Upper extremity pain is a leading cause of physician visits in the United States. This is particularly prevalent in sports and the workplace, contributing significantly to disability and lost productivity. Along the spectrum of potential conditions, musculoskeletal soft-tissue injuries are the most common. Despite a wealth of investigations on soft-tissue injury, there remains an incomplete understanding of what these injuries are and the sequence of events leading to their development. A detailed understanding of the relevant functional anatomy and potential mechanisms of injury allows for the most accurate diagnosis and is directly related to the likelihood of successful treatment. This chapter describes a classification of soft-tissue injury, identifies potential mechanisms of injury, and presents a model for successful rehabilitation. Injuries specific to the shoulder and elbow are considered.
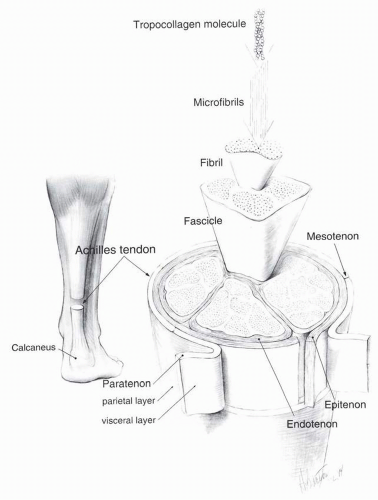
The soft tissues constitute a diverse group of connective tissues, including ligament, tendon, muscle, cartilage, fascia, synovium, articular cartilage, adipose tissue, and intervertebral disc. Collectively, connective tissues function as support for the soft tissues, transmit and distribute mechanical forces, and act as a conduit for neurovascular structures. They are composed of collagen fibers; ground substance, primarily in the form of proteoglycans and water; and specialized cellular components. Although the connective tissues share common structural features, each has unique cellular and biomechanical properties and, therefore, demonstrates individual responses to injury and healing (
1). Loose connective tissue, for example, is poorly organized and typically seen in subcutaneous tissue, small joint capsules, and fascial borders. Tendons and ligaments are composed of dense, organized connective tissue, with a larger proportion of collagen fibers arranged according to their biomechanical requirements (
2) (
Fig. 35-1). Tendons, in particular, are subjected to great tensile stress because they function to transmit force from muscle to bone. The tensile strength of tendon is generally double that of its associated muscle (
3,
4). This likely accounts for the greater incidence of injury at musculotendinous junctions. There are numerous factors influencing the integrity of soft tissues, including age, sex, temperature, body weight, exercise, nutrition, drugs, immobilization, injury, and systemic illnesses such as inflammatory arthritis and the collagen vascular disorders.
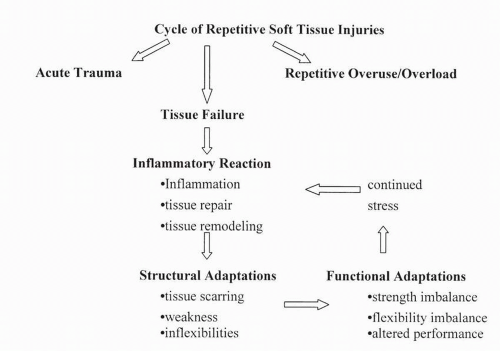
Soft tissues are susceptible to failure under conditions of stress and strain. The most common mechanisms of injury include acute trauma and repetitive overuse or overload. Musculotendinous structures are especially vulnerable to failure from sudden overloading, as with forceful muscular contractions, particularly when weakened as a result of concurrent illness (connective tissue disorders) or medications (steroids). More commonly, repetitive overuse leads to an insidious onset of pain, inflammation, and ultimately, structural failure. In the context of persistent or uncontrolled stress, a cycle may occur in which structural maladaptations develop in the damaged tissue, setting the stage for further injury and chronic inflammation (
Fig. 35-2).
The three phases of soft-tissue healing include the cellular response to injury; repair and regeneration, as immature collagen is laid down; and scar remodeling, a process that may continue for years (
5). Understanding this sequence of events has direct implications on the success of treatment and rehabilitation. The type of injury, age, vascularity, nutrition, genetic and hormonal factors, and activity level influence successful healing of soft tissues. Acute injuries typically have a sudden onset, are associated with a classic inflammatory reaction, and tend to follow a predictable course toward resolution. Chronic injuries (duration longer than 3 months) are often marked by an insidious onset of pain, less intense inflammation, progressive functional impairments, and a tendency toward reinjury. Advanced age is associated with decreased collagen synthesis and impaired tendon healing. Exercise improves both the mechanical and structural properties of tendon as opposed to inactivity, which favors collagen degradation and decreased tendon strength.
The nature and classification of soft-tissue injury, as well as the injury response, are specific to the involved structure (
1). Ligament sprains have been classically defined as grade I, II, and III based on the degree of tissue damage and separation (
Table 35-1). Grade I sprains demonstrate negligible loss of structural integrity, display minimal signs of inflammation, and generally recover quickly and completely. In grade II sprains, partial rupture of the ligament is associated with significant pain and inflammation. Functional recovery generally occurs within 4 to 6 weeks; however, pain is often experienced for months after the injury, and the tensile strength of the involved tissue is reduced up to 50% (
6). Grade III injuries are often associated with prolonged healing time, chronic instability, susceptibility to recurrent sprains, and impaired proprioception of the involved joint.
Tendons are susceptible to injury through the same mechanisms of tensile overload and repetitive overuse (
7,
8). Tendons are particularly vulnerable to failure when tension is applied quickly or obliquely, the tendon is tense before trauma, the
attached muscle is maximally innervated, the muscle group is stretched by external stimuli, and the tendon is weak in comparison to its muscle (
9). Tendon injuries, or tendinopathies, can be classified according to a sequence of overlapping pathologic conditions: inflammation, degeneration, and rupture (
Table 35-2). Paratenonitis refers to inflammation of the paratenon. When the structure is associated with a synovial lining, the condition is described as tenosynovitis. The term
tendinitis refers to injuries and inflammation specifically involving tendon.
Tendinosis describes a chronic process of intratendinous degeneration and atrophy, minimal or no inflammation, and loss of structural integrity, potentially leading to tendon failure (
10,
11,
12). Inflammation of the paratenon may occur concomitantly with tendon atrophy, referred to as paratenonitis with tendinosis. A functional classification of traumatic tendinitis is particularly useful because the degree of disability correlates well with the extent of injury (
Table 35-3). This grading system also provides objective parameters for following treatment and rehabilitation.
Muscular injuries are particularly common in sports. These are typically classified as contusions, strains, avulsions, and delayed-onset muscle soreness. Contusions result as a direct blow and are graded as mild, moderate, or severe based on the degree of soft-tissue swelling, motion restriction, and functional impairment. Intramuscular contusions tend to be more severe, resolve slowly, have more extensive scarring, and are susceptible to developing myositis ossificans (
13,
14,
15,
16). Muscular strains result from overstretching or peak contraction of the musculotendinous unit, particularly during eccentric muscular contractions. These injuries tend to occur more commonly at the musculotendinous junction. The classification is similar to that of muscular contusions.
The injured muscle generates reduced peak tensile loads and contractile forces, up to 50% of its strength. Contractile forces begin to recover as soon as 1 week after an acute strain; however, there is often prolonged and sometimes permanent loss of complete contractile ability (
17,
18,
19). Therefore, the functional ability of a patient recovering from a muscular strain may be significantly limited, and premature return to activity may increase the risk for further injury. Delayed-onset muscle soreness typically occurs within the first 24 to 48 hours after an intense bout of exercise that often involves repeated eccentric muscular contractions. Both inflammatory and metabolic mechanisms have been proposed for muscle damage in this condition (
20,
21). In most cases, the condition is self-limiting but occasionally requires activity modification and antiinflammatory medication.
It is useful to approach the treatment and rehabilitation of soft-tissue injuries through a conceptual framework that begins with establishing the most anatomically correct diagnosis and ultimately returns the patient to normal athletic or occupational performance (
22,
23,
24,
25,
26) (
Table 35-4). Protecting the injured site and controlling pain and inflammation set the stage for an active therapy program geared toward improving the flexibility, strength, and endurance of the damaged tissue and entire kinetic chain. This also takes into account other factors that may be associated with the development and persistence of symptoms (
Table 35-5).
SOFT-TISSUE INJURIES OF THE SHOULDER
Two primary factors make the shoulder joint particularly susceptible to soft-tissue injuries. First, the surrounding soft tissues constitute the main support system for the upper extremity. Second, the small glenoid fossa allows for a large range of motion that often permits excessive mobility, thereby straining the soft tissues and stressing the joint. Injuries of the shoulder can be broadly classified as those that result from more acute processes, such as direct trauma, and those that occur from more repetitive tasks, such as bursitis and tendonitis. Overall, shoulder injuries are so common that they are second only to back injuries in disability costs associated with lost time (
27). Understanding the complex anatomy and kinesiology of the shoulder is essential for accurate diagnosis and appropriate treatment.
Anatomy of the Shoulder
The shoulder is composed of many joints, including the scapulothoracic joint, which is considered a functional joint. The glenohumeral joint is a synovial joint lined by the glenoid labrum, which provides a large contact surface to the glenoid fossa. Despite the large labrum, the humeral head comes into contact with only about one third of the glenoid fossa at any one time (
28). The capsule of the glenohumeral joint is divided into three functional bands that are considered ligaments, aptly named the superior (SGHL), middle (MGHL), and inferior glenohumeral (IGHL) ligaments. Additional support is provided by the coracohumeral ligament (CHL) originating on the coracoid and inserting into the greater and lesser tuberosities. The acromioclavicular (AC) joint is another synovial joint made up of the distal aspect of the clavicle and the
acromion and is supported by the coracoacromial ligament, the AC ligament, and the coracoclavicular (CC) ligament (composed of two smaller ligaments—the conoid and the trapezoid). Motion at the AC joint requires not only translation but also rotation for smooth movement of the shoulder. The last synovial joint involved in the shoulder is the sternoclavicular joint. The joint is bordered by the medial aspect of the clavicle and the manubrium of the sternum. There are four ligaments surrounding the joint: the anterior and posterior sternoclavicular ligaments, the costoclavicular ligament, and the interclavicular ligament.
The muscles of the shoulder and shoulder girdle can be divided into two major groups: those that stabilize the scapula and those that attach to the humerus. The stabilizers include the trapezius, levator scapula, rhomboids, serratus anterior, and pectoralis minor. These muscles allow for the stability of the shoulder girdle and provide a foundation for movement and force generation that is passed along the trunk into the arm for functional use. The muscles that attach to the humerus include the rotator cuff muscles (supraspinatus, infraspinatus, teres minor, and subscapularis), deltoid, teres major, pectoralis major, coracobrachialis, biceps brachii, and latissimus dorsi. These muscles provide the arm with most of its motion.
Kinesiology of the Shoulder
Range of motion of the shoulder is accomplished by glenohumeral and scapulothoracic motions. The first 30 degrees of abduction is initiated by the deltoid muscle followed by a 2:1 ratio of movement, with the glenohumeral joint responsible for 120 degrees and the scapulothoracic motion supplying the additional 60 degrees. The humerus, however, needs to be in an externally rotated position to be able to obtain full abduction; otherwise, the tuberosity on the humerus impinges on the undersurface of the acromion.
Several authors have evaluated the kinematics of the scapula and its interaction with the humerus. Borstad and Ludewig (
29) looked at scapular motion in both symptomatic and asymptomatic individuals. Through electromagnetic tracking, they were able to evaluate scapular tipping and internal rotation. They noted that in symptomatic individuals there was less upward rotation at lower humeral elevations and increased tipping at higher elevations when compared to controls. These same scapular changes were also noted in patients with multidirectional instability (
30). There does not appear to be consistent findings with glenohumeral motion (
31).
The muscles noted previously can be divided into functional groups. For example, internal rotation is accomplished by the subscapularis, latissimus dorsi, anterior fiber of the deltoid, pectoralis major, and teres major. External rotators include the infraspinatus, teres minor, and posterior fibers of the deltoid. Abductors include the deltoid, supraspinatus, trapezius, and serratus anterior. Adduction is accomplished by the subscapularis, infraspinatus, teres minor, pectoralis, latissimus dorsi, and teres major. Flexion of the arm involves the pectoralis major, biceps brachii, and anterior deltoid. Extension is accomplished by posterior deltoid, teres major, and latissimus dorsi. Some muscles may contribute to motion based on the initial position of the humerus. For example, if the humerus is in a flexed position, the pectoralis may assist in early extension to the neutral plane.
Disorders of the Shoulder
Contusion and Myositis
Contusions are a result of blunt trauma to the soft tissue and may be difficult to differentiate from tears because both involve a significant amount of injury to the muscle fiber. Contusions can be divided into intermuscular and intramuscular types. Diagnostically, ultrasound or magnetic resonance imaging (MRI) may be helpful in determining the location of the injury. This may have clinical value because contusions and hematomas occurring between the muscles tend to disperse more easily along the fascial plains and result in an earlier return to function. Intramuscular lesions take longer to resolve because they are confined, and the inflammatory response is greater. These injuries also have a higher incidence of compartment syndrome (rare) and myositis ossificans associated with them. Myositis ossificans is the invasion of calcium and bony islands within the muscle. This process is usually accompanied by erythema, swelling, and a significant amount of pain. Radiographs early in the process may not reveal the ossification. If a compartment syndrome is suspected, release and drainage are critical to prevent long-term injury to the neurovascular structures.
Instability
Laxity of the shoulder joint varies tremendously between individuals. A certain amount of laxity or movement of the joint is normal; this translation is needed for the joint to have the mobility and function that it needs. Laxity is also noted to be present in most asymptomatic adolescents and decreases with age (
32). Instability as a pathologic process should only be explored if there are symptoms that correlate to the degree of motion noted at the joint. The labrum contributes to about 20% of the glenohumeral stability with the joint loaded (
33). Anterior stability is maintained not only through the forces at the labrum and rotator cuff muscles but also along the capsule particularly at the MGHL and IGHL. The anterior forces when the arm is abducted 90 degrees are mainly counteracted by the IGHL. At angles closer to the body, the MGHL plays a larger role. Most dislocations occur in an anterior plane when the arm is abducted, thereby indicating that the area most likely to be involved in a traumatic dislocation is the IGHL (
34). Posterior translation of the joint is significantly less common. The positions of the humerus that place the joint at greatest risk are flexion, adduction, and internal rotation. In this position, failure of several soft tissues is still required for dislocation to occur. The ligamentous capsule on the posterior aspect of the glenohumeral joint is underdeveloped; therefore, the support appears to be a combination of the anatomic position of the glenoid and the nearby SGHL, IGHL, and CHL along with the rotator cuff muscles themselves. Inferior translation is noted in the neutral
position by the sulcus sign. As stated earlier, a certain degree of laxity is normal. The counteractive force of inferior translation in the neutral position is mainly provided by the SGHL and the CHL. As the arm is abducted, the resistive force at the IGHL is increased and is related to the amount of abduction. If the arm is also internally rotated, additional force is placed on this ligament. Superior translation is clinically insignificant because of the bony structure of the acromion.
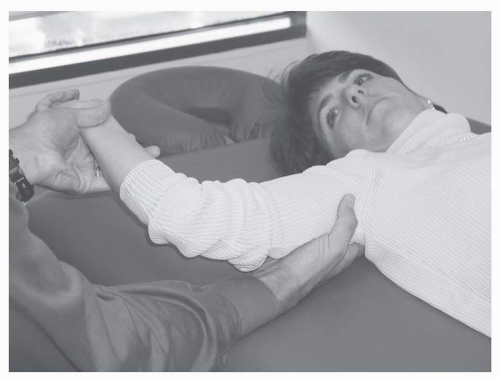
Diagnosis of instability relies on the history and reproduction of symptoms with specific physical maneuvers. An apprehension maneuver is typically completed in the supine position, and anterior translation-type forces are applied to the humerus with the arm abducted to 90 degrees and externally rotated. A positive test is noted with pain and fear of subluxation expressed by the patient (
Fig. 35-3). A relocation maneuver is also helpful to confirm the diagnosis. This is accomplished by a posterior force applied on the humerus with a reduction in symptoms or additional motion allowed in external rotation with a reduction in pain. Diagnostic tests that may be helpful include a scapular Y film and an axillary view for anteroposterior location of the humerus in relation to the glenoid.
Acromioclavicular Joint Sprain
AC joint sprain usually occurs from a fall on an outstretched arm or a direct blow to the shoulder. Pain over the joint and increased joint mobility is frequently noted and may help to guide the diagnosis. In addition, there is pain noted on crossed adduction from compression of the joint and in the end range of abduction from the pull of the deltoid and trapezius. Typically, the diagnosis can be made clinically, but in some cases, an x-ray with a weighted view may be helpful. If gapping of the joint is seen, it can support the diagnosis. However, it should be noted that a negative x-ray does not preclude the diagnosis. AC joint strain and separations are divided into grades. Grade 1 is defined as pain at the joint; however, the ligaments are intact, and there is no subluxation of the joint. Grade 2 is movement of the joint related to a tear in the AC ligament but not in the CC ligaments. Grade 3 indicates a tear through both AC and CC ligaments. Grades 4 to 6 are defined by displacement of the clavicle posteriorly, superiorly, and anteriorly, respectively. In addition, grade 6 displacement involves entrapment of the distal clavicle in the surrounding muscles. Typically, grades 1 to 3 are treated conservatively, whereas grades 4 to 6 require reconstruction. Reconstruction can also be considered in individuals with persistent pain from a grade 3 injury. Treatment of a grade 1 separation would include ice, sling and swath, or resting of the arm for a short period of time. Range of motion is progressed as tolerated, the supporting musculature is strengthened, and weight loading of the joint is avoided for about 6 weeks. A grade 2 injury requires a slightly longer rest period (up to 2 weeks) before returning to range and strengthening activities. Grade 3 injuries do not require surgical reconstruction. Although there may be some controversy regarding nonsurgical management of these injuries, there are several studies that have demonstrated good outcomes with conservative treatment, and one study showed an earlier return to work and play when compared with the surgically treated group (
35,
36,
37,
38). Grades 4 to 6 are still thought to do better with surgical intervention.
Bicipital Tendonitis
Activation of the biceps muscle is noted with elbow flexion and supination of the forearm. There is also some activity with abduction of the arm in an externally rotated position. The long head of the biceps is integrally linked to shoulder function and may assist the rotator cuff muscles with counteracting anterior and superior forces at the humerus. Its origin is at the supraglenoid tubercle and the adjacent labrum. It courses within the capsule and along the bicipital groove between the tubercles and is held in place by the transverse ligament. The biceps tendon is frequently involved with rotator cuff pathology and anterior laxity of the humerus. Tendinitis is common and usually associated with overhead activities. Clinically, palpation of the tendon and pain produced with resisted supination while the elbow is flexed and held against the trunk (Yergason’s test) or with resistance of forward flexion with the elbow extended and supinated (Speed’s test) are indicative of tendonitis (
Table 35-6). The tendon has been noted to be swollen, stenotic at the transverse ligament, and frequently hemorrhagic. In addition, adhesions may develop in the area with ongoing inflammation. If the transverse ligament is lax or ruptured, the biceps tendon can sublux. This can be palpated, and the patient frequently reports a snapping sensation. Rupture of the tendon most commonly affects the proximal portion of the long head. Symptoms range from discomfort and weakness to a painful snap. Surgical intervention is considered in young, active individuals. Mariani and Cofield (
39) evaluated conservative versus surgical intervention and noted the following: there was no difference in residual pain, elbow motion, strength of elbow extension, forearm pronation, or grip strength; the nonsurgical group usually returned
to activities, including work, more rapidly, albeit initially at a reduced capacity; and there was usually an associated loss of strength with elbow flexion (10%) and supination (20%), and many individuals were aware of this weakness. Therefore, if the patient is a young and active individual, surgical consultation is generally recommended.