40
Proximal Phalangeal Condylar Fractures
Carrie R. Swigart
History and Clinical Presentation
A 53-year-old right hand dominant man slipped and fell, striking his left fifth digit. He initially thought little of it, and it was not until later that day, while he was working with some tires and caught his left small finger, that he noticed pain and swelling of the digit. After initial consultation with an orthopedic surgeon, he was referred to a hand surgeon 6 days after injury.
Physical Examination
There was circumferential swelling of the digit. The finger angulated dorsally at the level of the distal portion of the proximal phalanx. No rotation deformity was noted, although the patient was unable to completely flex the digit. Profundus and sublimis tendon function was intact, as was the neurovascular status. The patient was otherwise in good health. He had had cardiac bypass surgery, but had no current complaints of exertional angina. His only medication was Dilantin.
Diagnostic Studies
Radiographs of the left small finger showed a comminuted fracture of the distal portion of the proximal phalanx. The fracture was slightly shortened and angulated dorsally ∼35 degrees. There was no apparent intraarticular involvement (Fig. 40–1).
PEARLS
- Careful preparation and planning are mandatory for successful use of the minicondylar plate.
- If rigid fixation is not likely to be attainable, closed or percutaneous methods must be considered.
PITFALLS
- Careful attention to rotation alignment is critical.
- The initial condylar K-wire placement has little to no margin for error.
- Additional soft tissue disruption complicated by insufficient stability can be disastrous.
Diagnosis
Unstable Comminuted Fracture of the Proximal Phalanx, Small Finger, Nondominant Hand
This is an unstable fracture pattern due to both the comminution and the obliquity of the fracture.
Comminuted, unstable fractures of the phalanges, especially about the proximal interphalangeal (PIP) joint, are difficult to treat and often result in limitations of motion and function, regardless of the treatment chosen. If open reduction is attempted, it is imperative that the fracture be rigidly fixed to allow for early range of motion. Operative fixation should be done on an urgent basis, ideally within the first 10 days to 2 weeks after the fracture.
Surgical Management
After the physician reviewed the preoperative blood work, including the Dilantin level, the patient was taken to the operating room on an elective basis, 11 days after sustaining the fracture. A Bier block anesthetic was used as a peripheral adjunct to general anesthesia. The patient was placed in the supine position with the left upper extremity on a hand table. The tourniquet, used for both the Bier block and hemostasis, was placed on the upper arm. It was inflated to 250 mm Hg.

Figure 40–1. Lateral (A) and anteroposterior (AP) (B) radiographs of the fracture showing marked apex palmar angulation and comminution.
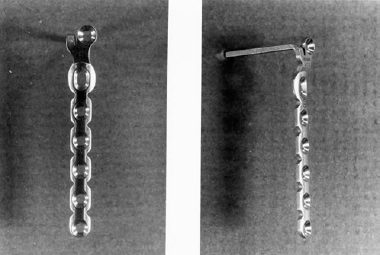
Due to the intercondylar fracture pattern, a minicondylar blade plate was selected as the implant. Because of the size of the phalanx, a 1.5-mm plate was chosen (Fig. 40–2). The first step in applying the plate was to pass a 0.045-inch Kirschner wire (K wire) distally across the condyles in the location of the future condylar screw (Fig. 40–3A). Its position was carefully checked in the anteroposterior (AP) and lateral planes with a minifluoroscopy unit. A preliminary reduction of the fracture was performed so that the appropriate length for the minicondylar plate could be assessed. This plate was then bent to match the lateral contour of the phalanx and trimmed to size. The blade of the plate was also trimmed to fit the AP dimension of the condyles. The blade of the plate was then inserted by first drilling a 1.5-mm hole adjacent and parallel to the K wire (Fig. 40–3B). The blade of the plate was then inserted, slipping the previously placed K wire through the hole for the condylar screw (Fig. 40–3C). The adjacent condylar screw was then placed, obtaining bicortical purchase (Fig. 40–3D). Once the condylar fragment was attached to the plate, the fracture was reduced. Due to the high degree of comminution, an anatomically keyed reduction could not be obtained. The fragments were aligned with maximal apposition of the fractured surfaces. Rotation was carefully checked during fragment alignment. The most proximal 1.5-mm screw was placed next, thus holding the fracture aligned and reduced with appropriate length of the proximal phalanx. The subsequent three screws were then carefully placed to rigidly stabilize the fracture (Fig. 40–3E).