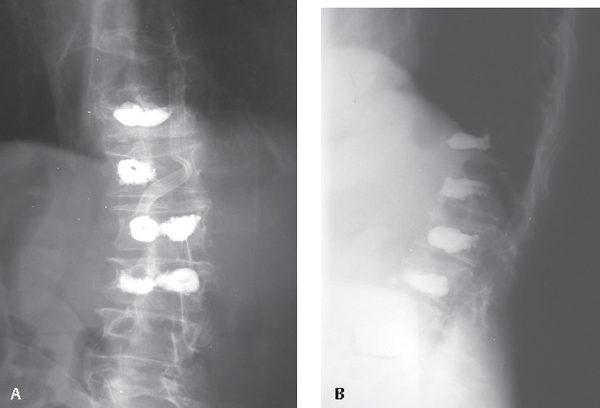
54 There are over 700,000 osteoporotic vertebral compression fractures (VCFs) each year in the United States, making this a major health concern. Although many patients respond to bracing, there is a subpopulation of those with VCFs who are not adequately treated with nonoperative care and for whom traditional open surgery is overly invasive. These patients may be helped by a percutaneous vertebral augmentation procedure. These procedures are able to achieve rapid pain relief in most patients, with a relatively low overall complication rate. Both vertebroplasty and kyphoplasty involve the injection of polymethylmethacrylate (PMMA) into the compressed vertebral body. In contrast to vertebroplasty, kyphoplasty first utilizes an inflatable bone tamp to make a space for the cement, and in some cases, it can help to restore vertebral body height (Fig. 54.1). Vertebroplasty and kyphoplasty are both indicated for the treatment of patients with VCFs who are experiencing severe, unmanageable pain or progressive deformity. These procedures have also been shown to have a role in the management of certain painful, osteolytic VCFs. Contraindications include any systemic pathology, such as sepsis or an anticoagulated state. Relative contraindications include nonosteolytic infiltrative spinal metastases, vertebral bodies with deficient posterior cortices (burst fractures), or patients presenting with a neurologic deficit. The onset, duration, location, and character of the patient’s pain/injury should be clearly understood. Pain related to other spinal issues, such as spondylolisthesis, will not benefit from cement augmentation, and an attempt should be made to exclude patients with other painful processes. It is also important for the physician to ensure that the underlying osteoporosis is diagnosed and treated. Fig. 54.1 Plain radiographs demonstrating vertebral compression fractures after correction with kyphoplasty. (A) Anteroposterior. (B) Lateral. In addition to a complete neurologic exam, the spine should be palpated or percussed over the fracture site to confirm direct tenderness. Symptoms may be shown to increase with upright positioning (as opposed to recumbency) or worsen with gentle range of motion. Radiographs and magnetic resonance imaging (MRI) are generally used to diagnose the fracture. The MRI can help to determine the acuity of the fracture by showing edema at the fracture site. The MRI should be carefully studied to rule out any findings of metastatic disease or burst component to the fracture. In cases where the diagnosis or fracture pattern is unclear, nuclear bone scans or computed tomography (CT) scans can be useful.
Vertebroplasty and Kyphoplasty
![]() Classification
Classification
![]() Workup
Workup
History
Physical Examination
Spinal Imaging
Special Diagnostic Tests
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






