Plantar Foot Surgery
J. Michael Miller
Suhail B. Masadeh
The indication for plantar foot surgery began primarily out of necessity as opposed to an elective approach to address particular foot pathology. Historically, plantar foot incisions have been avoided due to the concern of painful scar formation and difficult postoperative incision protection (i.e., non-weightbearing). With an appropriate understanding of incision placement, procedure selection, tissue handling, and off-loading measures, plantar foot incisions can be successfully utilized for plantar foot pathology or even chosen as an elective approach for some common operative conditions.
The plantar aspect of the foot provides several unique anatomical characteristics that can create challenges for the surgeon. The integument thickness, neurovascular and musculoskeletal anatomy, and protection against mechanical stresses are important issues that have to be given consideration prior to selecting a plantar incisional approach.
ANATOMY
The plantar skin is unique in that it is considerably thicker than other integumental areas of the body. Anatomically it is greatly keratinized, hairless, and filled with a dense collection of sweat glands. Fibrous septae originating from the plantar fascia adhere to the plantar skin to provide increased mechanical support in resisting shear forces associated with ambulation. The superficial fascia has abundant fibrous-lipoid tissue that assists in shock protection. The thickness of this tissue is most notable on the forefoot and heel areas (1).
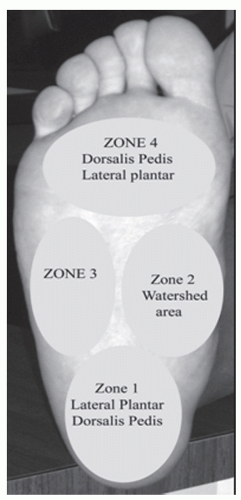
The neurovascular anatomy of the plantar foot primarily arises from the posterior tibial nerve and artery. The peroneal artery laterally also contributes vascular infusion to the plantar foot along with some communicating branches from the dorsal foot vascular network. The cutaneous nerves and vessels lie within the superficial fascia and include the medial and lateral calcaneal nerves and vessels, branches of the medial and lateral plantar nerves and vessels, and their plantar proper digital end points (2). The peroneal artery provides vascular inflow to the lateral and plantar heel via its calcaneal branch. Curtin and Hidalgo’s work on infrared photography and cadaveric injection studies revealed the plantar foot also relies on anastomosing arterial supply from the dorsalis pedis and the anterior perforating peroneal artery along with the posterior tibial artery and its branches (3,4 and 5). Hidalgo went on to describe four zones of the plantar arterial supply (Fig. 41.1). The first zone, the plantar proximal region, is supplied by the dorsalis pedis and lateral plantar artery. The second zone is the midplantar region and is supplied by multiple sources and termed the watershed area. The third zone is the lateral plantar foot and is supplied by the dorsalis pedis and the lateral plantar arteries. The fourth zone is the distal foot that is supplied by the dorsalis pedis, the lateral plantar artery, and the medial plantar artery (5).
Taylor and Palmer (6) expanded the work of vascular anatomy by organizing this information into a cohesive whole and coined the term angiosomes. An angiosome is a block of tissue (skin, subcutaneous tissue, fascia, muscle, and bone) fed by a source artery. This vascular knowledge is important in incision placement when planning planter foot surgery, especially when dealing with flap closure for soft tissue defects. Attinger’s work in plantar incision planning is based on identifying the angiosomes supplying the operative area (7). His efforts were to maintain continuity of a vascular network when placing a plantar incision. This rational for incision placement based on angiosomes is reviewed later in the chapter.
The muscular anatomy of the plantar foot is composed of the plantar fascia as well as intrinsic and extrinsic muscles. The plantar fascia is located deep to the superficial fascia and is divided into three bands (medial, central, and lateral). It has strong attachments to the periosteum of the os calcis proximally and has envelopments distally to the plantar plate, plantar skin, and the fibrous wing and sling components of the digital areas (Fig. 41.2). The plantar fascia also sends fibrous bands deep between the plantar muscles known as the medial and lateral intramuscular septa. These bands divide the plantar musculature into three superficial compartments (medial, central, and lateral) and one deep interosseous compartment. The medial compartment contains the flexor hallucis brevis muscle and the abductor hallucis muscle. The central compartment is composed of the flexor digitorum brevis muscle, the quadratus plantae muscle, and the four lumbrical muscles. The lateral compartment contains the abductor digiti minimi muscle and the flexor digiti minimi brevis. The fourth compartment that lies deeper is called the interosseous compartment and includes the three plantar and four dorsal interosseous muscles of the foot (1). These compartments are important to understand when dealing with potential compartment syndrome patients or when dealing with plantar foot infections that commonly spread along the path of least resistance within these tissue planes.
The plantar musculature is often discussed anatomically by its four layers as opposed to its division into plantar compartments. The first layer contains the abductor hallucis, flexor digitorum brevis, and the abductor digiti minimi muscles. The second layer contains the quadratus plantae muscle and the four lumbrical muscles. The extrinsic tendons of the flexor hallucis longus and flexor digitorium longus also pass in this layer. The third layer consists of the flexor hallucis brevis, adductor hallucis, and the flexor digiti minimi brevis muscles. The fourth layer of plantar muscles consists of the plantar and dorsal interossei (1).
INDICATIONS
The most common procedures performed on the plantar aspect of the foot are for plantar fibroma excision, intermetatarsal neuroma excision (primary and recurrent), plantar fascial
ligament release, metatarsal head resection/panmetatarsal head resection, excision of integumental or soft tissue masses, plantar plate repair, sesamoid excision, and plastic closure of wounds (rotational or advancement flap closure). Other indications may arise out of necessity to perform plantar incisions depending on the situation at hand. Specific techniques of these procedures are covered elsewhere in this text. The plantar incision options will be reviewed for these procedures.
ligament release, metatarsal head resection/panmetatarsal head resection, excision of integumental or soft tissue masses, plantar plate repair, sesamoid excision, and plastic closure of wounds (rotational or advancement flap closure). Other indications may arise out of necessity to perform plantar incisions depending on the situation at hand. Specific techniques of these procedures are covered elsewhere in this text. The plantar incision options will be reviewed for these procedures.
INCISION PLACEMENT
Plantar foot incisions are commonly used out of necessity to access soft tissue masses like planter fibromas, excise planter foot lesions, remove foreign bodies, or for plastic closure of wounds. Plantar incisions can also be used electively to gain excellent exposure for interdigital neuroma excision, metatarsal phalangeal joint for plantar plate repair, sesamoid excision, plantarfascial ligament release, or metatarsal head resection procedures. Plantar foot incisions pose unique challenges to the surgeon because of the thickness of the skin, weight-bearing structures, and vascular anatomy. With a good understanding of the risks and benefits of this type of incisional approach, the surgeon can complete his desired results with success if appropriate care is taken.
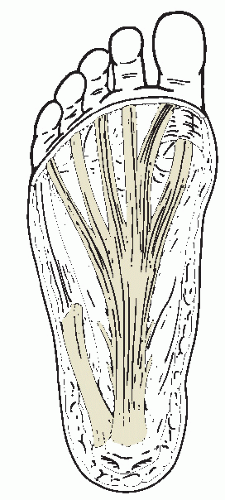 Figure 41.2 The plantar fascia is divided into three bands with strong attachment into the calcanus and distal attachment into the digits. Note the intermuscular septa between the plantar muscles. |
The goal of incision planning is to provide excellent exposure while leaving an aesthetically pleasing nonpainful scar while maintaining the functional integrity of the soft tissues. Knowledge of incision healing, functional anatomy, and the vascular supply to the plantar foot is paramount for an acceptable result.
Tissue handling via atraumatic technique as described by Bunuel must be utilized to limit the potential for painful scars on the plantar aspect of the foot (8). Gentle handling of the tissues produces less trauma and thereby tends to enhance healing and reduce scar formation. The thickness of the plantar skin along with the strong attachment of the underlying fibrous septae can create more difficulty with skin retraction and dissection; therefore, delicate tissue handling often is more challenging with plantar incisions (Fig. 41.3). Aggressive manipulation or retraction of plantar flaps can lead to partial- or full-thickness necrosis requiring subsequent surgery and potential need for free flaps and skin grafting (Fig. 41.4).
Appropriate skin closure technique is also important to prevent excessive scar formation. Due to the thickness of the plantar skin, everting the skin margins is essential to allow for a more anatomic wound. Utilizing horizontal or vertical mattress suture technique will assist in an optimal scar by keeping the epidermal layer away from the deeper dermal tissues, hence
preventing inclusion cyst formation and localized incision irritation and hypertrophy (Fig. 41.5).
preventing inclusion cyst formation and localized incision irritation and hypertrophy (Fig. 41.5).
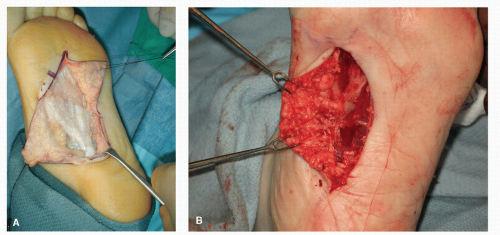 Figure 41.3 A: Note that the “no touch” technique via a single suture is utilized to retract the plantar flaps. (Courtesy of Gerard V. Yu.) B: An alternative method is to use single or double skin hooks to gently retract the flap.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|