Musculoskeletal ultrasonographic evaluation of the proximal lower limb includes the evaluation of the soft tissue structures, including tendons, ligaments, or muscles, and the bony structures of this region, include the hip, pubic symphysis, and sacroiliac joints. The evaluation of the hip or proximal lower limb region can be performed in an efficient and systematic manner. Ultrasonography of the lateral hip, intra-articular hip, medial thigh, and posterior thigh are discussed in the article.
Musculoskeletal ultrasonographic evaluation of the proximal lower limb includes the evaluation of the soft tissue structures, including tendons, ligaments, or muscles, and the bony structures of this region, include the hip, pubic symphysis, and sacroiliac (SI) joints. The hip or proximal lower limb includes not only the tendon insertions/origins, ligaments, and bony articulations but also the large neurovascular bundles tracking through this region to the distal limb. This bundle includes femoral, obturator, and sciatic nerves as well as the femoral artery, veins, and lymphatics. All these structures can be visualized using dynamic ultrasonography to detect pathology as well as to guide injection treatments.
Body habitus can preclude direct visualization of the intra-articular hip if adequate probe types are not available. This may require a curved array probe and low-frequency scanning to provide a greater depth of penetration and field of view to optimize views. Ultrasound-guided interventions have been described for the SI and hip joints as noted in later discussion.
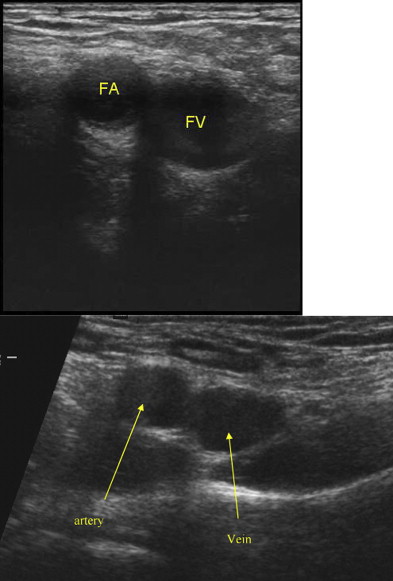
The evaluation of the hip or proximal lower limb region can be performed in an efficient and systematic manner. The lateral hip region contains the insertions of the gluteus medius and minimus tendons onto the greater trochanter, the iliotibial band (ITB) that crosses through this region as well as multiple bursae that are localized in this region. The anterior and anteromedial regions contain the muscle and tendon of the rectus femoris; the hip flexor tendon; and the femoral artery, nerve, vein, and lymphatics ( Fig. 1 ). In addition, the anterior position is used to visualize the hip joint and capsule, acetabulum and pubic symphysis can be imaged and scored for pathology or for guided interventions. These views are amenable to guided injections. The medial thigh region contains the origins of the adductor tendons and insertion of the pectineus, and it can be used to assess the fibers from the abdominal oblique muscles to assess for lesions associated with sport hernias. Inguinal herniations can also be noted in the anteromedial groin. Posteriorly, the insertion of the hamstring tendons, the muscle architecture of the gluteus maximus (Glut max), the SI joint, and the sciatic nerve can be visualized.
Lateral hip
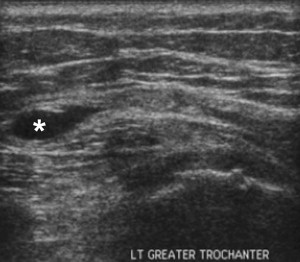
The greater trochanter is a bony landmark of the lateral hip region and provides an acoustic landmark for the lateral hip that helps the sonographer to orientate toward the soft tissue structures that run across this region and attach to this landmark. Anatomic landmarks of the greater trochanter are divided into 4 facets: anterior, lateral, superolateral, and posterior ( Fig. 2 ). Hip abduction occurs via 2 clinically important muscles: gluteus medius and gluteus minimus. The gluteus medius tendon has not only a broad attachment on the lateral facet but also a narrower attachment on the superolateral facet. The gluteus minimus is covered by the medius and inserts into the anterior facet of the greater trochanter ( Fig. 3 ). Gluteal tendinopathy is a common cause of lateral hip pain; therefore, these structures should be visualized during ultrasonography. As with all tendons, these structures need to be evaluated along the length and width of the tendons using longitudinal and transverse views. Diligent scanning must be used to account for potential anisotropy leading to false-positive findings. The posterior aspect of the greater trochanter is the location of the greater trochanteric bursa, which should be scanned for signs of inflammation such as fluid in the bursa and thickening of the bursal sac. Bursae are usually collapsed and difficult to identify during ultrasonography. Some bursae may have a tiny amount of hypoechoic fluid, separating the adjacent hyperechoic bursal walls.

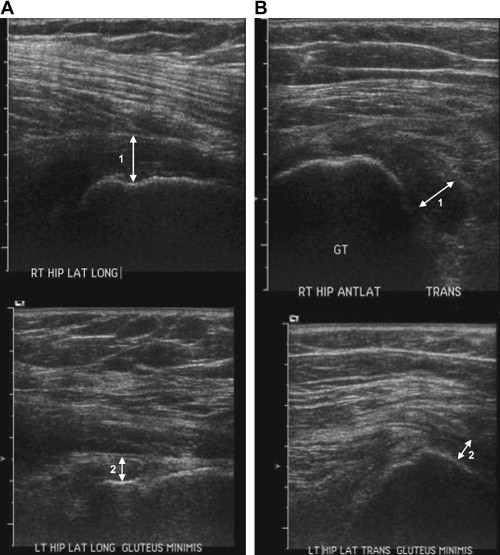
When scanning this region, the patient should be placed in a lateral recumbent position on the examination table, with the area to be scanned pointing upward. This positioning provides both patient and examiner comfort, which ultimately results in optimal imaging. Then, by either palpating or scanning the posterolateral femur transversely in a caudal to cephalad direction, the greater trochanter comes into view and is noted as a bony protuberance. Facet anatomy is well demonstrated on ultrasonography and assists in identifying the key structures in this region. From the transverse position, the sonographer then orientates the probe into a coronal oblique angle over the posterolateral greater trochanter. Here, the anatomy of the trochanteric bursa (trochanteric subgluteus maximus bursa) is variable and may be present adjacent to the posterior facet of the greater trochanter or between the lateral facet and the ITB. If there is no distention of the bursa, it usually appears as a thin, uniform, 1-to-2 mm hypoechoic region and deep to the Glut max and iliotibial tract. Trochanteric fluid would be seen posterolateral to the greater trochanter and deep to the Glut max. Visualizing the bursa is best when there is fluid or distention of this structure, making it obvious ( Fig. 4 ). Distention does not necessarily indicate inflammation; however, pain with pressure from the probe or increased flow on color or power Doppler imaging is suggestive of inflammation or bursitis. Maintaining the probe in a longitudinal plane and sliding anteriorly should bring the lateral or superolateral facet of the greater trochanter into view, thereby bringing the gluteus medius tendon into view on long axis. The long-axis view is the most important view when imaging tendons for pathologic conditions. Because of the fibrillar appearance of the tendons, any disruption of this pattern is easily evident and usually indicates a pathologic condition. Pain overlying this region has classically been considered and diagnosed as greater trochanteric bursitis. However, there is evidence that tendinopathy and tearing of the gluteus medius and gluteus minimus tendons are the usual cause of greater trochanteric pain syndrome. From this view, the gluteus medius can be seen inserting onto the lateral and superolateral facets of the greater trochanter. Scanning the length and anteroposterior margins of this tendon should be performed, noting for tendon thickening, hypoechoic regions, calcifications, and underlying cortical irregularity, which are diagnostic of tendinopathy. While continuing in a long-axis orientation but more anteriorly (coronal oblique position of the probe), the gluteus minimus is appreciated, lying deep to the gluteus medius muscle and inserting onto the anterior facet of the greater trochanter. When scanning the tendons, the goal is to scan the tendon from the musculotendinous origin to the “bird’s beak” appearance of the insertion on the greater trochanteric facet (see Fig. 2 ). Within these imaging windows, the iliotibial tract can be appreciated as it superficially extends from the proximal hip to the distally along the lateral thigh. Imaging of the tendons needs to be performed in both the long (longitudinal to the tendon fibers) and short (cross-sectional) axes. Therefore, during the examination of the lateral hip, the sonographer should rotate the probe 90° from the long-axis positions to view the cross section of the tendons. Scanning the superior (proximal) and inferior (distal) portions of the tendon needs to be examined. In these views, the gluteus minimus, gluteus medius, and ITB can be seen in a signal window.
Therapeutically, if pathology is noted on ultrasonography, whether it is subgluteus maximus bursitis or gluteus medius tendinosis, guided-injection therapy can be performed conveniently and immediately. Precise guidance of injections to the areas of pathology is inherently important when performing regenerative injections such as platelet rich plasma (PRP) injection. Activation and healing response of the platelets are initiated by contact with the damaged tissue. Therefore, proper placement of the biologic graft directly into the pathologic site is an important aspect of this new therapy. This treatment has been shown to have benefits in treating recalcitrant lateral epicondylosis, a common tendinopathy of the lateral extensor tendons of the elbow.
Intra-articular hip
The hip joint is imaged anteriorly; therefore, the patient should be asked to lay in a supine position for examination of the anterior structures. The deep anatomy of the hip joint requires a lower-frequency ultrasound setting and may require a curved array probe, particularly in the heavier patient, for optimal visualization of this structure.
Localizing the hip joint can be accomplished by imaging the femoral shaft in a transverse plane and moving proximally until the lesser and greater protuberances appear in the image. Then the probe is rotated to a sagittal oblique plane, the rounded surface of the femoral head and shoulder comes into the image, and the femoral neck is viewed longitudinally.
Another approach to the hip joint that was described by Smith and Hurdle provides a step-by-step approach to intra-articular hip injection using ultrasound guidance ( Fig. 5 ). The investigators describe placing the transducer medial to the anterosuperior iliac spine in a sagittal plane. From this position, the transducer is moved medially until the hyperechoic cortical rounded surface of the femoral head is seen. Centering the superior portion of the transducer on the femoral head (in a sagittal plane) and rotating the inferior portion laterally (sagittal oblique plane) bring the long axis of the femoral neck into view. In this plane, the fibers from the iliofemoral ligament as well as the hyperechoic fibrocartilage of the anterior hip labrum can be studied. Evaluation of the labra tear has been studied. Troelsen and colleagues described visualizing the labraltear in 2 studies aimed at using ultrasonography to detect acetabular labral tear. The investigators maintained the transducer parallel to the femoral neck with identification of the femoral head and neck. The transducer is moved medially and laterally and tilted in both ways providing a comprehensive evaluation of the anterior labrum. The leg can be moved into flexion, adduction, and internal rotation during examination. This dynamic examination was used to reveal labral detachment in a study by Troelsen and colleagues. Their criteria for labral tears were displacement or absence of the labrum, a hypoechoic cleft through the base of the labrum causing detachment with or without displacement, intrasubstance hypoechoic linear clefts, and intrasubstance hypoechoic, cystic, or irregular formations. Mixed echogenicity without definite tearing and irregular margins was interpreted as degenerative changes. Troelsen and colleagues found labral tears in 17 out of 18 hip joints when studied under ultrasonography. Of these, 16 were confirmed by magnetic resonance arthrography, with 1 false-positive and 1 false-negative finding. The investigators claimed that ultrasonography in the diagnosis of labral tear had a sensitivity of 94% and a positive predictive value of 94%.

The hip joint is noted when the acetabulum, femoral head, and femoral neck are all in the same scanning window. From these superficial views to the femoral neck, the anterior recess of the joint can be appreciated ( Fig. 6 ). Evaluation of this region is important when attempting to diagnose effusion or synovitis. The normal measurement of this recess is 5 mm. Measurements greater than 5 mm or layers of hypoechoic fluid are consistent with the diagnosis of effusion. The recess should also be examined in the transverse plane.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








