Uncemented Short Metaphyseal Femoral Components
S. David Stulberg and Ronak M. Patel
Key Points
Introduction
Total hip arthroplasty (THA) is a highly successful, safe, and cost-effective intervention for the treatment of patients with moderate and severe degenerative arthritis. Porous-coated, uncemented femoral stems were introduced in the 1980s for use in total hip arthroplasty. Uncemented stems, which achieve their fixation by porous diaphyseal fixation or by porous metaphyseal fixation–nonporous diaphyseal contact, produce dependable long-term fixation and pain-free function in patients of all ages and bone quality and in those with a wide range of clinical function.1–59 Uncemented, porous femoral implants are now used routinely in virtually all patients undergoing primary THA in North America. Despite the documented success of these implants, uncemented stems are currently being used in patients whose size, age, level of physical activity, and bone quality present particular challenges for uncemented fixation technologies. These challenges include (1) the need for very long-term fixation; (2) the preservation of proximal femoral bone stock; (3) the potential need for effective femoral component revision; (4) the desire to reproduce a wide range of proximal femoral extra-articular anatomic variations with the provision of multiple offset options; (6) the elimination of thigh pain in extremely active patients of all ages and bone quality; and (7) the ability to insert implants safely, securely, and reproducibly via specific surgical approaches (e.g., direct anterior) that are currently being evaluated and promoted. The success that has been achieved with uncemented femoral stems of a wide range of designs is now encouraging investigators to consider uncemented femoral implant concepts that address these challenges without compromising the high level of success attainable with current uncemented femoral components.
In particular, clinicians have expressed an interest in short uncemented stem designs that rely for their stability on femoral metaphyseal fixation. The purposes of this chapter are to (1) review the principles underlying these types of femoral components, (2) describe the various design characteristics of these stems, (3) summarize initial clinical results with these stems, and (4) suggest the direction that these design concepts may take in the near future.
Functions of the Diaphyseal and Metaphyseal Portions of Uncemented Femoral Stems
To understand the design rationale that is currently being applied to short, metaphyseal engaging femoral stems, it is important to consider the function of each portion of a femoral implant. The section of the femoral component that engages the diaphysis contributes to the initial stability of the device. This portion of the component may be cylindrical or tapered (Fig. 70-1a through c). Tapered stems may be two-dimensional (a coronal taper and a nontapered rectangular lateral border) or three-dimensional (tapered in both coronal and sagittal planes). The diaphyseal engaging stem may be made of cobalt-chrome alloy or titanium alloy. It may be fully coated with a three-dimensional porous surface, a thin layer of hydroxyapatite, a grit-blasted finish of varying degrees of roughness, or a combination of some or all of these surfaces. The diaphyseal portion of the stem may be polished. The femoral stem may have flutes to resist rotation and/or slots to reduce stiffness. The intended function of the diaphyseal portion of a femoral stem is reflected in its shape, metallurgy, and surface treatment.
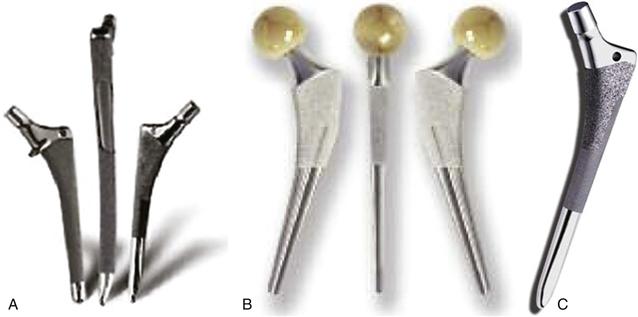
Figure 70-1 A through C, The section of the femoral component that engages the diaphysis contributes to the initial stability of the device. This portion of the component may be cylindrical or tapered and may be porous coated, hydroxyapatite coated, grit-blasted, smooth, or a combination. A, Cylindrical with various coating lengths. B, Narrow tapered stem. C, Anatomic tapered stem.
Cylindrical, cobalt-chromium, extensively porous coated stems (e.g., anatomic medullary locking [AML]) are designed to provide rigid initial and long-term fixation in the diaphysis. Initial axial fixation is achieved by tightly engaging a significant segment of the endosteal diaphyseal cortex. Although this engagement with the diaphysis may provide initial rotational stability, the porous coating also provides some resistance to rotational stresses. Long-term fixation is achieved by bone ingrowth into the porous coating. The long-term clinical and radiographic results of cylindrical, extensively coated stems have been extensively documented.21,22,60-72 The long-term stability of stems of this design is excellent in patients of all ages and bone quality. Consistent concerns associated with these stems have included stress shielding and thigh pain11,66,67,72-83 (Fig. 70-2). Cylindrical stems without porous coating may be made of cobalt-chromium or titanium alloys. The surfaces may be grit-blasted to varying degrees or polished. Cylindrical stems with a titanium alloy core and a flexible polymer coating are also available.27,46,84 These stems are designed to provide a degree of initial axial and rotational fixation by coming in contact with the diaphysis, but they avoid the stress shielding and thigh pain that might be associated with large, long, metal cylindrical stems.

Figure 70-2 Consistent concern associated with extensively porous-coated, cylindrical stems has been stress shielding. Poor bone remodeling in a well-fixed, extensively porous-coated femoral stem.
Cylindrical femoral components with absence of a diaphyseal porous coating rely on metaphyseal bone contact to enhance their initial axial and, especially, rotational stability. Moreover, these stems seek long-term fixation through bone ingrowth or ongrowth at the metaphysis. These stems achieve metaphyseal stability by attempting to optimize resistance to rotation with rectangular shapes, lateral antirotation ridges, or wedge shapes. Some implants with uncoated cylindrical stems seek to achieve rotational stability and optimized proximal bone restoration by maximizing the fit and fill of the metaphysis (e.g., the PCA implant). All current metaphyseal engaging implants with nonporous coated diaphyseal stems seek to increase rotational stability and positive bone remodeling with metaphyseal circumferential porous coatings or ongrowth surfaces. Numerous reports of follow-up longer than 10 years indicate that femoral components with cylindrical stems without ingrowth or ongrowth coating are associated with durable fixation and very satisfactory and reliable clinical results.* The goals of stems of this design are to reduce the incidence of thigh pain and stress shielding associated with extensively porous-coated, cylindrical stems while retaining, through osseointegration in the metaphysis, durable fixation. In general, stems of this design appear to be associated with a lower incidence of thigh pain and less proximal stress shielding than extensively coated, cobalt-chromium, cylindrical stems.†
Tapered uncemented femoral components seek to achieve fixation in two phases.100 Initial rigid fixation is achieved by three-point self-locking fixation (Fig. 70-3). When the tapered stem is securely inserted into the cylindrical femur, hoop stresses are generated. When stress relaxation of the femur has occurred, equilibrium is set up between bone and stem, and the axially loaded tapered component will not advance. In principle, this mechanism of initial axial fixation works best in proximal femoral morphologies with tapered medullary shapes. Therefore stems of this design are best applied to Dorr type A (champagne fluted) and type B (funnel shaped) and are less well suited to type C (cylindrical shape) femurs.90,100 The proximal component taper seeks to maximize implant-bone contact with the intramedullary proximal femoral shaft taper and to provide a gradual loading profile to the proximal femur.
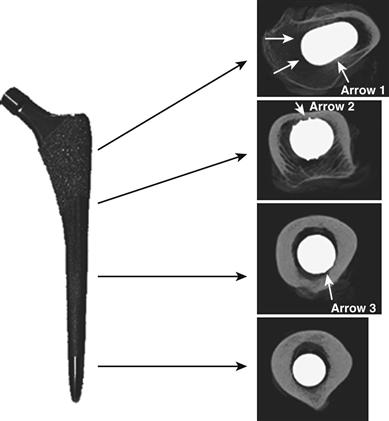
Figure 70-3 Computed tomography scan images from four regions along the length of a tapered cementless femoral implant (Synergy). Proximally, primary cancellous contact occurs. In the proximal quarter, posterior cortical contact is noted (arrow 1). In the second quarter, anterior cortical contact is evident (arrow 2). In the third quarter, cortical contact is seen posteriorly (arrow 3). (Courtesy Busch CA, Bourne RB: The tapered femoral stem. In Callahan JJ, Rosenberg AG, Rubash HE, editors: The adult hip, ed 2, Philadelphia, 2007, Lippincott Williams & Wilkins, pp 1025–1035.)
Establishment of rotational stability of tapered stems is critical for achieving initial rigid fixation of tapered stems. Some tapered stem designs (e.g., Zweymuller [Zimmer Inc., Swindon, United Kingdom] and cementless locking stem [CLS]) are rectangular. Some (e.g., Taperloc, Biomet, Warsaw, Ind) have antirotation lateral ridges. Other stems (e.g., the Synergy stem, Smith & Nephew, Fort Washington, Pa) have wedge-shaped proximal geometries. Still others (e.g., the ABG stem, Stryker Corporation, Berkshire, United Kingdom) have anatomically shaped metaphyseal designs that seek to achieve rotational stability by maximizing fit and fill in the proximal femur (Fig. 70-4).

Figure 70-4 Tapered stem designs may achieve proximal stability with (A) rectangular shapes (Zweymuller); (B) antirotation lateral wedges (Taperloc); (C) wedge-shaped proximal geometries (Synergy); and (D) anatomic-fit/fill-metaphyseal designs (ABG). A, Tapered stem with antirotational rectangular shape (Zweymuller). B, Tapered stem with antirotation ridges (Taperloc). C, Tapered stem with wedge metaphyseal design (Synergy). D, Tapered stem with anatomic metaphyseal design (ABG).
The second stage of fixation sought by tapered stems occurs in the metaphysis and depends on the presence of a circumferential ingrowth or ongrowth surface.100 It is believed that the more extensive the area of contact between implant and metaphyseal bone contact, the more secure will be the secondary fixation, and the more positive will be the proximal bone restoration and remodeling. The goals of tapered stems are to achieve rigid durable fixation, to eliminate thigh pain, and to minimize stress shielding. A substantial number of studies have established the clinical and radiographic reliability and durability of tapered stems of many designs.* In general, the use of femoral components with tapered diaphyseal stems is associated with less thigh pain than implants with cylindrical stems.9,74,77,83,100
In summary, the diaphyseal portions of femoral stems, both cylindrical and tapered, are designed to provide primary axial stability to the component and varying degrees of rotational stability. These portions of the implant are particularly critical for achievement of rigid initial fixation. The metaphyseal portion of femoral implants provides initial rotational stability. Provision of this stability may be particularly important in stems of tapered designs or polished cylindrical designs, in which localized bone contact and absence of porous coating reduce that resistance to rotation provided by the diaphyseal portion of these implants.
Design Rationale and Requirements for Uncemented, Short, Metaphyseal Engaging Stems
Short, uncemented, metaphyseal engaging stems seek to address the following issues: (1) the need for very long-term fixation in young patients; (2) the preservation of proximal femoral bone stock, particularly in young patients and patients with poor proximal femoral bone quality; (3) the potential need for effective, bone-preserving femoral component revision; (4) the elimination of thigh pain in extremely active patients of all ages and bone quality; and (5) the ability to insert implants safely, securely, and reproducibly using specific surgical approaches, in particular, the direct anterior approach.112 Developers of these stems believe that these goals can be best attained by femoral components that achieve secure enough initial fixation in the metaphysis that the axial and rotational stability provided by the diaphyseal portion of the femoral implant is not important or perhaps even necessary. Long-term fixation of these short components is achieved, it is hoped, in the same manner as that achieved by tapered implants (i.e., metaphyseal ingrowth or ongrowth).
A wide variety of short stem designs have been introduced over the past few years (Fig. 70-5). Although some of these stems incorporate unique design characteristics, many are simply shortened versions of currently available cementless stems. A classification of these short, metaphyseal engaging stems has not yet been developed; however, currently available implants fall into one of two categories: (1) standard neck resection and (2) femoral neck sparing. The former implants are frequently shortened versions of currently available uncemented stems of standard length; the latter often incorporate new, unique design features. Although no accepted definition of “short stem” has been identified, most implants seeking this designation are 110 mm or less from the level of the top of the prosthesis neck to the tip of the stem.
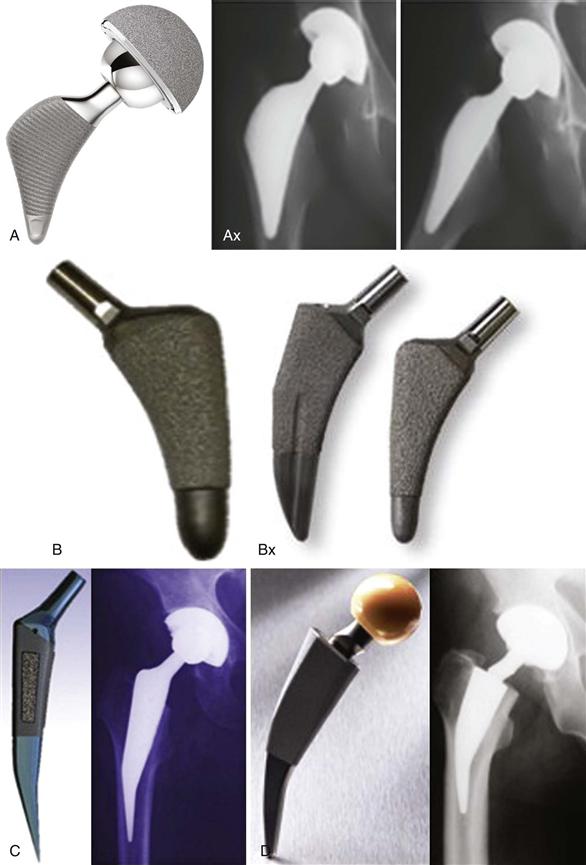

Figure 70-5 A wide variety of short stem designs have been introduced in the past few years. A, Proxima stem. B, Microplasty Balance and Taperloc stems. C, Mayo stem. D, Metha stem. E, Eska stem.
Experience with stems that are shortened versions of cementless stems of standard length and that are inserted using a standard level of neck resection has been gradually accumulating over the past 4 years.106,112-115 Stems included in this category may have shortened tapered or cylindrical diaphyseal-reaching stems and metaphyseal shapes that range from currently available two- or three-dimensional taper shapes that achieve 2-point wedge fixation in the metaphysis113 to anatomic shapes that seek to fit and fill the metaphysis.112 Investigators of these shortened versions of cementless implants of standard length (e.g., the Taperloc Microplasty stem, Biomet; the Citation Short, Stryker) anticipate that the proximal, metaphyseal fixation provided by stems of standard length will be adequate to achieve initial and long-term stability of the shorter versions.
Although extensive laboratory work examining the characteristics of femoral stems, including stem length, has been done for cemented femoral implants, little research has focused on the impact of stem length on the performance of uncemented femoral components.71,116-118 Therefore, virtually no laboratory evidence underlies the current clinical use of short stems. Early adopters of these types of devices hope that the extremely reliable midterm clinical and radiographic results with stems of standard length will be replicated by the shortened implants. In this early evaluation phase of these short stems, investigators have tended to restrict the use of these devices to patients with good bone quality, those who are younger, and patients who are not excessively large. Moreover, investigators tend to follow a somewhat less aggressive return to full activity and weight bearing than normal.119,120 These stems are being inserted using all of the surgical approaches and current surgical techniques employed for their standard length counterparts. Initial clinical and radiographic results with these shortened stems of standard metaphyseal design have been encouraging. No reports have described an increased incidence of early stem subsidence or loosening, of unsatisfactory or atypical clinical and functional results, or of inadequate bone ingrowth or remodeling. However, reports on the use of these stems at this time are sparse and describe short-term results from centers responsible for the development of these stems or from centers very familiar with the use of devices of standard length. Nevertheless, it is noteworthy that, unlike the experience with surface replacement arthroplasties, these favorable initial results appear to have been achieved with little if any learning curve. If results in the hands of these initial users are sustained and replicated by the general orthopedic surgical community, it is conceivable that surgeons familiar with the use of devices of standard length can relatively easily adopt the shorter versions. What must be established, however, is whether implants of varying metaphyseal design will produce equally satisfactory clinical and radiographic results when their stems are shortened.
The concept of high femoral neck resection in association with the use of cementless stems has been discussed and evaluated since the earliest days of uncemented total hip arthroplasty.121–128 The rationale for this concept has been based on the belief that additional initial implant stability and optimal proximal femoral neck preservation can be achieved with this design. Proponents of this concept have suggested that important bone and soft “tissue sparing” occurs with the use of these implants. This tissue preservation is believed to enhance implant fixation, reduce symptoms associated with surgical trauma, improve abductor muscle function, and provide additional bone stock if future procedures are necessary. Both conventional-length (Freeman, Whiteside, Pipino) and short (Mayo) stems have been combined with the concept of high femoral neck resection.
Although results reported by the developers of uncemented femoral components inserted with high femoral neck resection have been encouraging,116,123,125,129-132 widespread use of these devices has not yet occurred. A number of reasons have been proposed for the slow adoption of this concept. The surgical technique for inserting stems of this design is more difficult than more standard neck resection approaches. The long retained femoral neck can make exposure of the acetabulum difficult. Accurate, reproducible alignment of the femoral stem within the diaphysis may be difficult to accomplish. Restoration of accurate leg length and avoidance of lengthening of the extremity may be difficult to achieve. Moreover, the high neck resection limits exposure of the metaphysis and may reduce the extent and reliability with which metaphyseal fit and contact can be achieved. Concerns have been raised that the combination of high neck resection and short stems may be associated with an increased incidence of proximal femoral fractures.117 Finally, surgeons and investigators have suggested that the use of implants inserted using a high femoral neck resection may result in increased bone-bone impingement and a consequent reduction in range of motion.
Nevertheless, encouraging results with the original short-stemmed implants inserted with a high neck resection have led to the development of a substantial number of new designs that are currently in various phases of clinical evaluation. Development of these devices is being spurred by a renewed interest in the use of the direct anterior approach for THA, the desire for surgical and implant approaches that minimize soft tissue and bone trauma, and a concern about proximal bone preservation and positive bone remodeling. Increasing concerns regarding the use of metal-on-metal surface replacement arthroplasties are also stimulating interest in the development of reliable, safe, tissue-preserving short-stemmed femoral implants as a possible alternative to surface replacements.
Evolution of and Experience with Metaphyseal-Engaging Short Stems
For many years, our center has had an interest in the development and application of metaphyseal-engaging short-stemmed femoral components. This interest focused on four issues related to cementless femoral fixation: (1) optimizing load transfer to the proximal femur and preserving femoral bone stock80,133; (2) eliminating the potential for proximal metaphyseal and distal diaphyseal mismatch (Fig. 70-6a and b); (3) facilitating the use of potentially less invasive surgical exposures, especially the direct anterior approach; and (4) making possible a bone-conserving revision of the well-fixed, ingrown femoral component, if this was ultimately required. We believed that these issues could and should be addressed without compromising the results that are achievable with current cementless femoral components of standard length. Specifically, the goal was to identify design characteristics of metaphyseal-engaging short-stemmed femoral components that (1) could be inserted reproducibly with a surgical technique that was associated with a minimal learning curve; (2) provided secure enough initial fixation to allow immediate, full weight bearing; (3) allowed a high level of function without thigh pain; (4) could be used in patients of all ages with all bone types; and (5) provided durable fixation with positive proximal femoral bone remodeling.

Figure 70-6 Two types of proximal-distal mismatch treated with metaphyseal-engaging, short-stem devices. A, Proximal femoral fracture. B, Wide metaphysis, narrow diaphysis in a young, robust male patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








