and the other spinal deformities are not uncommon. The prevalence of idiopathic scoliosis is reported to be between 0.3% and 2% of the population (9). The incidence of degenerative scoliosis is reported as 6% in people over 50 years of age and 36% in persons over 50 with osteoporosis (10). Scheuermann’s disease, a common cause of pathological thoracic kyphosis, has a prevalence of between 0.4% and 8.3% of the population. Up to a 100% incidence of spinal deformity can be found in people with many neuromuscular conditions (see section on “Neuromuscular Scoliosis”).
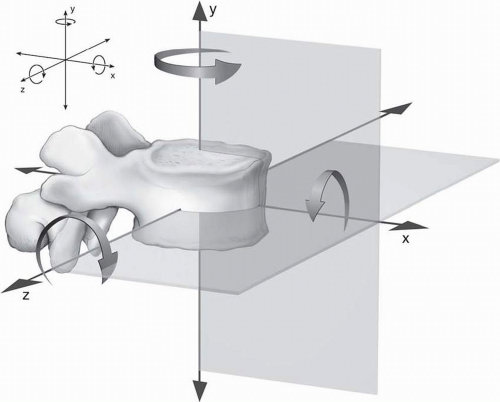
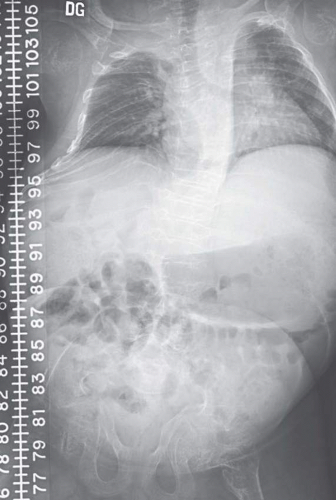
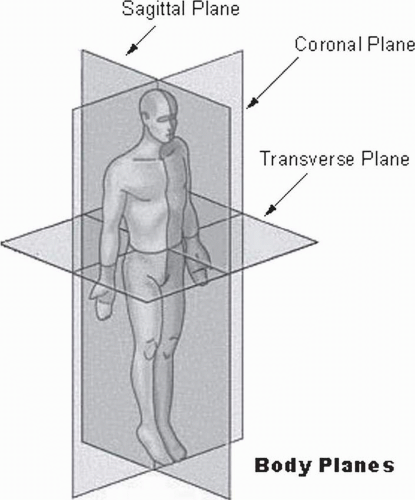 FIGURE 34-1. The planes of the body. (Courtesy of National Cancer Institute’s SEER Program web-based training module.) |
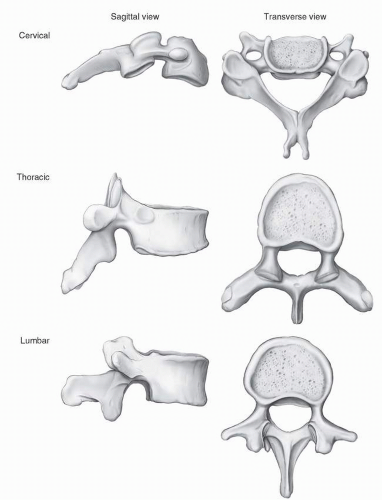
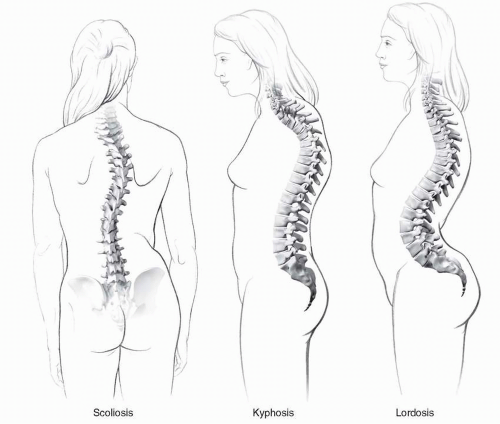 FIGURE 34-2. There are three basic types of pathological spinal curves. (Courtesy of Donald Bliss and Alan Hoofring of the Medical Arts and Publications Branch, NIH.) |
and their families. By persevering through the remainder of this chapter, you will have the chance to
TABLE 34.1 Types of Scoliosis and Typical Ages of Onset | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Regain sufficient memory of the anatomy and physiology underlying the balance of the spine in order to appreciate the factors contributing to the various spinal deformity pathologies and to have a basis to develop a rational treatment plan
Understand how to obtain the crucial historical, clinical, and radiographic data to form an educated diagnosis and prognosis
Appreciate the impact of spinal deformity on a person’s quality of life
Understand the pathophysiology and etiologies of spinal deformity
Understand the roles of physiatric modalities in the (re) habilitation of persons with spinal deformity
Understand the role of surgical treatment
Consider the issues involved in postsurgical rehabilitation
the vertebral body, there is a similar ligament, the posterior longitudinal ligament. However, it has an hourglass shape and is thinner than the anterior ligament. There are also three ligaments which connect portions of the posterior column of the spine. The supraspinous ligament stretches across the tips of the spinous processes while the interspinous ligaments stretch from one spinous process to the next. The ligamenta flava (flava is Latin for yellow and the ligament is that color due to the high proportion of elastic tissue within it) connect the laminae of adjacent vertebrae from the anterior surface of the proximal lamina to the posterior surface of the distal lamina. They also blend in with the capsule of the zygopophyseal joints.
allow limited movement in all six directions, although each individual joint only moves to a small degree. The zygopophyseal joints are the only true synovial joints in the spine and are found at the junction of the pedicle with the lamina. The form of their alignment contributes significantly to the functional movement at different levels. The transverse alignment in the neck permits good flexibility in all planes. In the thoracic spine, the facets are aligned frontally which, along with the linkage to the rib cage, limits flexion and extension. The lumbar facets are arranged sagittally, limiting lateral rotation.
is a validated instrument focused specifically on persons with spinal deformity (14, 15, 16). Alternatively, one of the many generic “disability/burden of care” or “health-related quality of life” instruments may be used (see Chapters 11 and 18).
symmetry should be viewed at the level of the acromioclavicular joint (13). Pelvic symmetry can be viewed either at the brim of the pelvis at the iliac crests or at the posterior superior iliac spines, which is seen on the surface of the buttocks as the two sacral “dimples.”
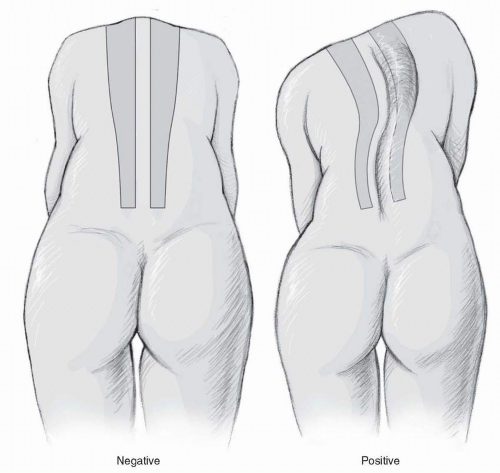 FIGURE 34-5. Adam’s forward bending test. (Courtesy of Donald Bliss and Alan Hoofring of the Medical Arts and Publications Branch, NIH.) |
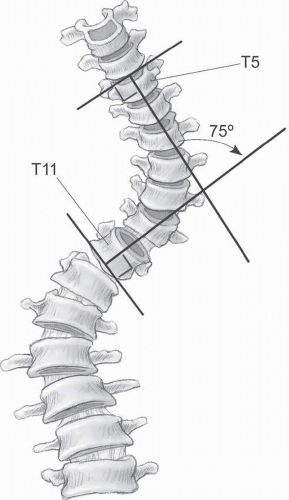
reliability similar to the film-based method (24, 25, 26). More recently, some systems have introduced fully automated Cobb angle calculations. However, it appears that this technology still requires further refinement to achieve adequate accuracy for curves of all magnitudes (27).
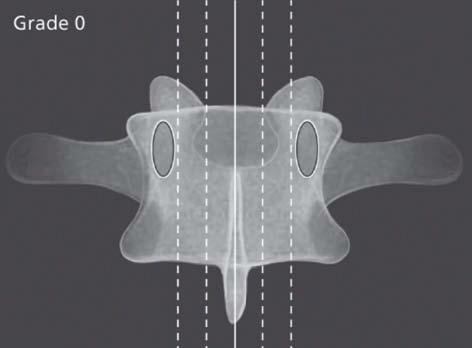
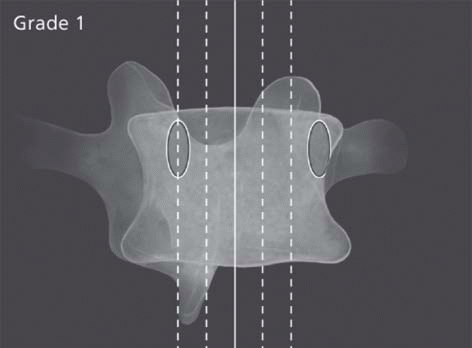
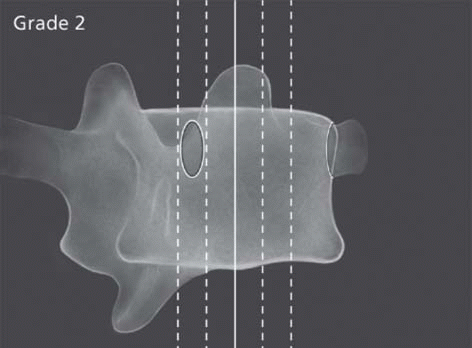
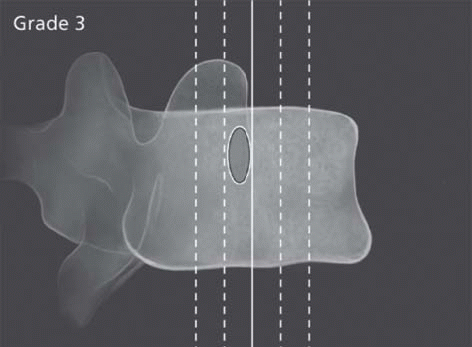
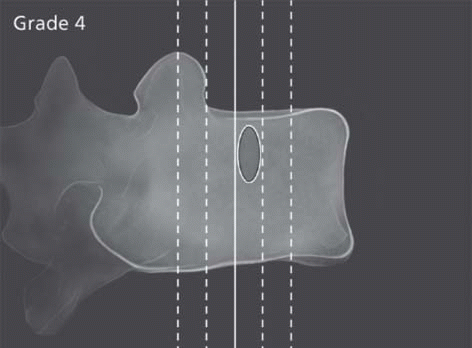
TABLE 34.2 Moe-Nash Classification of Spinal Rotation | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
three-dimensional CT may be useful, especially in congenital disorders (30, 31). MRI might offer similar information without radiation exposure (although still with the need for sedation in groups including young children and adults with claustrophobia); however, at the current state of technology, recommendations for its use are still limited to ruling out potential etiologies or neurological abnormalities (32). It is also important to remember that neither CT nor MRI is able to assess the impact of gravity on a curve, since both studies are done in a supine position.
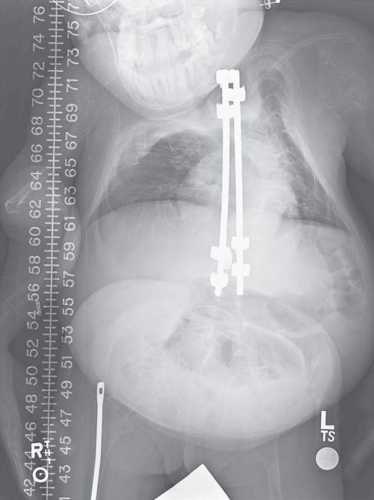 FIGURE 34-7. Rib asymmetry associated with spinal deformity in an adolescent girl with osteogenesis imperfecta. (Courtesy of Department of Imaging Sciences, Warren G. Magnuson Clinical Center, NIH.) |
tumors, the delay between the onset of symptoms and the diagnosis can be up to 19 months. In malignant tumors, it can be up to 4 months between symptom onset and diagnosis. It is important to recall that tumor-related pain is often worse at night and is disassociated from any obvious initiating or exacerbating factors (35).
acquired? If it is acquired, is the etiology traumatic, infectious, neoplastic, autoimmune, or degenerative? Understanding the biology of the dysfunction is important, that is, is the problem due to a metabolic defect in the tissue or is the tissue reacting to an outside influence. The nature of how these systems interact should also be considered. For example, does the elastic pathology cause secondary bony deformity?
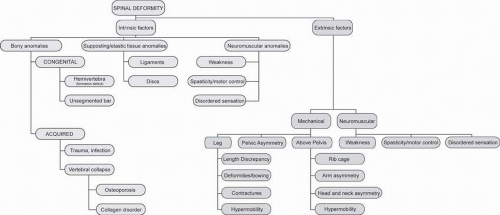 FIGURE 34-9. Pathological factors contributing to spinal deformities. (Courtesy of Donald Bliss and Alan Hoofring of the Medical Arts and Publications Branch, NIH.) |
progression and 15% show no progression (46). The character of the curve will help determine likelihood of success of a given treatment approach. Long, flexible curves may respond to orthotic management. Short, stiff curves will require surgery if they progress.
TABLE 34.3 Classification of Scoliosis Based on the SRS Taxonomy | |||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||