2). A suture’s configuration will affect its handling characteristics and its interaction with the body.
Monofilament sutures are a single strand of either an absorbable or nonabsorbable material. The monofilament configuration provides an overall smoother, low-friction surface that allows the suture to glide easily through soft tissues and slip easily, but not necessarily securely, into a knot. Another benefit of this smooth suture surface is that it provides less shelter for bacteria.
Many of the synthetic absorbable suture materials are very stiff, which precludes their use as a monofilament suture (
11). Instead, thin strands of these materials are fashioned into multifilament strands, which affords them greater flexibility and strength (
11). Some newer synthetic materials such as PDS and polyglyconate, however, offer excellent handling characteristics and strength, even as a monofilament.
Multifilament suture materials can be natural or synthetic, absorbable or nonabsorbable. They are formed by twisting or braiding several single filaments together to form one suture strand of a desired thickness. Synthetic multifilament sutures are formed by first liquefying the polymer and then extruding it through spinnerets to form narrow, monofilament strands. These strands are then braided or twisted together to form an appropriate-size multifilament suture thread (
1,
12). Multifilament synthetic sutures are relatively flexible and easy to handle as compared with monofilament synthetic sutures that tend to be stiff and wiry. Uncoated multifilament suture has a rough texture that generates high levels of friction when moved through soft tissue. High levels of friction create soft tissue drag that can cause tissue damage and make insertion and removal of suture difficult. A beneficial consequence of this rough, high-friction surface is that it affords a relatively secure knot. Uncoated multifilament sutures also have a tendency to absorb and harbor bacteria in their fiber arrangements. It is for these reasons that many multifilament sutures are offered with coatings that help to reduce tissue drag and lower the propensity for bacterial uptake between suture filaments.
KNOT SECURITY
Knot strength is defined as the mean tensile strength of the knotted suture (
15). The knot is typically the weakest point in a suture loop (
15). Its efficacy is determined by comparing the tensile strength of knotted versus unknotted suture of the same material and same dimensions (
15). Knot failure may occur either due to slipping or due to knot break. There are several factors that impact the security of a knot. A knot is deemed secure if it can hold, without significant slipping, to the point of knot break when subjected to a sufficient force (
19). When suture breaks, the knot is usually the site of the break and is a result of shear forces generated within the knotted configuration (
19). For absorbable sutures, knot strength decreases as the suture is absorbed (
19).
Knot failure is more likely to occur due to knot slippage rather than an outright break. Knot slippage is an untying of the knot that occurs, to some degree, with all suture materials (
20). This can result in either complete failure of the suture loop or widening of its diameter with resultant separation of soft tissue margins (
20). Improper tying technique, the type of knot thrown, and the smoothness of the suture material can all contribute to slippage.
Coefficient of friction is a measure of the slipperiness of a suture material (
1). A suture material with a low coefficient of friction is smooth, will glide easily through soft tissues, both
when inserted and removed, with less effort and with less patient discomfort (
1). A suture material with a low coefficient of friction will tie easily and glide smoothly into a knotted configuration (
1). Once tied, however, the knot may also slip more easily, loosen, or become completely untied (
1). Some suture materials, like polyester, are coated with special polymers to decrease their coefficient of friction (
1). These coatings improve handling characteristics while maintaining knot security.
Suture materials with a high coefficient of friction tend to be rougher in texture. Setting a knot requires more effort as the rough, high-friction material is dragged across itself while being moved into a knotted configuration (
1). This same friction, however, will help to maintain the suture in its knotted configuration, even when acted upon by additional forces such as those brought on by edema (
1). Plain catgut and monofilament and multifilament steel have high coefficients of friction and have the highest knot efficacy among all suture materials, independent of the type of knot thrown (
13). Multifilament, uncoated suture materials such as polyester also have a very high coefficient of friction and rank just below steel and catgut in terms of knot efficacy (
Table 4.5).
The type of knot being tied causes more variation in knot efficacy than variations in the type or size of the suture material (
13). Simple crossed knots are very inefficient for most suture materials, with steel and catgut being the exceptions (
13). For catgut and multifilament and monofilament steel, knot strength has been shown to be independent of the type of knot thrown (
13). Most materials, however, require a more complex knot, meaning a greater number of throws, to afford them security. Complex knots, three throws or better, have, on average, greater knot efficacy, almost twice that of simple knots (
13,
19,
21). In some cases, the addition of one extra throw may increase the knot strength by threefold (
21). Additional throws are recommended for materials with a low coefficient of friction, monofilament synthetic nonabsorbable and coated sutures (
6). Throws added in addition to what will provide for a secure knot do not contribute significantly to the strength of the knot but instead will increase the suture volume in or near the wound. The increased volume offers more surface area to harbor bacteria and amplifies the local inflammatory reaction to the suture (
6,
22). A balance must be maintained between adding too many throws, too much suture material, and throwing too few loops resulting in a week knot that will slip (
21). The square knot and the surgeon’s knot are the most secure and reliable knots for tying most suture materials (
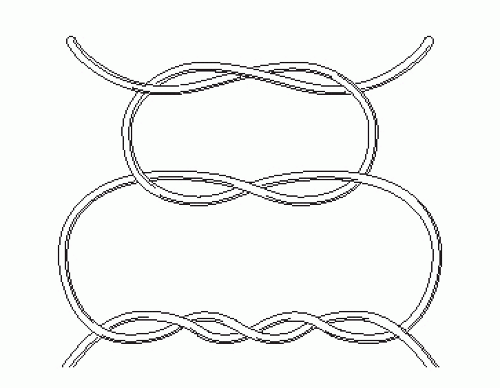
6). The surgeon’s knot with the addition of a square knot is very reliable (
Fig. 4.1). The number of throws and type of knot needed to make the knot secure varies with different suture materials, and there are often specific recommendations per the manufacture provided in the package insert.
Knot security is more dependent on the type of material the suture is made of than on the dimensions of the suture (
13,
23). No clear correlation can be made between thread diameter and knot efficacy for most suture materials (
11,
23,
24 and
25). For some stiffer, monofilament suture materials, such as monofilament nylon, knot efficacy may increase somewhat with narrower-diameter sutures. This is likely due to the more pliable (bendable) nature of the narrower product, which allows the knot to be set more securely (
22).
The length of the cut ends of a suture must be long enough to allow the knot to slip to some degree without completely untying (
20). Cutting the suture ends too long, on the other hand, leaves more suture material in or near the wound, which may incite an inflammatory response and harbor bacteria (
20). It is recommend that a 3-mm tail remain to offer some room for knot slip while minimizing the amount of extra suture left in or near the wound. Some materials are more prone to knot slip. These materials tend to have a high degree of memory and a low coefficient of friction, as seen with some synthetic monofilaments like nylon. These materials require additional throws and longer cut ends, up to a 6-mm tail, to guard against knot failure due to slippage (
6).
Surgeon’s technique is a major factor in knot security. It has been demonstrated that improper knot tying technique can lead to knot slippage and failure (
22). The knot must be secured snugly into place with uniform tension maintained on both ends of the suture to insure a square knot is being tied and not a slip knot, which is relatively insecure (
21,
24).
BIOLOGIC PROPERTIES
All suture materials, both absorbable and nonabsorbable, are recognized as a foreign body and will elicit some degree of a soft tissue response (
1,
2,
11). The degree and severity of the response will vary depending on the type of material, its configuration, and the quantity of material implanted (
1,
26).
Several simultaneous histologic reactions occur as the host tissue reacts to the foreign material. Cells are recruited to clear debris, break up, and absorb suture material. At the
same time, other cells are recruited to make collagen to heal the wound (
11,
12).
The initial soft tissue reaction, which is the same for all types of needles and all types of suture materials, is the result of the inherent damage sustained during the passage of the suture material and needle (
1,
12,
27,
28). The cellular response to the implanted suture material then begins and will peak at 2 to 7 days postimplantation (
1,
29). After this initial response, between 7 and 10 days postimplantation, variations in the inflammatory reaction can then be seen for different types of suture (
12,
30).
Minimizing the soft tissue reaction is important because a prolonged and severe reaction may lead to a heavy buildup of exudates and debris, which may delay wound healing and increase the risk of infection (
1,
2,
27,
31,
32 and
33). A large inflammatory reaction zone around the implanted suture material can also affect how well the suture is able to hold the tissue margins in apposition (
31,
32,
34). A wide reaction zone means the tissue inside the suture loop may be weakened, thereby increasing the risk of the suture material cutting out of the wound margins (
31). Madsen (
30,
31 and
32) showed that plain catgut caused a severe soft tissue reaction with large amounts of exudates and a wide reaction zone around the suture. This caused a delay in collagen formation and a delay in wound healing (
30,
31 and
32). If wound healing is delayed, the risk for wound dehiscence increases as the weakened incision site may lack sufficient strength to support itself by the time the suture is either removed or absorbed (
30,
31 and
32).
The degree and severity of soft tissue response to absorbable sutures varies among the materials but is overall greater than that elicited by nonabsorbable sutures. Multifilament materials and natural materials will elicit more of a response than monofilament and synthetic materials (
1,
34). Plain catgut elicits the most severe inflammatory response among all suture materials followed by chromic catgut then natural fiber materials such as silk (
24,
30,
31 and
32,
34). For all suture materials, the inflammatory reaction will be greater with an increase in the volume of implanted suture (
1,
22,
31,
32).