50
Volar Metacarpophalangeal Dislocations (Irreducible)
Benjamin Chang and Mark Katz
History and Clinical Presentation
A 17-year-old boy was grabbed by the left ring finger during an altercation and the finger was twisted. He noted immediate pain, swelling, and deviation of the finger. He came to the emergency department on the same day for treatment.
Physical Examination
The patient’s ring finger was ulnarly angulated, shortened, slightly hyperextended at the metacarpophalangeal (MP) joint, and flexed at the proximal interphalangeal (PIP) joint. There was no active motion at either joint. The skin was intact. The base of the proximal phalanx was prominently palpable in the palm and deviated to the radial side. Sensibility and capillary refill were normal. The remainder of the upper extremity was nontender.
Differential Diagnosis
Dislocation Volar MP joint
Simple
Complex Dorsal MP joint
Simple
Complex
Sprain of the MP joint
Fracture of the distal metacarpal
Fracture of the proximal phalanx
PEARLS
- If the mechanism is a hyperextension, then think an injury to the distal volar plate avulsion and plan a volar surgical approach
- If the mechanism is a hyperflexion, then suspect a proximal dorsal capsule interposition and plan a dorsal surgical approach
PITFALLS
- The digital nerves are displaced by the dislocation and are more prone to iatrogenic injury from the volar incision.
- Prolonged postoperative immobilization in the absence of a fracture is unnecessary and leads to stiff joints.
Diagnostic Studies
Radiographs of the hand revealed a fracture/dislocation of the MP joint with ulnar deviation of the ring finger and radial displacement of the base of the proximal phalanx on the posteroanterior view (Fig. 50–1). The lateral view clearly demonstrates the volar dislocation of the proximal phalanx relative to the metacarpal head (Fig. 50–2). An oblique view was also obtained.
Diagnosis
Volar Intraarticular Fracture/Dislocation of the Ring Finger MP Joint
The radial collateral ligament is presumably still attached to the small fracture fragment, but the ulnar collateral ligament must be completely disrupted to permit this degree of displacement.


Figure 50–2. Lateral radiograph of a complex volar fracture-dislocation of the left ring finger metacarpophalangeal joint.
The volar plate can be avulsed from the base of the proximal phalanx by hyperextension and become interposed in the MP joint, as in this case, trapping the proximal phalanx between the flexor tendons and the lumbrical. One may expect the more common dorsal dislocation with hyperextension, but Betz et al suggested that volar dislocation is produced when hyperextension force is applied to an actively flexing finger.
The dorsal joint capsule can be avulsed proximally from the metacarpal by hyperflexion and become interposed in the joint, thus blocking reduction. Wood and Dobyns have reproduced this injury in cadavers with hyperflexion and proximal translation. Hyperflexion force applied to the dorsum of the thumb proximal phalanx produces a tear of the dorsal capsule and herniation of the metacarpal head through the extensor aponeurosis between the extensor pollicis longus on the ulnar side and the extensor pollicis brevis on the radial side. The extensor aponeurosis is then trapped volar to the metacarpal head, preventing its reduction.
Surgical Management
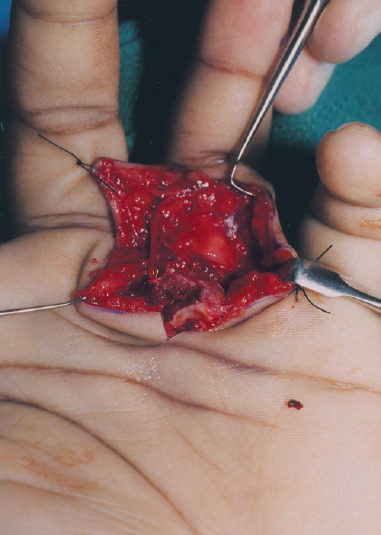
Closed reduction under general anesthesia was attempted in the operating room on the day of injury but was unsuccessful. Open reduction was performed through a volar zigzag incision over the ring finger metacarpal extending up to the PIP flexion crease. The digital neurovascular bundles were identified and retracted. The base of the proximal phalanx was found to be displaced volar and radial to the flexor tendons. There was an articular fragment missing from the radial base of the proximal phalanx (Fig. 50–3). The volar plate and collateral ligaments were no longer attached to the proximal phalanx, but were found dorsal to the proximal phalanx. The base of the proximal phalanx was trapped between the flexor tendons on the ulnar side, the lumbrical on the radial side, and the volar plate on the dorsal side.
The A1 pulley was incised and the flexor tendons returned to their normal position volar to the proximal phalanx. The base of the phalanx was then easily reduced. An interosseous wire was placed through drill holes to secure the fracture fragment to the base of the phalanx, restoring anatomic alignment (Fig. 50–4). The volar plate was reattached to the proximal phalanx with 4–0 Prolene passed through the periosteum and flexor tendon sheath at the lateral edges of the A2 pulley. After reduction and repair, the MP joint was stable through a passive range of motion between 0 and 90 degrees of flexion.
After skin closure, a short arm cast was applied with the wrist in slight extension, the MP joints in flexion and the PIP joints fully extended.
Postoperative Management
The cast remained in place for 3 weeks. Gentle active range of motion commenced at 3 weeks. The patient began passive range of motion, blocking, and strengthening at 6 weeks. At 3 months, the patient had full active motion at the interphalangeal joints and −15/80 degrees at the MP joint of the ring finger.