Ultrasound Anatomy of the Ankle and Foot
Thomas Grant
Musculoskeletal ultrasound (US) is a rapidly evolving technique that is gaining popularity for the evaluation and treatment of joint and soft tissue diseases. A clear understanding of normal US anatomy is required to prevent misdiagnosis and ensure optimal patient care. The advantages of sonography include its unsurpassed depiction of normal and pathologic anatomy, accessibility, and multiplanar capability. Selective use of high frequency transducers and optimization of sonographic parameters improves visualization of normal and pathologic tissue. Comparison with the contralateral anatomic structures and dynamic scanning are invaluable in aiding learning and interpretation of normal and pathologic features.
Advances in technology with higher frequency transducers, power and color Doppler, and extended field-of-view (FOV) functions have facilitated the progressive development of sonography (Figs. 14.1 and 14.2).1, 2 US offers a cost-effective alternative for imaging musculoskeletal disorders in many situations.
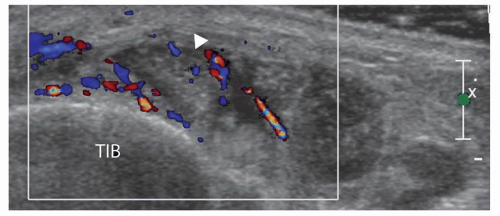
The major soft tissues of the ankle and foot are predominantly superficial and can be assessed with a high-frequency linear transducer. The in-plane spatial resolution and minimal slice thickness using these probes are superior to those achieved with clinical magnetic resonance (MR) protocols. The small footprint probes are particularly useful to maintain constant uniform contact between the probe and skin. Active or passive movement can be used for dynamic evaluation of all tendons for tears, abnormal movement due to subluxation, and adhesive tenosynovitis (Fig. 14.3).3 Interrogation with color or power Doppler imaging is performed if tendon abnormality is seen. Power and color Doppler vascularity within a tendon or the soft tissues usually indicates tendinopathy or synovitis.1
TENDONS
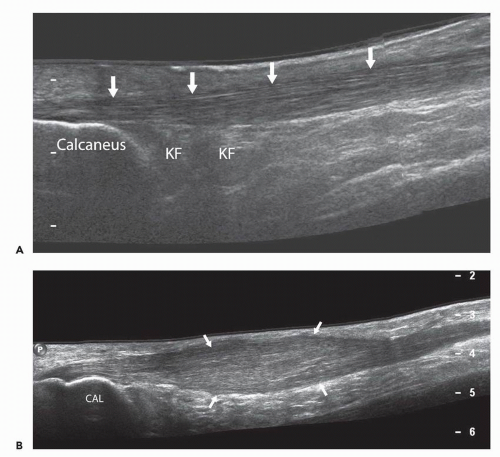
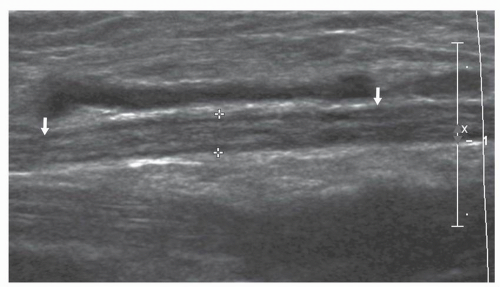
Tendons are better visualized with US than with MR imaging (MRI). Tendons consist of bundles of linear arranged fibrils of type I collagen with a supporting matrix. The fibrils are oriented in a direction specific to the forces applied from the interaction between a tendon and its muscle and skeletal attachment.4, 5 During movement, tendons shorten and lengthen as springs do, transmitting and absorbing forces. When the US beam is perpendicular to the tendon, the energy of the beam is reflected back to the transducer resulting in a fibrillar pattern of alternating hyperechoic and hypoechoic lines (Fig. 14.4). The fibrillar pattern is unique to tendons. If the beam loses this perpendicular orientation, the beam is reflected away from the transducer and the tendon will appear hypoechoic within a hyperechoic paratenon. This phenomenon is known as anisotropy and can be avoided by keeping the beam perpendicular to the tendon.
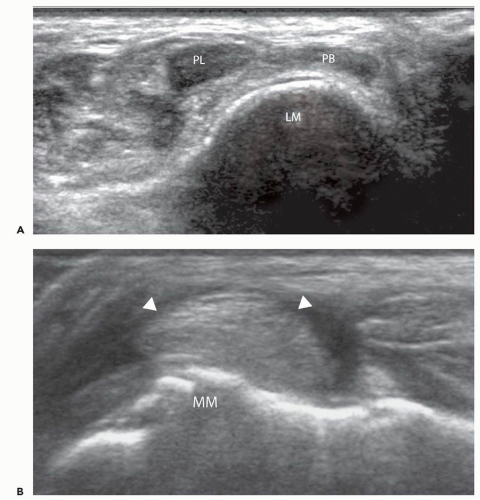
LIGAMENTS
Ligaments also contain longitudinally arranged parallel fibers of type I collagen.6 However, their architecture is not as fibrillar (Fig. 14.5). Although anisotropy is observed, it is not a prominent imaging feature, but it can be used to find ligaments and distinguish them from surrounding connective tissue. Like tendons, ligaments must be imaged longitudinally and transversely.
NERVES
Peripheral nerves can also be accurately identified using US imaging. Nerves are composed of multiple axons that are bundled together in neuronal fascicles. The fascicles are held together by loose connective tissue: the epineurium.7, 8 Normal peripheral nerves typically appear as echogenic fascicular structures and tend to be slightly less echogenic than tendons or ligaments (Fig. 14.6). This appearance is somewhat variable depending on the location and orientation of the nerve but can usually be identified by the nerve distribution.
CAPSULE AND FASCIA
Capsular tissue and fascia appear hyperechoic.
CORTICAL BONE
Cortical bone is hyperechoic, reflecting the insonating beam and producing a black acoustic shadow; hence, precluding visualization of the osseous medulla.
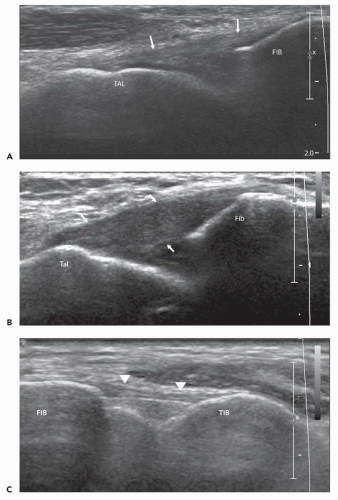
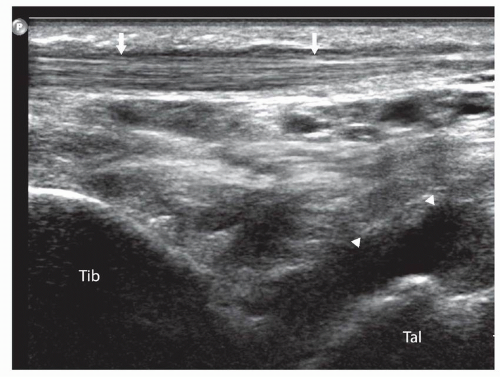 Figure 14.4 Normal tibialis anterior tendon (arrows) superficial to the talus (Tal) and tibia (Tib). Note the articular cartilage of the talus (arrowheads). |
ARTICULAR CARTILAGE
Hyaline articular cartilage is anechoic and homogenous and can only be visualized in areas free of acoustic shadowing from neighboring bony structures—among them, the dorsal articular surfaces of most of the forefoot and midfoot joints.
MUSCLE
Muscle, like tendons and ligaments, has an organized structure. The epimysium is identified as an echogenic envelope surrounding the muscle belly, whereas the perimysium, enveloping muscular fascicles, is seen as short echogenic lines or dots on a hypoechoic background (Fig. 14.7). Intramuscular tendon extensions and bright intermuscular septae and aponeuroses are also easily identified on sonography.4
FLUID AND SYNOVIUM
Bland uncomplicated fluid and synovium appear uniformly anechoic. Posterior acoustic enhancement, the absence of vascularity on Doppler imaging, and the swirling movement of debris on intermittent pressure with the probe may differentiate simple fluid from synovium.
NORMAL ULTRASOUND ANATOMY OF THE ANKLE
The ankle is the most frequently injured major joint in the body. It is also involved by degenerative and rheumatology-related diseases. US has become an increasingly important imaging modality in the assessment and diagnosis of tendons, muscles, ligaments, nerves, and the soft tissues.9, 10, 11 However, radiographs of the ankle should be obtained to evaluate for bone lesions that can be overlooked or not visualized using US.
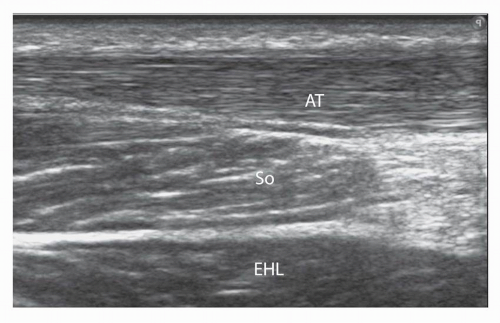 Figure 14.7 Normal soleus (So) muscle and extensor hallucis longus (EHL) muscle anterior to the Achilles tendon (AT). |
Anterior Ankle
The tibialis anterior (TA) tendon, extensor hallucis longus (EHL), extensor digitorum longus (EDL), the anterior tibial artery, the deep peroneal nerve, and a portion of the tibial talar joint can be assessed with US.12
The TA is the widest of the tendons and attaches to the anterior and inferior medial cuneiform and first metatarsal. The EHL and EDL lie adjacent to each other in the ankle and fuse with the extensor hood (Fig. 14.8). The anterior tibial artery lies lateral to the EHL tendon. It is readily assessed by visualizing its pulsatility or with Doppler imaging (Fig. 14.9). The deep peroneal nerve runs adjacent to the artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree