Wound Complications
Yeukkei Cheung, Derek F. Amanatullah and Paul E. Di Cesare
Key Points
• Preoperative antibiotics can reduce the risk of wound infection.
• The diagnosis of deep infection is a critical decision in the course of treating an infected THA.
Introduction
Although managing the surgical wound is not the main goal of a total hip arthroplasty, it is critically important as prolonged postoperative surgical wound drainage has been associated with increased wound complications. Among the many potential causes of wound drainage include obesity, bleeding associated with various anti-coagulation regimens, and high closed suction drain output. Other factors that may be important include the nutritional status of the patient. The goal of this chapter is to provide the clinician with a practical guide to wound management including ways to avoid wound healing problems, guidelines to differentiate superficial from deeper wound problems, and strategies to manage the problematic wound.
Wound Drainage in Total Hip Arthroplasty
Understanding the potential causes of and methods to prevent wound drainage is important because prolonged postoperative surgical wound drainage has been associated with increased risk of deep infection, increased morbidity, and longer postoperative hospitalization after total hip arthroplasty (THA).1–3 No strict definition of “prolonged” or “persistent” wound drainage has been put forth. Some authors have defined prolonged or persistent wound drainage as wound drainage occurring or continuing 48 hours after the operative procedure.4 The overall incidence of superficial infection, defined as infection superficial to the fascia lata, in one series of 183 THAs was approximately 17%, and the overall incidence of deep wound infection within 6 weeks was slightly above 1%.5 However, the rate of deep wound infection increases from 1.3% to 50% with prolonged wound drainage.2,3,6,7
A retrospective review of 10,000 patients after THA or total knee arthroplasty (TKA) over a 5-year period identified 300 patients with wound drainage occurring more than 48 hours postoperatively.4 Persistent wound drainage stopped after 2 to 4 days in 217 patients (72.3%) when treated with a standardized initial treatment protocol of local wound care, which involved cleaning the wound with sterile saline solution followed by application of povidone-iodine solution and oral prophylactic antibiotics.
The remaining 83 patients (27.7%) with persistent wound drainage who failed the standardized protocol were treated with surgical irrigation and débridement performed 2 to 37 days postoperatively. Deep irrigation and débridement was performed when the deep fascia had not sealed. Surgical irrigation and débridement (performed 4 to 32 days postoperatively) was successful (no further intervention required) in 63 patients (75.9%). The remaining 20 patients (24.1%), who failed the initial surgical irrigation and débridement, were treated with removal of hardware, two-stage exchange arthroplasty with an antibiotic spacer, or long-term antibiotic suppression.4 Critical evaluation of the 83 patients necessitating surgical irrigation and débridement revealed that surgical irrigation and débridement was significantly more successful in patients who received surgical irrigation and débridement within 14 days from the index arthroplasty.4 In addition, an association was found between malnutrition (defined as serum transferrin less than 200 mg/dL, serum albumin less than 3.5 g/dL, or total lymphocyte count less than 1500 per mL) and failure of the initial surgical irrigation and débridement.4 All of the other variables evaluated, including age, gender, surgical blood loss, operative time, and diabetes mellitus, were not statistically significant risk factors for failure of initial surgical irrigation and débridement.
A similar retrospective study involving 1211 THAs identified risk factors associated with wound drainage 15 days after THA. Obesity (i.e., a body mass index greater than 35), use of low-molecular-weight heparin (LMWH) as venous thromboembolism prophylaxis, and high closed suction drain output were associated with prolonged wound drainage and higher rates of postoperative infection.1 It should be noted that in this study, use of LMWH was associated with earlier postoperative wound drainage compared with use of aspirin with intermittent compression devices or warfarin, but the time to a dry surgical wound between LMWH and warfarin equalized on postoperative day 8.
A meta-analysis comparing deep venous thrombosis prophylaxis with warfarin, low-dose unfractionated heparin, LMWH, and aspirin and pneumatic compression found that minor wound bleeding was greatest with LMWH and low-dose unfractionated heparin.8 However, LMWH does not requiring monitoring, hence its ease of use may outweigh the risk of a longer time to a dry surgical wound.9 Low-dose unfractionated heparin was also associated with a higher risk of major bleeding requiring surgical evacuation.8 Unfortunately, no randomized clinical trials have examined factor Xa inhibitors (e.g., fondaparinux) and their effects on surgical wound drainage. Appropriate deep vein thrombosis prophylaxis is important, and although many agents have been shown to be effective, some studies suggest that LMWH produces more wound drainage than Coumadin.
Use of a Closed Suction Drain
The routine use of a closed suction drain in THA remains controversial. Recent data demonstrate that rates of wound infection, postoperative hematoma, and reoperation are the same with or without a drain.10 One hypothesis is that a closed suction drain prevents hematoma formation, decreases wound tension, and subsequently prevents infection.10,11 Another hypothesis is that a closed suction drain may itself be a source of infection by acting as a conduit for entry of bacteria into the wound.12 A meta-analysis evaluating the use of closed suction drains during THA or TKA concluded that, although many studies have showed the pros and cons of closed suction drains, most lacked the appropriate methods or included an underpowered sample size.13 Often infection was used as a primary endpoint. However, the rate of infection after primary THA is low, hence most studies lack the power to support or refute the use of a closed suction drain in THA.
More recent data suggest that a closed suction drain does not decrease wound drainage, and that wounds without a closed suction drain require fewer dressing changes and dry faster.14,15 In one report, a high volume of closed suction drain output was correlated with prolonged wound drainage and a higher rate of postoperative infection in THA.1 Further, patients with a closed suction drain tended to require a greater number of postoperative blood transfusions.
One prospective study evaluated the effect of a closed suction drain on hematoma volume via nuclear medicine erythrocyte scintigraphy after THA.16 No statistically significant difference in volume of postoperative hematoma was noted after THA in either group at 22 hours. However, patients with closed suction drains had an increased need for postoperative blood transfusions. These studies show that it is important to tailor the placement of closed suction drains according to the needs of each individual, bearing in mind that data are available to support a higher rate of postoperative blood transfusion when closed suction drains are used, and that significant controversy continues about whether closed suction drains prevent infection after THA.
Early Plastic Surgery Consultation
Few studies have focused on the management of complex infected wounds (e.g., those with exposed endoprosthetic implants or bone) (Fig. 106-1A and B). In a retrospective review of 10 patients with infected THA wounds, early plastic surgery consultation was evaluated for the management of these complex wounds. Plastic surgery intervention within 5 to 7 days of the index THA resulted in endoprosthetic salvage in 6 of 10 (60%) THAs when a deep wound infection was present.17
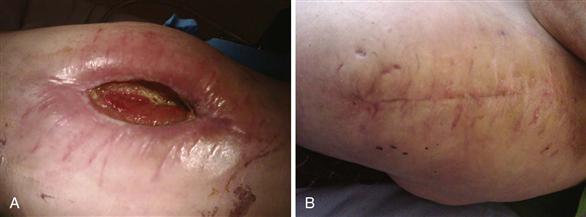
Figure 106-1 A, An example of an infected wound after total hip arthroplasty. B, Same wound after prosthesis removal and delayed primary closure.
Prior studies have supported the finding that early recognition, aggressive surgical irrigation and débridement, and stable wound coverage (primary or with a muscle flap) may result in endoprosthetic salvage.18–20 Vastus lateralis, rectus femoris, and rectus abdominis flaps have been advocated for coverage and salvage of THA.20–22 However, there remains no consensus regarding optimal management of an infected deep hip wound for endoprosthetic salvage. Although many wounds can be managed via local wound care, use of vacuum-assisted dressing, or delayed wound closure, muscular flaps remain an option because they enhance the blood supply to regional tissues, improving the delivery of antibiotics and reducing dead space.
Serum Markers of Malnutrition
It is important to recognize and identify malnourished patients preoperatively to optimize their postoperative wound healing potential. Many studies have shown that the process of postoperative wound healing is directly related to nutritional status (Fig. 106-2).4,23,24 Laboratory animals with protein malnutrition have less tensile wound strength, suggesting that protein malnutrition may increase the incidence of wound dehiscence in the early postoperative period.25 A prospective study evaluated the ability of serum albumin, serum transferrin, hematocrit, platelet count, prothrombin time (PT), partial thromboplastin time (PTT), erythrocyte sedimentation rate (ESR), and total lymphocyte count (TLC) to predict malnutrition and wound complications in 103 THAs. Low preoperative serum transferrin and albumin were observed in 34 (33.0%) patients with delayed wound healing. All measured nutritional markers were significantly lower in the immediate postoperative period. Each marker began to increase slowly on postoperative day 6. In the same study, patients who underwent single-stage, bilateral THAs had significantly lower serum transferrin and albumin levels on postoperative days 2, 4, and 6, and had higher rates of wound healing complications than patients who underwent unilateral THA.26
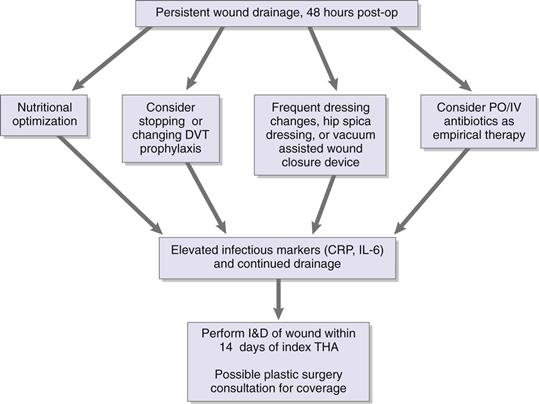
Figure 106-2 Treatment algorithm for persistent wound drainage. CRP, C-reactive protein; DVT, deep vein thrombosis; IL-6, interleukin-6; I&D, irrigation and débridement; postop, postoperatively; THA, total hip arthroplasty.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








