Cross-Sectional and Topographic Anatomy
Shahan K. Sarrafian
Armen S. Kelikian
I. CROSS-SECTIONAL ANATOMY
The cross-sectional anatomy provides the foundation for the topographical, surgical anatomy.
The compartmental anatomy of the tibiotalocalcaneal tunnel is best understood when considered in continuity with the posterior compartment of the leg.
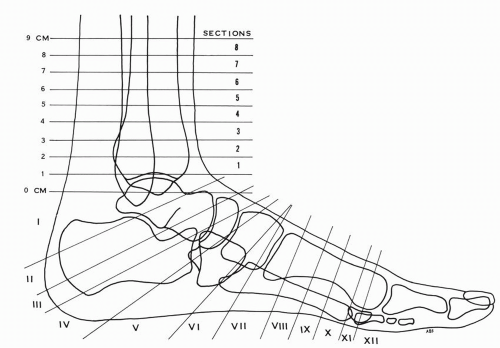
A cross-sectional study was conducted in the transverse, oblique, and coronal planes in two fresh frozen lower legs-feet. In the major first specimen, the sections were made as indicated in Figure 9.1. This provided transverse sections of the distal leg-ankle 1 cm apart, followed by oblique section blocks of the hindfoot, tarsus, and coronal sections up to the base of the proximal phalanx of the big toe. The second specimen provided coronal sections of the hindfoot and tarsus. Previous crosssectional materials were incorporated for further clarification or demonstration of the anatomy.
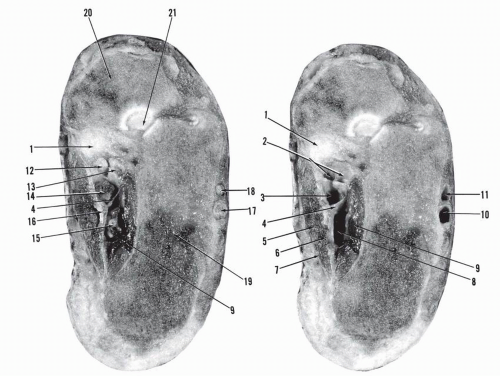
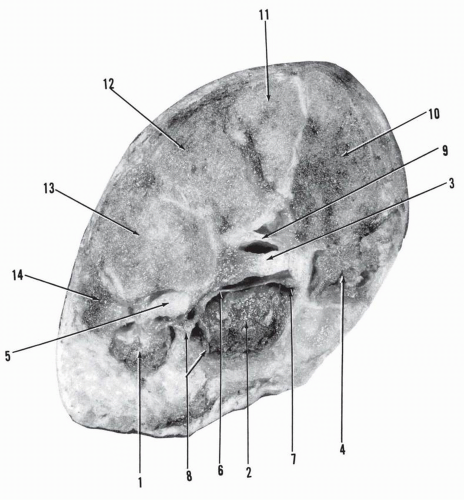
TRANSVERSE CROSS-SECTIONS OF THE DISTAL LEG AND ANKLE
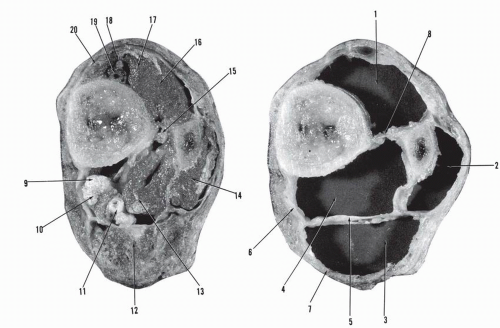
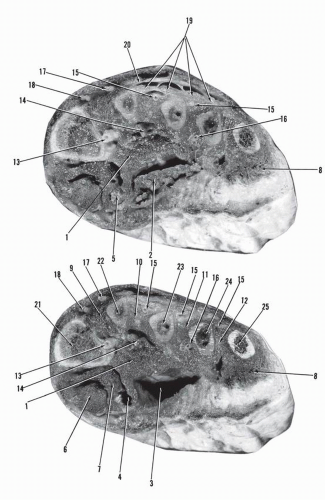
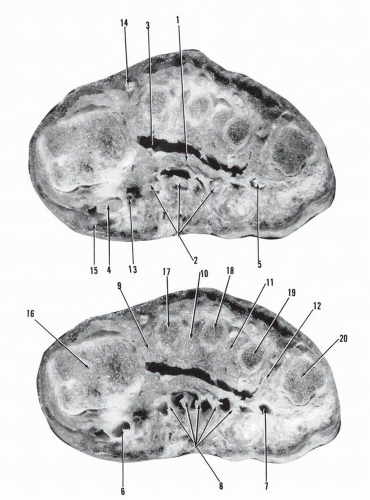
As shown in Figure 9.2, Section 8 is 8 cm proximal to the level of the medial malleolus (distal surface of section). The tibia and fibula are united by the interosseous membrane and the leg is enveloped by the superficial aponeurosis cruris. Four compartments are delineated: anterior, lateral, posterior superficial, and posterior deep. The posterior compartment has been divided into a superficial and deep compartment by the deep aponeurosis cruris. The latter originates from the posteromedial border of the tibia, adheres initially to the superficial aponeurosis cruris, and then diverges transversely to insert on the posterior wall of the lateral compartment.
The anterior compartment contains the extensor digitorum muscle, the extensor hallucis muscle, the tibialis anterior, which is becoming tendinous, and the anterior tibial neurovascular bundle. The vessels are against the bone, with the nerve anterior. The neurovascular bundle is located between the tibialis anterior and the extensor hallucis longus muscle.
The lateral compartment lodges the peroneus longus and brevis muscles. The superficial posterior compartment contains the gastrocnemius-soleus muscle. Located in the deep posterior compartment are the musculotendinous flexor hallucis longus and the tibialis posterior tendon anterior to the musculotendinous flexor digitorum longus. The posterior tibial neurovascular bundle is also located in this deep compartment against the deep crural aponeurosis. The peroneal artery is just posterior to the interosseous membrane.
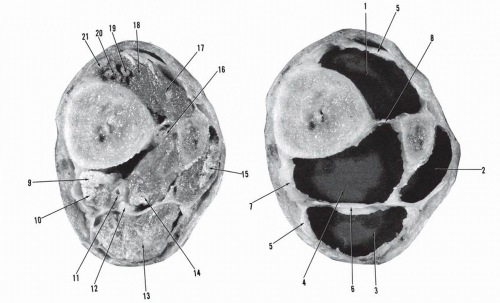
Section 7 is 7 cm proximal to the level of the medial malleolus (distal surface of section; Fig. 9.3). The partition of the compartments and the contents are similar to those in Section 8 except for the slight decrease in size of the posterior superficial compartment.
Section 6 is 6 cm proximal to the level of the medial malleolus (distal surface of section; Fig. 9.4). The partition of the compartments is unchanged. The lateral compartment is shifting posteriorly. The superficial posterior compartment is decreasing in size.
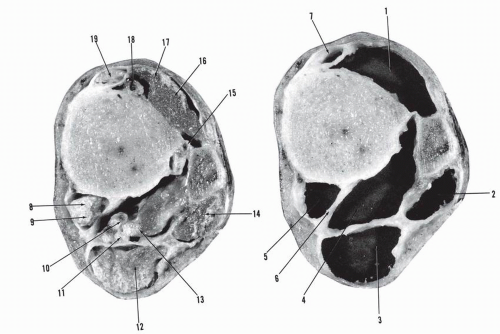
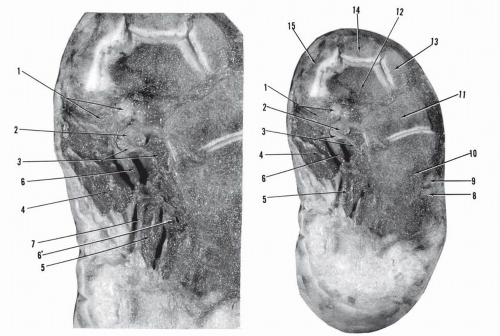
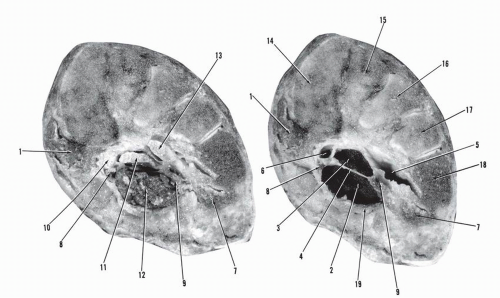
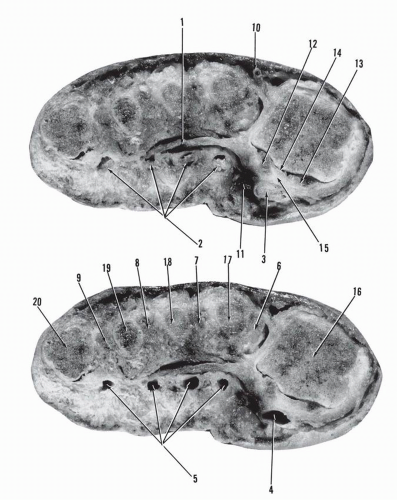
Section 5 is 5 cm proximal to the level of the medial malleolus (distal surface of section; Fig. 9.5).
A major change occurs: a fifth compartment appears. A new aponeurotic structure appears in the deep posterior compartment. It originates at the posteromedial border of the tibia, courses posteriorly, remaining adherent to the deep aponeurosis cruris, curves back anteriorly, and attaches to the posterior aspect of the tibia. It delineates a deep posteromedial fifth compartment, which lodges the tendons of the tibialis posterior and the flexor digitorum longus. The remaining larger segment, deep posterolateral, contains the posterior tibial neurovascular bundle and the musculotendinous flexor hallucis longus. The lateral compartment has shifted into a posterior position relative to the fibula. In the anterior compartment, a tunnel has formed for the tibialis anterior tendon.
Section 4 is 4 cm proximal to the level of the medial malleolus (distal surface of section; Fig. 9.6). The interosseous membrane has disappeared. The tibial metaphysis is united to the distal fibula through the syndesmosis. Five compartments are present, as in the previous section. The tibialis posterior tendon is medial to the flexor digitorum longus tendon: the crossing of the two tendons has occurred and this level is considered the beginning of the tibiotalocalcaneal tunnel. A triangular aponeurotic space is present, superficial to the deep posterior compartment. It lodges a medial calcaneal neurovascular bundle. The anterior peroneal artery is now seen anterior to the tibiofibular syndesmosis.
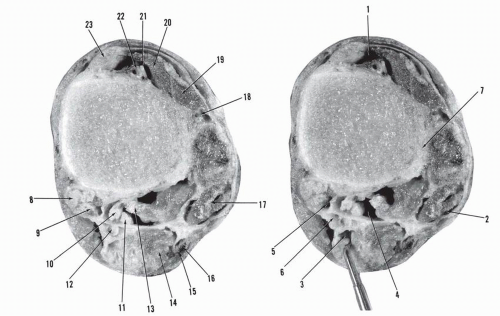
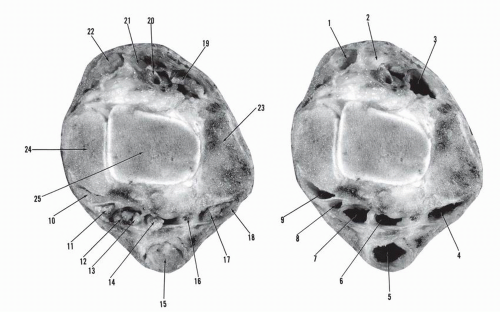
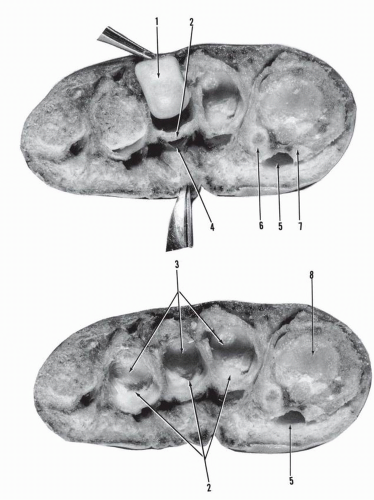
Section 3 is 3 cm proximal to the level of the medial malleolus (distal surface of section; Figs. 9.7 and 9.8).
The tibial distal metaphysis is quadrilateral with concaveconvex fit at the tibiofibular syndesmosis. The deep posterior compartment is now reduced in size and four tunnels are formed corresponding to the posterior aspect of the tibia. The common deep compartment previously lodging the tibialis posterior tendon and the flexor digitorum tendon is divided into two tunnels, the most medial corresponding to the tibialis posterior tendon and the lateral to the flexor digitorum longus tendon. Similarly, the deep posterolateral compartment is divided by a septum into two tunnels, the medial for the posterior neurovascular bundle and the larger lateral for the flexor hallucis tendonmuscle. The peroneal tunnel is posterior to the fibula.
The superficial posterior compartment has decreased in size. One clearly sees how the superficial aponeurosis cruris splits to enclose the Achilles tendon and remains adherent at this level to the deep aponeurosis cruris. Both unite laterally with the peroneal compartment.
This level represents the tibial section of the tibiotalocalcaneal tunnel.
Section 2 is 2 cm proximal to the level of the medial malleolus (distal surface of section; Fig. 9.9). The disposition of the compartments is similar to that in Section 3.
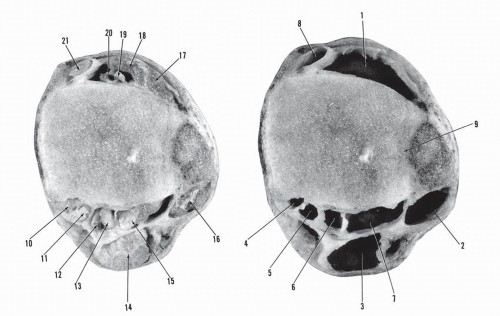
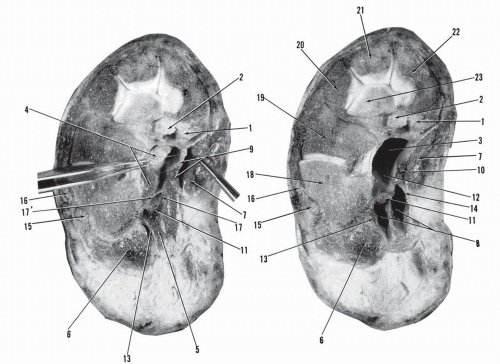
Section 1 is 1 cm proximal to the top of the medial malleolus. This section passes through the malleoli and the talu (distal surface of section; Figs. 9.10 and 9.11).
The tunnel of the tibialis posterior is posterior to the medial malleolus. The tunnels of the flexor digitorum longus, the posterior tibial neurovascular bundle, and the flexor hallucis longus correspond to the posterior aspect of the tibiotalar joint. The peroneal tunnel is located on the posterior surface of the lateral malleolus. The posterior peroneal artery is located in the tunnel of the flexor hallucis longus. The Achilles tendon tunnel has further decreased in size, corresponding to the size of the tendon. Anteriorly, the inferior extensor retinaculum has formed the tunnels of the tibialis anterior, the anterior tibial neurovascular bundles, the extensor hallucis longus, and the extensor digitorum longus.
OBLIQUE SECTIONS OF THE HINDFOOTTARSUS FOLLOWED BY TRANSVERSE SECTIONS OF THE TARSUS AND FOREFOOT IN THE CORONAL PLANE (SEE FIG. 9.1)
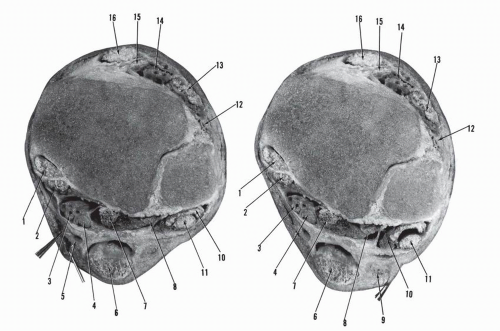
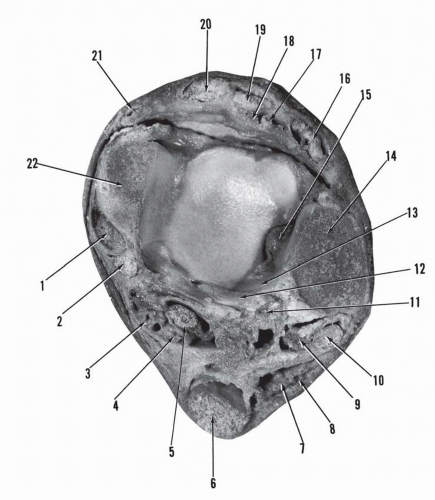
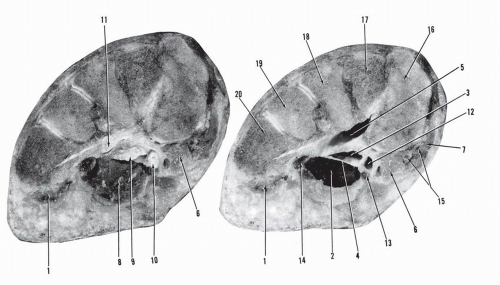
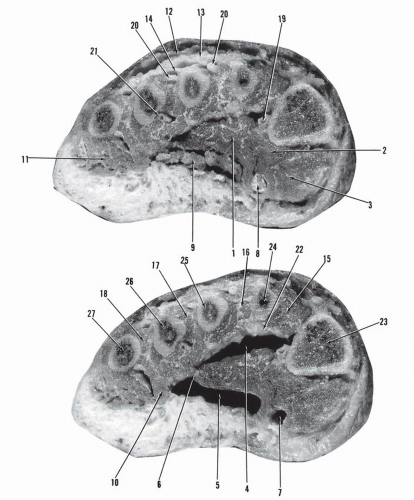
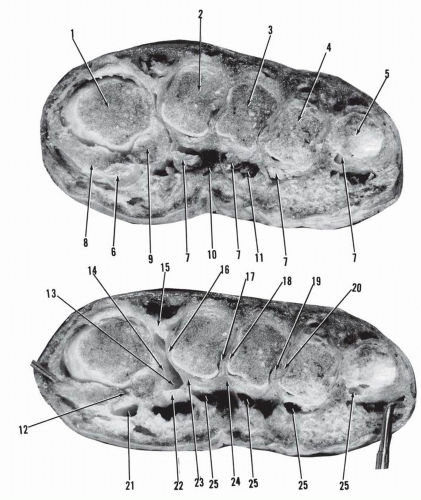
Section I is an oblique section passing through the posterior talocalcaneal joint. The distal surface of section is shown in Figure 9.12.
The tunnels of the tibialis posterior tendon, the flexor digitorum longus, the posterior tibial neurovascular bundle, and the flexor hallucis longus tendons are oriented in a near sagittal plane rather than in a coronal plane as seen in the previous sections.
Section II is an oblique section of the calcaneotalonavicular. The distal surface of this section is shown in Figure 9.13.
The tibialis posterior tendon and its tunnel are applied on the superomedial calcaneonavicular ligament. The flexor digitorum longus and tunnel are located on the medial surface of the sustentaculum tali and the flexor hallucis longus tendon and tunnel occupy the lower surface of the sustentaculum tali. The posterior tibial neurovascular bundle is located in a large sagittally oriented tunnel limited medially by the flexor retinaculum, laterally by the tunnel of the flexor hallucis longus, further posteriorly by the quadratus plantae and its investing fascia, and anteriorly by the tunnel of the flexor digitorum longus.
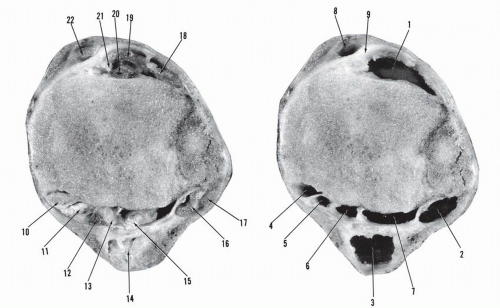
Section III is an oblique section of the calcaneotalonavicular. The dorsal surface of the section is shown in Figure 9.14. This section clearly depicts the calcaneal tunnel. The medial wall of
the tunnel is formed by the abductor hallucis muscle and its investing fascia, the lateral thicker than the medial. The lateral wall is formed by the concave surface of the calcaneus buttressed by the quadratus plantae and its aponeurosis. The interfascicular lamina extends from the fascia of the quadratus plantae to the lateral investing aponeurosis of the abductor hallucis. It divides the calcaneal canal into two chambers: anterosuperior for the medial plantar neurovascular bundle and posteroinferior for the lateral plantar neurovascular bundle. The common tunnel of the flexor digitorum longus and flexor hallucis longus forms the roof of the superior calcaneal chamber. The tibialis posterior tendon has inserted on the tuberosity of the navicular.
the tunnel is formed by the abductor hallucis muscle and its investing fascia, the lateral thicker than the medial. The lateral wall is formed by the concave surface of the calcaneus buttressed by the quadratus plantae and its aponeurosis. The interfascicular lamina extends from the fascia of the quadratus plantae to the lateral investing aponeurosis of the abductor hallucis. It divides the calcaneal canal into two chambers: anterosuperior for the medial plantar neurovascular bundle and posteroinferior for the lateral plantar neurovascular bundle. The common tunnel of the flexor digitorum longus and flexor hallucis longus forms the roof of the superior calcaneal chamber. The tibialis posterior tendon has inserted on the tuberosity of the navicular.
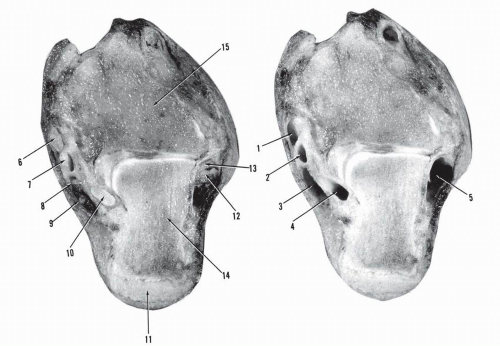
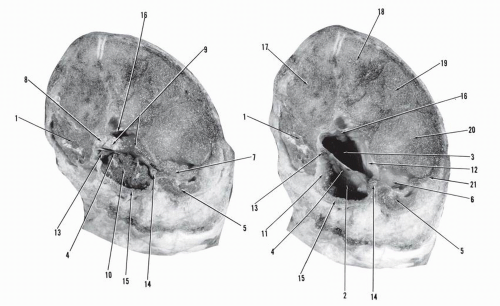
Section IV is an oblique section of the calcaneocubonavicular cuneiforms. The distal surface of section is shown in Figure 9.15. The long flexor tendons have crossed, and the flexor digitorum longus is inferior or plantar to the tendon of the flexor hallucis longus. The medial plantar neurovascular bundle now courses within the medial intermuscular septum. The latter forms the lateral investing layer of the larger abductor hallucis muscle and continues as a septum interposed between the abductor hallucis muscle and the flexor digitorum brevis muscle.
Section V is an oblique section of the calcaneocubonavicular cuneiforms. The proximal surface of the section, distal to section IV, is shown in Figure 9.16.
The flexor hallucis longus is separated from the flexor digitorum longus-quadratus plantae by a septum. The tibialis posterior is insertional. The three compartments of the sole are clearly identified: lateral, central, medial. The lateral compartment lodges the abductor digiti quinti and the medial compartment lodges the abductor hallucis muscle. The central compartment is subdivided into a superficial compartment for the flexor digitorum brevis and an intermediary compartment for the quadratus plantae and the flexor digitorum longus. The medial plantar neurovascular bundle is carried within the medial intermuscular septum. The lateral plantar neurovascular bundle is located between the transverse aponeurosis of the quadratus plantae and a thin aponeurosis that is more superficial.
A different view of section V is provided in Figure 9.17. This figure shows the distal surface of a coronal section through cuboid, cuneiforms1-2-3, and the base of metatarsal 5.
The peroneus longus tendon and its tunnel are under the cuboid and covered by the lateral compartment lodging the abductor digiti quinti. The middle or central compartment is divided by
a transverse septum into the superficial compartment for the flexor digitorum brevis and the intermediary compartment lodging the flexor digitorum longus and the quadratus plantae. The flexor hallucis longus is medial to the flexor digitorum longus. The medial compartment lodging the abductor hallucis muscle is under the first cuneiform. The medial and lateral intermuscular septa are clearly identified. At both insertional sites of the transverse septum of the central compartment are the medial plantar neurovascular bundle on the medial side and the lateral plantar neurovascular bundle on the lateral side. On the most dorsal aspect of the central compartment, a short, sturdy transverse septum is present uniting the apices of the first and third cuneiforms.
a transverse septum into the superficial compartment for the flexor digitorum brevis and the intermediary compartment lodging the flexor digitorum longus and the quadratus plantae. The flexor hallucis longus is medial to the flexor digitorum longus. The medial compartment lodging the abductor hallucis muscle is under the first cuneiform. The medial and lateral intermuscular septa are clearly identified. At both insertional sites of the transverse septum of the central compartment are the medial plantar neurovascular bundle on the medial side and the lateral plantar neurovascular bundle on the lateral side. On the most dorsal aspect of the central compartment, a short, sturdy transverse septum is present uniting the apices of the first and third cuneiforms.
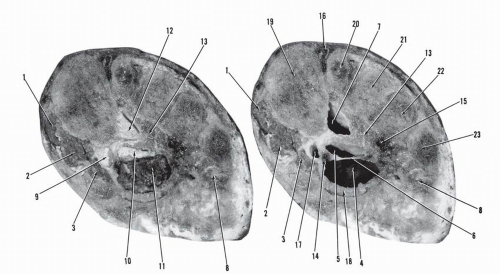
Section VI is a coronal section through cuneiforms1-2-3, the cuboid, and the base of metatarsal 5 (Fig. 9.18). The proximal surface of the section is shown. The disposition of the compartments is similar to that of the previous section. The fifth metatarsocuboid joint is apparent.
The distal surface of section VI is shown in Figure 9.19. This is a coronal section through cuneiform 1 and metatarsal bases 2-5.
The peroneus longus tendon is well represented, crossing obliquely the bases of metatarsals 5-4-3. The flexor hallucis longus has its own tunnel located between the lateral wall of the medial compartment and the medial aspect of the intermediary deep segment of the central compartment. The dividing transverse septum of the latter is now very thin, membranous like. The medial plantar neurovascular bundle is in its own triangular channel within the medial intermuscular septum. The lateral plantar neurovascular tunnel is seen at the lateral end of the transverse membrane, within the lateral intermuscular septum.
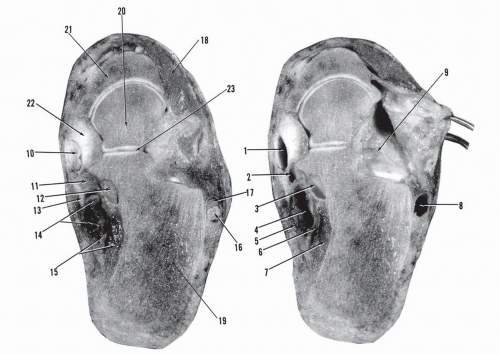
Section VII is a coronal section through cuneiform1 and metatarsal bases 2-5. The proximal surface of the section is shown (Fig. 9.20).
The oblique peroneus longus tunnel and tendon are seen at the base of metatarsals 2-3-4 and at the base of cuneiform 1.
The central intermediary compartment is triangular, lodging the flexor digitorum longus. This compartment is barely separated from the superficial central compartment by the thin transverse aponeurosis. The tunnel of the flexor hallucis longus is clearly delineated, adjacent to the central intermediary compartment and to the tunnel of the medial plantar neurovascular channel on its plantar aspect. The lateral plantar neurovascular bundle is located within the lateral intermuscular septum.
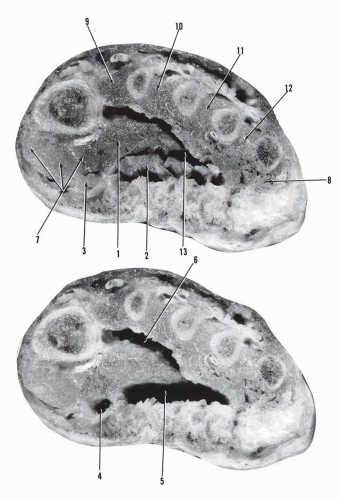
A different view of section VII is provided by Figure 9.21. The figure shows the distal surface of a coronal section through the base of metatarsals 1-5.
The peroneus longus has inserted on the base of the first metatarsal. The origin of the oblique head of the adductor hallucis is seen. The central superficial and intermediary compartments are about to coalesce because the separating membrane is extremely thin. The tunnel of the flexor hallucis longus is again well delineated and located under the first metatarsal. The lateral plantar artery is seen under the fourth metatarsal and deep to the adductor hallucis. The dorsalis pedis artery is between the first and second metatarsal bases dorsally.
Section VIII is a coronal section through the metatarsal shafts 1-5. The distal surface of the section is shown in Figure 9.22.
The oblique head of the adductor is well developed, delineating the beginning of the adductor compartment and space. The superficial and intermediary central spaces have united. The tunnel of the flexor hallucis longus is located between the adductor hallucis and the flexor hallucis brevis lateral head. The metatarsal arteries are seen. The interossei spaces are defined.
Section IX is a coronal section through the mid segment of metatarsal shafts 1-5. The proximal surface of the section is shown in Figure 9.23.
The oblique head of the adductor is well delineated, determining the adductor compartment and dorsally the adductor
space. The thin investing fascia of the adductor inserts laterally on the interossei fascia and separates the adductor space from the central intermediary space. The flexor hallucis brevis, lateral head, is in intimate contact with both the adductor hallucis and the medial head of the flexor hallucis brevis. The intermediary central compartment lodges the flexor digitorum longus, the corresponding lumbricals, and the tendons of the flexor digitorum brevis. The flexor hallucis longus is lodged in a tunnel delineated by the adductor hallucis and the flexor hallucis brevis. The interosseous spaces with the corresponding interossei and intermetatarsal arteries are clearly seen. The lateral compartment is limited to the undersurface of the fifth metatarsal. On the dorsal surface, the superficial dorsal aponeurosis, the extensor digitorum longus-brevis (tendinous with the intertendinous fascia), and the dorsal interossei fascia are demonstrated.
space. The thin investing fascia of the adductor inserts laterally on the interossei fascia and separates the adductor space from the central intermediary space. The flexor hallucis brevis, lateral head, is in intimate contact with both the adductor hallucis and the medial head of the flexor hallucis brevis. The intermediary central compartment lodges the flexor digitorum longus, the corresponding lumbricals, and the tendons of the flexor digitorum brevis. The flexor hallucis longus is lodged in a tunnel delineated by the adductor hallucis and the flexor hallucis brevis. The interosseous spaces with the corresponding interossei and intermetatarsal arteries are clearly seen. The lateral compartment is limited to the undersurface of the fifth metatarsal. On the dorsal surface, the superficial dorsal aponeurosis, the extensor digitorum longus-brevis (tendinous with the intertendinous fascia), and the dorsal interossei fascia are demonstrated.
A different view of section IX is provided in Figure 9.24. The figure shows the distal surface of a coronal section through the mid metatarsal shafts 1-5.
The disposition of the spaces and compartments is similar to that in the previous section.
The adductor compartment and space, the central intermediary compartment, and the interossei compartments are well delineated. The lateral and medial compartments are in very close contact with the adjacent muscles. The tunnel of the flexor hallucis is most superficial.
Section X is a coronal section through the distal segment of the metatarsal shafts 1-5. The proximal surface of the section is shown in Figure 9.25.
The adductor compartment space and the central intermediary compartments are smaller. The sagittal septa of the
plantar aponeurosis projecting into the central intermediary compartment are already seen. The adductor compartment is separate from the medial compartment lodging the flexor hallucis brevis, the flexor hallucis longus, and the adductor hallucis.
plantar aponeurosis projecting into the central intermediary compartment are already seen. The adductor compartment is separate from the medial compartment lodging the flexor hallucis brevis, the flexor hallucis longus, and the adductor hallucis.
The vertical fibers of the plantar aponeurosis projecting into the dermis are seen with abundant plantar veins.
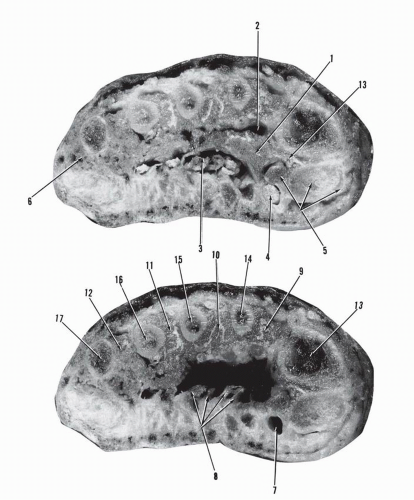
A different view of section X is provided in Figure 9.26. The figure shows the distal surface of a coronal section through the distal segment of the metatarsals 2-3-4 and the heads of metatarsals 1 and 5.
The transverse head of the adductor hallucis is seen. The vertical septa of the plantar aponeurosis have formed near-tunnels to the long flexor tendons of toes 2-3-4. The fibrous tunnels of the flexor hallucis longus and of the long flexor of the fifth toe are demonstrated. The interosseous spaces are well delineated. The adductor space between the interossei and the transverse head of the adductor hallucis is present.
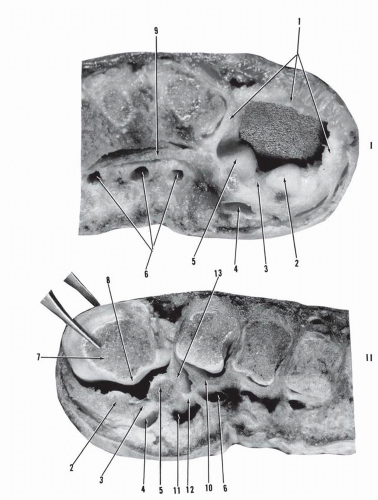
Section XI is a coronal section through the head of the first metatarsal and its sesamoids, the head of the fifth metatarsal, and the necks of metatarsals 2-4. The proximal surface of this section is seen in Figure 9.27.
The transverse head of the adductor hallucis is very thin. The flexor hallucis longus, the flexor digitorum longus, and the corresponding tendons of the flexor digitorum brevis have their own fibrous tunnels. The flexor hallucis longus tunnel is located between the medial and lateral sesamoids. The interossei spaces are present.
The distal surface of the coronal section through metatarso-phalangeal joints 1-4 and the base of the proximal phalanx of the fifth toe illustrates section XI (Fig. 9.28).
The fibrous flexor tunnels are located on the plantar aspect of the corresponding plantar plates. The interossei spaces have disappeared. The interossei tendons are seen in their insertional positions on each side of the corresponding lesser metatarsal head. The dorsal aponeurosis of the first interspace is substantial. The first transverse deep intermetatarsal ligament is well delineated. The plantar neurovascular bundles are seen on the plantar aspect of the plantar metatarsal ligament and are located between the corresponding fibrous flexor tunnels.
Section XI is shown in Figure 9.29. Part I of Figure 9.29 is a close-up view of the coronal section through the sesamoid ring of the big toe (proximal surface of section). Part II of Figure 9.29 is a close-up view of the coronal section through the metatarsal head of the big toe (distal surface of section).
The sesamoid articular surfaces are oriented obliquely and articulate with the corresponding concave metatarsal articular surfaces separated by a crest. The soft-tissue ring with the incorporated sesamoids, the intersesamoid ligament, and the fibrous tunnel of the flexor hallucis longus form a unit. The first deep transverse metatarsal ligament is clearly seen extending from the lateral sesamoid to the fibrous tunnel and the plantar plate of the second toe. The neurovascular tunnel is plantar to the ligaments and the adductor is dorsal to the same.
Section XII is a coronal section through metatarsophalangeal joints 1-4 and the proximal phalanx of the fifth toe. The proximal surface of the section is shown in Figure 9.30.
Three niches for the metatarsal heads are demonstrated. Each niche is formed by the base of the proximal phalanx, the attached capsuloligamentous cuff, and the plantar plate. In the big toe the sesamoids are embedded in the plantar plate.
II. TOPOGRAPHIC ANATOMY
ANTERIOR ASPECT OF THE ANKLE AND DORSUM OF THE FOOT
The anterior aspect of the ankle is a passage zone from the anterior compartment of the leg to the dorsum of the foot. Morphologically, the distal narrow leg gradually enlarges at the bimalleolar level and is in continuity with the foot plate. The latter is convex dorsally in the proximal and mid segments. Distally, at the level of the metatarsal heads, the foot plate is larger and horizontal.
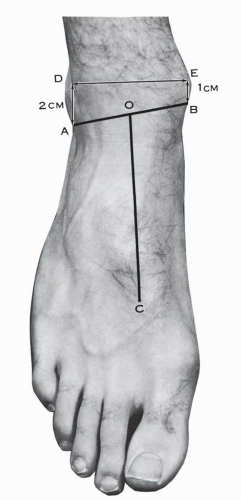
Surface Anatomy
The lateral and medial malleoli are easily palpated. The lateral malleolus is more distal—about 1 cm—and more posterior than the medial malleolus. The bimalleolar axis is thus turned posterolaterally, with an average angle of rotation of 20 to 30 degrees. A line, nearly horizontal, drawn 2 cm proximal to the tip of the lateral malleolus and 1 cm proximal to the tip of the medial malleolus closely delineates the talotibial joint anterior interline (Fig. 9.31).
On the anterior aspect of the ankle, the tendons of the tibialis anterior medially and of the extensor digitorum longus laterally are easily palpated. Lateral to the latter and medial to the former are the medial and lateral premalleolar depressions where the synovium of the ankle joint may bulge in the presence of effusion. Between these two tendons (although deeper) is the tendon of the extensor hallucis longus; the tibialis anterior pulse may be taken just lateral to this tendon. A line drawn from the midpoint of the bimalleolar axis to the tip of the first intermetatarsal space traces the direction of the dorsalis pedis artery when the latter is present in its typical location (see Fig. 9.31). The dorsalis pedis pulse is felt for along this line, lateral to the extensor hallucis longus tendon and distal to the inferior extensor retinaculum. In young individuals the pulse of the first dorsal metatarsal artery may be found in the first intermetatarsal space and felt up to the level of the head of the first metatarsal.
A lateral premalleolar fat pad may be seen and palpated. At the level of the sinus tarsi, a second soft tissue bulge is frequently found, representing the well-developed origin of the extensor digitorum brevis muscle.
A lateral premalleolar fat pad may be seen and palpated. At the level of the sinus tarsi, a second soft tissue bulge is frequently found, representing the well-developed origin of the extensor digitorum brevis muscle.
On the lateral borders of the foot, the tuberosity of the fifth metatarsal is easily found. The calcaneocuboid joint line is one fingerbreadth proximal to this tuberosity. On the medial border of the foot the tuberosity of the navicular is palpated and, farther distally, the tubercle of the first metatarsal base; the latter is located at the midpoint of the medial border of the foot. The talar head is located medially at the midpoint of a line joining the tuberosity of the navicular to the tip of the medial malleolus. A line drawn across the foot from the calcaneocuboid interline to the middle of a line connecting the head of the talus with the tuberosity of the navicular closely locates Chopart’s joint line.1 A line, slightly convex anteriorly, drawn across the foot from the tuberosity of the fifth metatarsal to the tubercle of the first metatarsal base closely corresponds to Lisfranc’s joint interline.1 On the dorsum of the foot, in addition to the digital extensor tendons and the tibialis anterior tendon, the examining hand may palpate the intermediate cutaneous branch of the superficial peroneal nerve, which in certain individuals stands up like a thin, tense cable when the foot is inverted and plantar flexed. This nerve courses in the direction of the third web space.
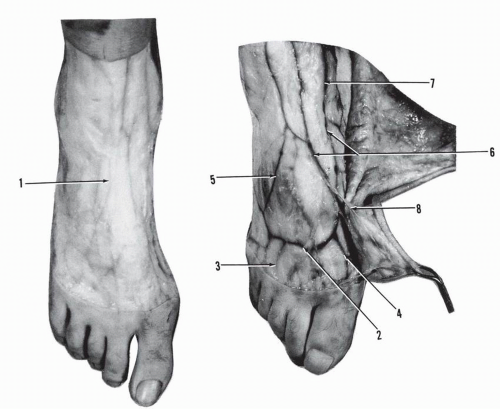
Skin and Subcutaneous Layer and Superficial Veins and Nerves
Skin and Subcutaneous Layer
The skin on the anterior aspect of the ankle and the dorsum of the foot is thin and supple and may be easily moved over the underlying structures. At the level of the lateral border of the foot it is more intimately connected to the subcutaneous tissue and appreciably loses its mobility.
The cleavage lines of the dorsal skin are shown in Figure 9.32. Along the tibial aspect of the leg and across the anterior aspect of the ankle and the dorsum of the big toe, the lines run parallel to the long axis of the foot. In the remaining segment of the dorsum of the foot, the cleavage lines veer laterally, and at the level of the fifth ray, the obliquity of the lines may reach 45 degrees. Around the lateral aspect of the ankle, the cleavage lines follow more or less the contour of the lateral malleolus. Over the lateral and the medial borders of the foot, the lines are longitudinally oriented. Surgical incisions parallel to the cleavage lines leave finer linear scars, whereas incisions at right angles to these lines are subjected to increased tension and may leave wider scars.
The subcutaneous tissue is formed by a loose-meshed connective tissue, lamellar in structure and mobile relative to the underlying structures. It contains a variable amount of adipose tissue. This layer may form a thin transparent fascia covering or carrying the superficial nerves and veins and may be reflected with ease, exposing the superficial dorsal aponeurosis.
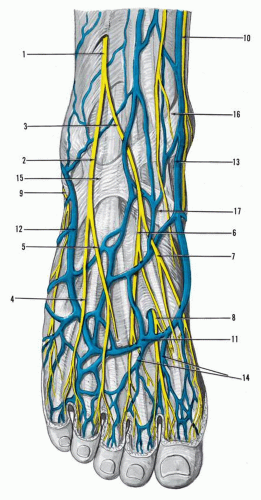
Superficial Veins
The superficial veins of the dorsum of the foot and the anterior ankle are usually superficial to the sensory nerves (Figs. 9.33 and 9.34).2 The venous network is formed centrally by longitudinally and obliquely oriented veins and distally by the dorsal venous arcade, which receives the superficial dorsal metatarsal veins.
The dorsomedial vein of the big toe, a set of parallel superficial veins crossing the medial border of the foot, and the medial deep perforating veins join the proximal medial extension of the dorsal venous arcade to form the greater saphenous vein. The greater saphenous vein courses anterior to the medial malleolus and receives most of the longitudinally oriented dorsal veins from its lateral border. A medial malleolar vein crosses the medial malleolus inferiorly and transversely and unites the greater saphenous vein with the posterior tibial vein.
The medial perforating veins surface between the superior border of the abductor hallucis and the tarsus. They are usually four in number, one located at the level of the cuneo1-metatarsal1 joint, two periscaphoid, and one more proximal, arising from the medial plantar vein.
On the dorsum of the first web space, a perforating vein connects the dorsal venous arcade with the medial end of the deep plantar venous arch. The proximal lateral extension of the dorsal venous arcade receives a set of parallel veins (average number, 15) crossing the lateral border of the foot; this forms the lesser saphenous vein, which courses along the posterior aspect of the lateral malleolus.
The lateral perforating veins join the lesser saphenous vein. They are the peroneal perforating veins, distal and proximal. The distal peroneal perforating vein emerges on the lateral border of the peroneus brevis tendon near its insertion and arises from the dorsal aspect of the calcaneocuboid joint. The proximal peroneal perforating vein originates from the plantar aspect of the calcaneocuboid joint, emerges deep to the peroneus longus tendon, and unites with the lesser saphenous vein. The lesser saphenous vein also receives, from its medial border, the deep lateral malleolar veins that pass under the extensor digitorum longus tendons and unite with the dorsalis pedis vein.
The venous flow in the foot is bidirectional but, when valves are present, the flow is from the depth of the planta pedis to the superficial dorsal system.
Superficial Nerves
The superficial nerves of the dorsum of the foot are provided by the superficial peroneal nerve, the terminal branch of the deep peroneal nerve, the lateral sural nerve, and the saphenous nerve (Figs. 9.33, 9.35, and 9.36).
The superficial peroneal nerve trunk is usually found subcutaneously along the anterior border of the fibula, 10.5 cm above the tip of the lateral malleolus, in the groove between the peroneal group of muscles and the extensor digitorum longus.3 The nerve divides into its terminal branches—intermediate and medial dorsal cutaneous nerves—at an average of 6.5 cm proximal to the tip of the lateral malleolus.3 The intermediate dorsal cutaneous nerve courses along the tibiofibular syndesmosis, passes over the root of the inferior extensor retinaculum, crosses obliquely the fifth and fourth extensor digitorum longus tendons, and courses over the third intermetatarsal space. This nerve can be palpated through the skin. Distally, the nerve divides into the dorsolateral branch of the third toe and the dorsomedial branch of the fourth toe. An anastomotic branch to the sural nerve may be present. The variations of distribution of the sensory nerves are dealt with in Chapter 8.
The medial dorsal cutaneous branch is located laterally over the anterior aspect of the ankle and overlies the extensor digitorum longus tendons. It runs parallel to the extensor hallucis longus tendon, crosses the inferior extensor retinaculum, and, distal to the latter, divides into three branches: lateral, middle, and medial.
The lateral branch obliquely crosses the long extensor tendon of the second toe and bifurcates in the anterior segment of the second intermetatarsal space into the dorsomedial branch of the third toe and the dorsolateral branch of the second toe. The middle branch courses superficially over the first intermetatarsal space and divides into two thin branches supplying the dorsomedial aspect of the second toe and the dorsolateral aspect of the big toe. These two branches are reinforced by the deep peroneal nerve.
The medial branch is directed medially; it crosses the extensor hallucis longus tendon and forms the dorsomedial cutaneous nerve of the big toe. This is the superficial nerve branch that is to be looked for and reflected laterally during the bunionectomy of the big toe through a medial approach.
The intermediate and medial dorsal cutaneous nerves are to be dealt with in the anterolateral approach to the lateral malleolus and the ankle joint, in the anterolateral portal of ankle arthroscopy, in the lateral approach for a triple arthrodesis, in the transverse or longitudinal approach for a tarsometatarsal mobilization, in the midtarsal osteotomy, or in the central metatarsal osteotomies. The longitudinally oriented superficial nerves are most vulnerable in the transverse dorsal incisions.
The saphenous nerve is located on the anterior aspect of the medial malleolus, posteromedial to the greater saphenous vein, and may extend along the medial border of the foot and reach the medial aspect of the big toe.
The sural nerve, after turning around the lateral malleolus, divides into two branches—lateral and medial—at the base of the fifth metatarsal bone. The lateral branch terminates as the dorsolateral nerve of the fifth toe. The medial branch obliquely crosses the long extensor tendon of the fifth toe and forms the dorsomedial branch to the fifth toe. As mentioned previously,
an anastomotic branch may be present between the sural nerve and the lateral division branch of the intermediate dorsal cutaneous nerve.
an anastomotic branch may be present between the sural nerve and the lateral division branch of the intermediate dorsal cutaneous nerve.
Dorsal Aponeurosis and Dorsal Fascial Spaces and Contents
Dorsal Aponeurosis
The superficial dorsal aponeurosis of the foot is encountered after reflection of the skin and the subcutaneous layer carrying the fascia superficialis and the incorporated superficial veins and nerves. This thin, semitransparent layer invests the musculotendinous units, the arteries, and their accompanying deep veins. It is attached to the dorsal skeletal frame medially and laterally and creates a true osteofascial space: spatium dorsalis pedis.4 Laterally, the aponeurosis attaches on the os calcis, the cuboid, and the tuberosity and the lateral border of the fifth metatarsal bone. The medial marginal insertion extends from the sustentaculum tali to the tuberosity of the scaphoid and the medial border of the first metatarsal bone.
The superficial dorsal aponeurosis extends vertical fibers to the skin and closes the dorsal subcutaneous space along its margins. Distally, the thin aponeurosis attaches to the fibrous sheath of the extensor tendons and proximally it is in continuity with the inferior extensor retinaculum.
The inferior extensor retinaculum is a retention system acting as multiple pulleys for the tendons crossing the anterior aspect of the ankle and of the foot, preventing their bowstringing (Figs. 9.37 and 9.38). Their surgical preservation or reconstruction is essential.
At first sight, the delineation of the borders of this retinaculum might not be very clear, because distally it is in continuity with the dorsal aponeurosis and proximally with the distal segment of the aponeurosis cruris and the superior extensor retinaculum. The inferior extensor retinaculum originates from the sinus tarsi and sinus canal with three roots: lateral, intermediate, and medial (Fig. 9.39). The lateral root inserts on the lateral border of the sinus tarsi and over the inferior peroneal retinaculum; it is lateral to the origin of the extensor digitorum brevis muscle. The intermediate root originates in the center of the sinus tarsi, medial to the extensor digitorum brevis muscle and posterior to the cervical ligament. The medial root originates in the sinus tarsi, next to the intermediate root; in the canalis tarsi it is anterior to the interosseous ligament and sends an arm to the talar roof of the tarsal canal. The lateral and intermediate roots envelop the origin of the extensor digitorum brevis, unite, and form the stem of the inferior extensor retinaculum. The medial root courses superomedially and attaches to the deep surface of the stem immediately medial to the extensor digitorum longus tendons, contributing to the formation of the powerful lateral retention sling for these tendons. Anteriorly, the retinacular stem divides into two arms, superomedial and inferomedial. The superomedial arm passes over the tendon of the extensor hallucis longus, covers the tendon of the tibialis anterior, and inserts on the anterior aspect of the medial malleolus. On the medial border of the extensor hallucis longus
tendon, deep retinacular fibers loop around the tendon posteriorly and insert on either the talar neck or the deep surface of the lateral sling. These recurrent fibers form a retention tunnel for the extensor hallucis longus tendon. Farther medially, the superomedial arm of the retinaculum reaches the tibialis anterior tendon and forms two retention systems: superior and inferior. The superior tunnel has a very thin or absent superficial cover, whereas the deep layer is thick and inserts on the medial malleolus. The inferior tunnel is well structured. The anterior and posterior walls of the tunnel unite on the medial border of the tendon and insert on the anterior aspect of the medial malleolus.
tendon, deep retinacular fibers loop around the tendon posteriorly and insert on either the talar neck or the deep surface of the lateral sling. These recurrent fibers form a retention tunnel for the extensor hallucis longus tendon. Farther medially, the superomedial arm of the retinaculum reaches the tibialis anterior tendon and forms two retention systems: superior and inferior. The superior tunnel has a very thin or absent superficial cover, whereas the deep layer is thick and inserts on the medial malleolus. The inferior tunnel is well structured. The anterior and posterior walls of the tunnel unite on the medial border of the tendon and insert on the anterior aspect of the medial malleolus.
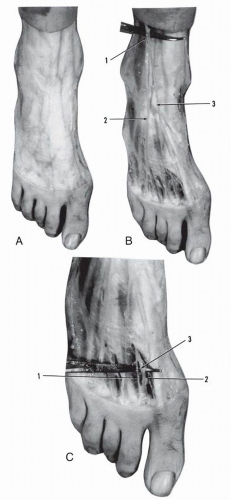
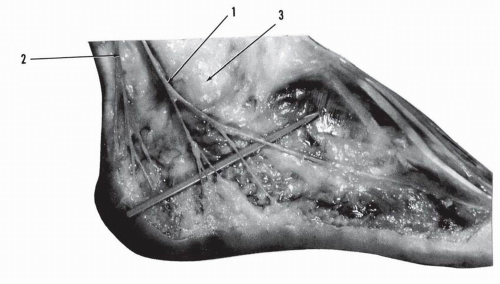 Figure 9.36 Sural nerve. (1, sural nerve trunk; 2, lateral calcaneal nerve, branch of sural nerve; 3, premalleolar fat pad). |
The inferomedial arm of the retinaculum courses anteromedially and reaches the medial border of the foot at the level of the cuneonavicular joint. The fibers pass over the dorsalis pedis vessels, the deep peroneal nerve, and the extensor hallucis longus tendon—and, as they reach the tibialis anterior tendon, they form a terminal tunnel for the latter. This segment of the retinaculum splits into deep fibers, which insert on the navicular and medial cuneiform, and superficial fibers, which are in continuity with the investing fascia of the abductor hallucis muscle.
In 25% of the cases the inferior extensor retinaculum has an oblique superolateral extension band that gives to the retinaculum a cruciate configuration. This band originates from the lateral sling, from the superomedial band, or from both. It courses upward and laterally and inserts on the lateral surface of the lateral malleolus and the lateral crest of the lower segment of the fibula.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree