Uncemented Tapered Femoral Components
Kristoff Corten and Robert B. Bourne
Key Points
• Proximal coating of uncemented stems allows for reliable ingrowth and decreased stress shielding of the proximal femur.
• Uncemented stems manufactured with a titanium alloy have been associated with decreased rates of thigh pain.
• Reliable and stable initial three-point fixation with a minimum risk of subsidence can be achieved with a proximal 3D-tapered geometry of the uncemented stem.
• The uncemented, 3D-tapered, titanium alloy stem with proximal coating provides optimal initial fixation and is associated with excellent long-term clinical results and survivorship of 99% at 20 years.
Introduction
During the early 1980s, with total hip arthroplasty (THA) becoming a much more established procedure, concerns surrounding the use of cement fixation started to surface. The longevity of first-generation cementing techniques was being questioned, especially in young, active patients.1–5 The more frequent occurrence of osteolysis, which in retrospect was erroneously attributed to “cement disease,” promoted renewed interest in both improved cementing techniques and cementless fixation with ingrowth or ongrowth of bone to stem. The first generation of cementless femoral stems produced mixed results, with problems related to fixation failure, thigh pain, wear, and osteolysis.6–10 Subsequent generations of uncemented femoral stems have been developed to address these complications and have achieved longevity after 10 years that is at least comparable with that of their cemented counterparts11–20 (Table 69-1).
Table 69-1
Uncemented, Tapered Femoral Components With Minimum 10-Year Follow-up Have Been Reported With Survivorships from 94% to 100%*
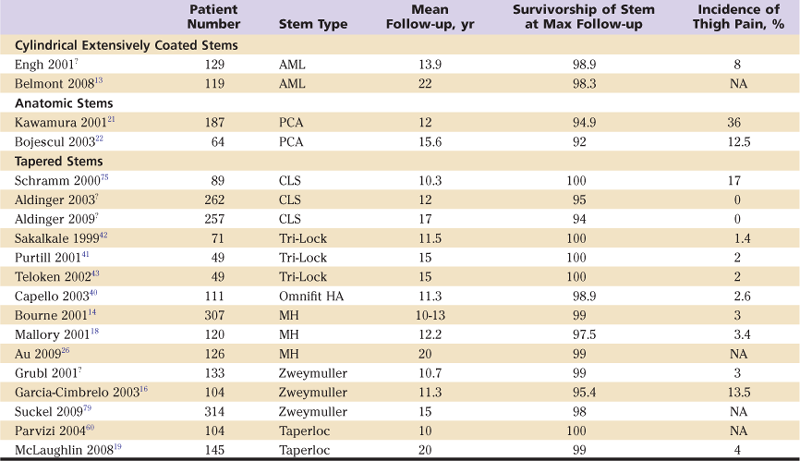
AML, Anatomic medullary locking; PCA, porous-coated anatomic; CLS, cementless locking stem; MH, Mallory-Head; NA, not applicable.
*The prevalence of thigh pain with tapered stems varies between stem designs but also between studies focusing on a particular design. Cylindrical extensively coated stems and anatomic stems have reported survivorships of 98% to 99% and 92% to 95%, respectively; both designs are associated with a high prevalence of thigh pain.
Various cementless THA designs are currently available, and good long-term results are now reported most often. In general, uncemented stems can be grouped into three design categories: anatomic, cylindrical, and tapered. The main differences among these choices include component shape, metallurgy, and head/neck design. Furthermore, the coating surface can vary in extent (proximally vs. fully coated) and in surface properties (e.g., hydroxyapatite, porous, fiber/metal coated). These design features result in different fixation modes, which may influence clinical results.
Anatomic designed femoral stems such as porous coated anatomic (PCA, Howmedica, Rutherford, NJ) are manufactured from a cobalt-chrome (Co-Cr) alloy and achieve fixation by proximal ingrowth. Modular mismatch, endosteal irritation, and lack of ingrowth all were implicated in the high prevalence of symptomatic thigh pain with this implant. At our institution, we prospectively reviewed 311 PCA hip replacements in 279 patients.21 The mean follow-up was 12 years (range, 10 to 14 years) in 168 patients with 187 PCA replacements. The overall survival rate at 14 years with revision for any reason as the endpoint was 90 ± 5.4%, whereas the survival rate of the femoral component was 95 ± 3.6%.21 This was similar to the 4% revision rate for aseptic loosening of the stem at 15 years that was reported by Bojescul.22 Reported prevalence of thigh pain was 36%21 and 13%,22 respectively. Osteolysis and wear of the polyethylene liner were the two most important indications for revision at long term.21,22
Fully porous-coated cylindrical stems such as anatomic medullary locking (AML) stems (DePuy, Warsaw, Ind) achieve primarily distal diaphyseal fixation. This Co-Cr stem has a sintered-bead porous surface. Several reviews have reported on an unselected, consecutive series of 223 patients with an AML stem,13,15,23,24 and results of 119 hips in 113 patients with a minimum follow-up of 20 years (mean, 22 years) have been reported.13 A vast majority of revisions were directed toward the acetabular component (TriSpike, DePuy), and 77 patients (65%) continued to retain all components. Six stems (3%) were radiographically loose, of which four cases had undergone revision. Ninety-six percent of stems achieved bone ingrowth, and none of them subsequently loosened. At the time of the most recent follow-up, 18 hips (16%) were associated with moderate and 9 (8%) with severe functional limitations. Survivorship upon analysis of the stem, with revision for aseptic loosening as the endpoint, was 99 ± 1.5% at 15 years23 and 98.3 ± 1.9% at 20 years.13 Femoral osteolytic lesions were present in 25 of 68 hips (37%) with minimum 20-year radiographic follow-up.13 Although thigh pain was not reported in this series, an earlier publication reported an incidence of 8%.24 Osteolysis and polyethylene wear were the most frequent complications associated with this total hip system.13,15,23,24
Uncemented, tapered femoral components were designed to allow for stable initial three-point fixation and a graduated load transfer to the proximal femur, which reduces excessive proximal stress shielding and decreases the risk for thigh pain (Table 69-2). We reported on the 10- to 13-year performance of a nonconsecutive series of 307 Mallory-Head THAs (Biomet, Warsaw, Ind) in 283 patients.25 Overall 10-year Kaplan-Meier survivorship was 90% for hip replacement and 99% for the stem. Mild stress shielding limited to Gruen zones 1 and 7 was seen in 50% of patients, and activity-related thigh pain was present in only 3%.25 In addition, 20-year results of a randomized controlled trial (RCT) conducted at our institution to compare the results of cementless and cemented fixation of Mallory-Head THA showed that the survival rate of the stem was 99%, with only 1 stem out of 126 revised for periprosthetic fracture. The 20-year survival rate of the cementless system (76%) was significantly higher than that of cemented THA (63%) (P = .018).26
Table 69-2
Overview of the Metallurgy, Coating, and Geometric Features of the Most Common Uncemented, Tapered Stem Designs
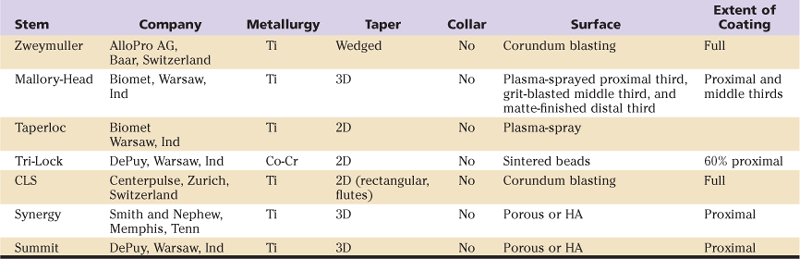
2D, Two-dimensional; 3D, three-dimensional; CLS, cementless locking stem; Co-Cr, cobalt-chrome; HA, hydroxyapatite; Ti, titanium.
In general, not the stem but the acetabular component has been shown to be the weakest link in early-generation cementless THA systems, and long-term survivorship of anatomic, cylindrical, and some tapered designed stems can be considered good to excellent.11–20 However, concerns regarding subsidence with some designs,11,12,27 thigh pain,7,13,15,21,28-30 and stress shielding31,32 have been raised. Uncemented three-dimensional (3D)-tapered femoral components rely on initial three-point fixation followed by proximal porous ingrowth for continued stability. Subsidence does not seem to be a problem with proximally coated tapered-stem designs.25,26,33 When osseointegration has occurred at approximately 12 weeks, a graduated load transfer is induced by the tapered design; this reduces excessive proximal stress shielding, as we have shown in a multicenter, randomized, controlled trial in which proximal coated stems were compared with cylindrical extensively coated stems.34 In addition, the elastic modularity of the titanium alloy approaches the modularity of the femoral bone; this could reduce the prevalence of thigh pain.25 Our experience has been that in terms of fixation, avoidance of thigh pain and stress shielding, with a cementless, proximally coated, tapered femoral component, based on a Titanium alloy (Ti), indeed seems to be a promising option. In this chapter, we will review the design rationale and the surgical technique of tapered cementless stems, as well as currently available outcomes studies.
Design Rationale for Tapered Femoral Components
Cementless tapered femoral components require good initial fixation by means of proper femoral size selection and the design features (i.e., oversized porous coating, antirotation fins) of tapered (usually 3D-taper) stems. There is little doubt that the principle of obtaining good initial femoral fixation is of importance in promoting good long-term fixation between the component and the host bone. Excessive initial micromotion greater than 40 to 75 µm will lead to the formation of fibrous connective tissue at the bone-stem interface.35,36 Tapered femoral components gain initial three-point, self-locking fixation, which also provides rotational stability (Fig. 69-1).
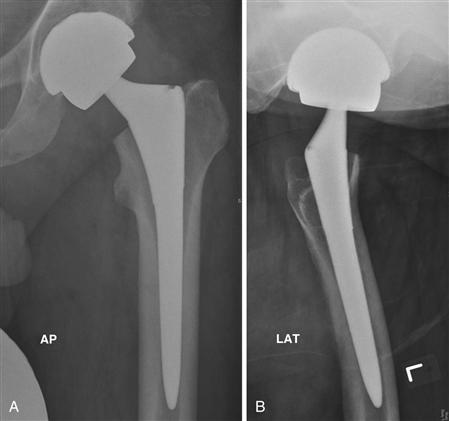
Figure 69-1 Anteroposterior (AP) and lateral (LAT) radiographs of a total hip replacement using a cementless tapered femoral component (Synergy, Smith and Nephew, Memphis, Tenn). On the lateral view, note the three-point fixation of the femoral component with posterior cortical contact proximally, anterior contact at the metaphyseal/isthmic junction, and posterior distal contact.
Popular cementless tapered stems may feature a two-dimensional (2D) coronal or sagittal femoral taper or a 3D-tapered design; the most important difference is that 3D-tapered stems have a transverse taper, in addition to coronal and sagittal tapers. When a tapered component is forced into the cylindrical medullary canal of the femur, hoop stresses are set up. The femoral bone is viscoelastic; this implies that when a tapered stem is introduced into the slightly smaller medullary canal, creep and stress relaxation will occur. Initially, three-point fixation and press-fit will be noted, which implies that when an equilibrium is set up, the axially loaded tapered stem will not advance any farther.37 Over time, viscoelastic relaxation of the bone can occur and the press-fit will lessen. Further advancement of the implant within the bone is prevented by three-point fixation, the high roughness and friction of the porous or hydroxyapatite surface, and the 3-degree tapered design. The initial and intermediate stability of the component within the bone will allow for appositional bone formation on the component surface. This appositional bone in turn will connect to the endosteal bone at approximately 12 weeks.38 In other words, the design of the tapered component allows for stable initial mechanical fixation, which in turn allows for biological fixation over a period of approximately 3 months in the metaphyseal region. As a consequence, the proximal femur is subjected to a more favorable gradual loading profile, which may be responsible for reduced stress shielding and the relatively low prevalence of thigh pain observed with the use of tapered femoral components.7,17,18,39-43 The use of a collar in cementless tapered stems would interfere with initial implant impaction and the secondary small amount of “settling” of the component. Therefore, tapered stems are usually collarless.
Achieving initial rotational stability is of paramount importance for long-term fixation. The Zweymuller stem is a 2D-tapered stem that achieves its rotational stability through its rectangular cross-section and the lock achieved by sharp corners of the stem with cortical bone. Most contemporary cementless tapered stems are round in cross-section, feature a 3-degree three-dimensional longitudinal taper, and obtain additional rotational stability through the use of longitudinal fins. Newer-generation tapered stems such as the Synergy stem (Smith and Nephew, Memphis, Tenn) are 3D tapered at the proximal, porous-coated part of the stem by the addition of a 3-degree taper in the transverse plane. This configuration more closely mimics the proximal geometry of the femur, which is narrower medially (calcar and medial neck) than laterally (greater trochanter) (Fig. 69-1 through 69-3). Tapered stems with circular cross-sections and longitudinal flutes that provide rotational stability also exist. Wagner44 promoted such stems in patients with dysplastic hips, in whom the proximal femur is not morphologically suited to an oval or rectangular stem. The circular shape allows for correction of anteversion and reduces the risk for intraoperative fracture. Highly satisfactory successful outcomes with no thigh pain were reported in a 9-year follow-up study of 635 implants.44
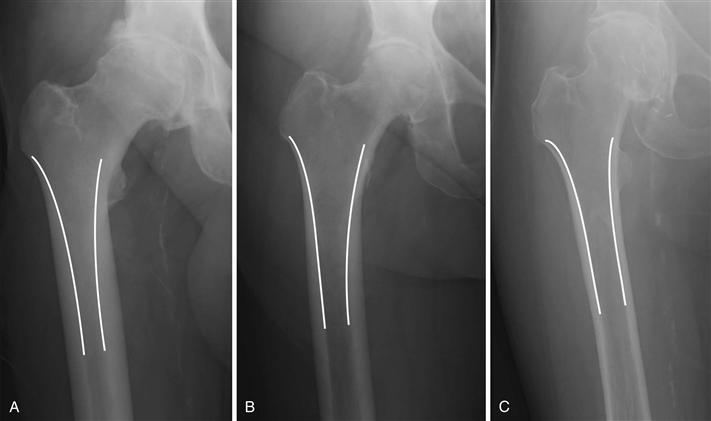
Figure 69-2 Anteroposterior hip radiographs demonstrating the three varying proximal femoral morphologies using the Dorr classification: type A (champagne flute), type B (funnel-shaped), and type C (cylindrical).
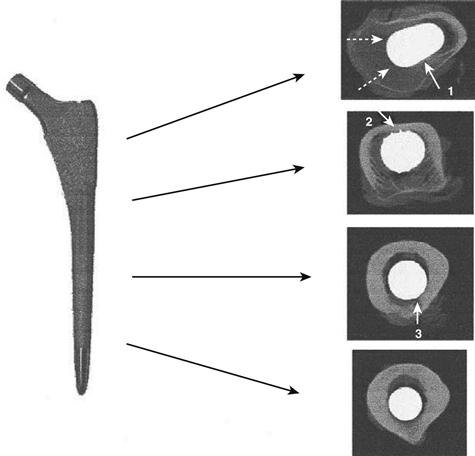
Figure 69-3 Computed tomograms demonstrating where a cementless tapered femoral component (Synergy, Memphis, Tenn) contacts the cortical bone proximally, mid stem, and distally.
A modular mismatch between stem and surrounding bone might lead to an increased incidence of endosteal irritation and thigh pain.7,28 Most tapered cementless stems are made of a titanium (Ti) alloy with aluminum and vanadium (Ti-6Al-4V). This alloy has the greatest fatigue resistance of all Ti alloys and is 50% less stiff than Co-Cr alloys used in earlier cementless designs that were associated with a high incidence of thigh pain.21,22,25 In addition, Ti has been histologically demonstrated to be very biocompatible, with ongrowth (e.g., plasma-sprayed surface) or ingrowth (e.g., porous surface) of the bone to the stem surface.38 This property of Ti alloys enabled Albrektsson to coin the term “osseointegration.”38 More recently, the application of bioactive coatings such as hydroxyapatite (HA), to which Ti specifically lends itself, has been shown to enhance the process of osseointegration.45 However, this has not resulted in improved long-term survivorship in comparison with porous-coated designs without HA coating.20 Furthermore, circumferential proximal coated surfaces seem protective in preventing femoral osteolysis distal to the level of the lesser trochanter.26
The mechanical properties of tapered stems imply that they, theoretically, work best in proximal femoral morphologies with tapered medullary shapes, because the congruency between the 3-degree taper of the implant and the morphology of the proximal femur allows maximal implant-to-bone contact. According to the Dorr classification,46 Dorr type A or B femurs would be ideally suited for tapered stems. However, in our clinical practice, we sometimes use these stems in Dorr type C femurs with good clinical results (see Fig. 69-2).
Surgical Technique
Preoperative Planning
Preoperative planning is a very important step of any THA procedure. A low-centered anteroposterior (AP) radiograph of the pelvis and a true lateral radiograph of the affected hip are needed to assess leg length, the anatomic femoral configuration, the level of the femoral neck cut, offset, and stem size.
Pelvic obliquity, pelvic symmetry, and other leg abnormalities (i.e., malunion, growth arrest, deformity) must be considered when leg length discrepancies are assessed. In most cases, a horizontal line can be drawn through the teardrops (inferior aspects of the pelvic quadrilateral plates). A vertical line drawn through the center of the femoral heads or the tip of the greater or lesser trochanter will detect any leg length that has to be made up. Some surgeons prefer to use a horizontal line to join the ischial tuberosities instead of the inter-teardrop line, but occasionally a fixed flexion contracture of the hip can render these landmarks erroneous (Fig. 69-4).

Figure 69-4 Two options for assessing leg length on an anteroposterior pelvic radiograph using lines joining the teardrops (superior line) or the transischial line (inferior line). When the patient has a fixed flexion contracture of the hip, the line joining the teardrops is preferred.
It is important to preoperatively estimate the anatomic relationship of the tip of the greater trochanter to the medullary canal of the femur. This will allow the surgeon to anticipate any erroneous medial reaming of the canal when the trochanter tip overhangs the femoral canal. This probably will lead to varus positioning of the stem and to relative undersizing of the component. If the tip excessively overhangs the canal, the surgeon should remove the medial part of the tip so that he or she is able to fully access the femoral canal in line with its axis.
Usually, the femoral neck cut is one fingerbreadth (approximately 1 cm) proximal to the lesser trochanter. Preoperative templating will allow the surgeon to adjust the level of the neck cut. A lower neck cut will allow for deeper engagement of the stem in the femoral canal and may be necessary to avoid leg lengthening in a patient with a short—often varus—femoral neck or to avoid excessive femoral stem anteversion in dysplastic femurs with excessive anteversion. A higher femoral neck cut will allow for a relatively higher press-fit of the stem in the proximal femur, which may be necessary to lengthen a short leg or to compensate for a higher valgus neck shaft angle.
Offset restoration is a particularly important aspect of soft tissue balancing that will in turn determine implant stability and long-term survival.47–50 Soft tissue balancing is important to avoid dislocation by tensioning soft tissues, preventing impingement, and improving abductor function and resultant hip joint reaction forces by restoring normal abductor resting length. For offset estimation, the surgeon needs radiographs in which the lower extremities are in neutral rotation. This is sometimes a problem in arthritic hips with external rotation contractures that lead to an underestimation of the true offset. Oblique radiographs sometimes may be beneficial,51 but more important, templating of the contralateral and ipsilateral hip is recommended (Fig. 69-5). Multiple operative factors such as the level of the femoral neck osteotomy, the varus/valgus positioning of the stem, and the position of the acetabular component may have an influence on restoration of normal abductor resting length of the replaced hip. Intraoperatively, the use of a special caliper may help in assessing the amount of leg lengthening that has occurred during surgery and may indicate the degree of restoration of the femoral offset. The jig we use (Smith and Nephew) consists of a pin placed in the iliac crest. It also has an adjustable side arm that is fixed to the pin and allows measurement of both leg length and offset to a point indicated on the greater trochanter. This is done before dislocation of the hip and following trial reduction (see also “Surgical Technique”). This allows the surgeon to anticipate any measured length and offset discrepancies (Fig. 69-6). The geometry of the femoral component also plays an important role in restoring the femoral offset. We compared the original Mallory-Head stem design with a 135-degree neck shaft angle versus the newer Synergy stem, with a 131-degree neck shaft angle and two offset options in terms of restoring femoral head offset.52 Patients with unilateral osteoarthritis were included, and AP radiographs were taken with the leg 15 to 20 degrees internally rotated. In keeping with the criterion that successful restoration of the offset was within 4 mm of the nonoperated side, femoral offset was restored in 99 of 109 patients (91%) in the Synergy group, and in 38 of 93 patients (41%) in the Mallory-Head group.52

Figure 69-5 Templating of ipsilateral and contralateral hips is recommended on an anteroposterior radiograph where magnification has been determined, because the ipsilateral hip often has an external rotation contracture, making it difficult to determine the size of the component and offset required.
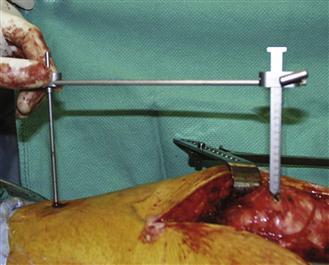
Figure 69-6 The authors’ preferred method of determining leg length and offset restoration, using a pin placed in the iliac crest and a detachable leg length/offset guide. Leg length and offset are determined before the hip is dislocated, then are reassessed with the trial components and final components in place to verify that the required corrections have been made.
Finally, the stem size will be determined by the diameter of the femoral canal, but most important, it also will be determined by the anatomic and biomechanical requirements of the proximal femur such as the femoral offset.
Surgical Technique
The surgical procedure using a tapered uncemented femoral component is simple and straightforward. Cementless tapered stems can be inserted using any of the traditional surgical approaches (anterolateral, posterior, transtrochanteric, and minimally invasive). In our institution, we prefer to use a direct lateral Hardinge or posterolateral surgical approach. Before dislocating the femoral head, we fix a pin to the iliac crest and use the cautery and a marking pen to identify a landmark on the greater trochanter. The leg length/offset jig is then fixed to the pin and set at the level of the trochanter landmark, with the leg in a position that can be reproduced later on with the trial components in place. Following the femoral neck osteotomy, the acetabulum is reconstructed using the surgical technique pertinent to use of the intended acetabular component. We usually first insert a trial liner. The leg is externally rotated and the lower limb is placed in a leg bag placed on the side opposite to the surgeon. The femoral canal is opened with the use of a box osteotome. It is important to stay as lateral and posterior as possible. The use of a blunt Hohman retractor behind the greater trochanter and a Hohman retractor behind the posterior cortex to elevate the proximal femur into the wound is recommended. Sequential tapered reamers are used to enlarge the femoral canal. Care is taken to prevent damage to the gluteus medius muscle. During reaming it is important to stay as lateral as possible. Failure to do so may result in ultimate varus placement of the component. If necessary, and as assessed on preoperative templating, it might be helpful to remove some medial bone of the tip of the greater trochanter with a broach or a rongeur. Reaming is stopped when the templated size reamer reaches the osteotomy level. If reaming is held up at a smaller size than templated, varus malpositioning is the usual cause. Next, the broaches are used to further prepare the femoral canal. The first broach used should be at least two sizes smaller than the templated size. If progression of the broach is slow, the surgeon should consider two steps: (1) rasping of the lateral aspect of the femoral canal to correct for any varus malpositioning, and (2) careful partial extraction and reintroduction of the broach to clear its teeth to overcome resistance to further introduction of the broach. Full seating of the broach is established when the level of the femoral neck osteotomy is reached. The broach handle is toggled using the antirotation side bar on the handle to observe the potential for rotatory movement between the broach and the bone. If any rotation of the stem still occurs, upsizing of the stem is probably required. With the broach seated, a calcar reamer may be used to remove some prominent bone, which bears a potential for impingement. At this stage, a trial reduction can be done with the final broach in place to assess for stability of the hip (Fig. 69-7). Changes to stem offset, neck length, femoral neck cut, and acetabular liner can still be made. With the trial components in place, the leg length/offset jig can be reapplied to the pin. Assessment of the position of the previously set jig relative to the previously identified trochanter landmark will allow evaluation of whether any adjustments to the stem or the liner (with or without offset) would improve hip biomechanics. The hip is taken through a full range of movement, and soft tissue tension is assessed. External rotational stability of the hip should be tested in extension, and stability in maximal internal rotation in 90 degrees of flexion should be evaluated. Also, any potential for impingement is investigated and offending osteophytes are removed. If this is satisfactory, the definitive stem and liner can be inserted.
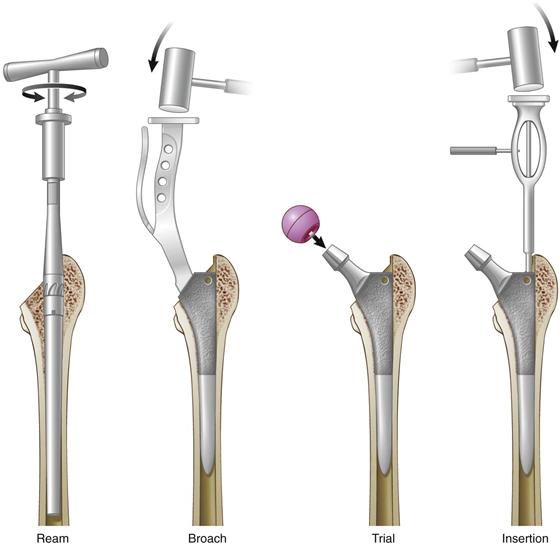
Figure 69-7 A pictorial representation demonstrating the four easy steps of inserting a cementless tapered femoral component (i.e., ream, broach, trial, and insert).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








