High-frequency diagnostic ultrasonography of the hand, wrist and elbow has significant potential to improve the quality of diagnosis and care provided by neuromuscular and musculoskeletal specialists. In patients referred for weakness, pain and numbness of the hand, wrist or elbow, diagnostic ultrasonography can be an adjunct to electrodiagnosis and help in identifying ruptured tendons and treating conditions such as carpal tunnel syndrome or trigger finger. Use of a small high-frequency (>10–15 MHz) transducer, an instrument with a blunt pointed tip to enhance sonopalpation and a model of the hand, wrist and elbow is advised to enhance visualization of small anatomical structures and complex bony contours. A range of conditions, including tendon and ligament ruptures, trigger finger, de Quervain tenosynovitis, intersection syndrome, lateral epicondylitis, and osteoarthritis, is described along with detailed ultrasonography-guided injection techniques for carpal tunnel syndrome and trigger finger.
For the physiatrist with a busy electrodiagnostic practice, ultrasonography of the hand, wrist, and elbow provides a natural transition into the realm of musculoskeletal diagnostic and interventional ultrasound. The anatomy is familiar and accessible, and its visualization frequently provides complementary information with regard to the chief complaint and how it is related to the electrodiagnostic findings. Over time, as the physiatrist develops expertise and is able to provide unique and useful information using diagnostic ultrasound, specific referrals for musculoskeletal diagnostic ultrasound are likely to ensue.
Musculoskeletal diagnostic ultrasonography of the hand, wrist, and elbow presents some unique challenges. The anatomy is small and superficial, so it is best if the smallest possible transducer with the highest possible frequency is used (>10–15 MHz). We (the authors of this article) find it useful to use a small instrument such as a curved hemostat or the tip of one’s little finger to enhance accuracy while palpating small structures. Careful handling of the transducer, use of adequate gel, and/or a standoff pad is required to maintain contact with the skin and obtain optimum images. We also find it useful to place for reference an anatomic model of the hand and wrist next to the patient and ultrasound machine to enhance visualization of complex anatomy such as the bony contours of the carpal bones ( Fig. 1 ).

Anatomy
The skeleton of the hand, wrist, and elbow includes the distal humerus, the radius and ulna, the proximal carpal row, including the scaphoid, lunate, triquetrum, and pisiform, the distal carpal row, including the trapezium, trapezoid, capitate, and hamate, and the metacarpals and phalanges. The proximal carpal row serves as a rigid intercalated segment in the wrist kinetic chain and forms a semirigid ring with the distal carpal row. The distal radius has a biconcave articulation with the proximal carpal row, allowing wrist flexion and extension and radial and ulnar deviation. The distal radioulnar joint allows the radius to rotate around the ulna during forearm pronation and supination.
The elbow is a compound joint, consisting of the humeral trochlea and ulnar coronoid process (hinge) and humeral capitellum and radial head (ball and plate) joints, providing elbow flexion and extension and forearm pronation and supination. The thumb is highly mobile because of the saddle shape of its trapezium and rounded dorsal aspect of its proximal metacarpal. By contrast, the carpal-metacarpal joints of the index and middle fingers are immobile while the carpal-metacarpal joints of the ring and little fingers are somewhat mobile, providing approximately 15° and 30° of flexion to allow them to move closer to the thumb.
More than 100 ligaments stabilize 20 bones and 41 joints in the hand, wrist, and elbow. The collateral ligaments of the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints provide stability during flexion and extension. The metacarpophalangeal (MCP) collateral ligaments tighten in flexion and loosen in extension, allowing radial and ulnar deviation of the fingers in extension. The dorsal and volar scapholunate and lunotriquetral ligaments are important stabilizers of the proximal carpal row, while the intercarpal ligaments stabilize the distal carpal row.
At the floor of the carpal tunnel, the scaphotrapeziotrapezoideum (STT), radioscaphocapitatum (RSC), radiolunotriquetrum (RLT), and triquetrohamatocapitatum (THC) ligaments provide stability to the radiocarpal joint and the proximal and distal carpal rows. Experimental sectioning of the RSC in cadavers has resulted in dorsal intercalated segment instability (DISI). The ulnolunate and ulnotriquetral ligaments are the most important stabilizers of the ulnar aspect of the wrist.
The radius and ulna have a reciprocal load-bearing relationship in the upper extremity: the ulna has a broad articulation proximally and a narrow one distally, whereas the radius has a broad articulation distally and a narrow one proximally. The diagonally oriented fibers of the interosseus membrane transmit load from the distal radius to the proximal ulna during axial loading of the hand, but at least 15% of the load depending on wrist position is transmitted directly to the ulna. To facilitate weight bearing, the meniscus homologue of the triangular fibrocartilage broadens the contact area between the proximal carpal row and the distal ulna.
The medial elbow is stabilized by the ulnar collateral ligament (UCL) with its anterior, posterior, and inferior components, the anterior of which is the most important and spans between the medial epicondyle and a tubercle on the coronoid process. The lateral elbow is stabilized by the radial collateral and annular ligaments.
The muscles of the volar aspect of the hand, wrist, and elbow include the flexor digitorum superficialis (FDS), flexor digitorum profundus (FDP), and flexor pollicis longus (FPL), whose tendons pass through the carpal tunnel along with the median nerve, the flexor carpi radialis (FCR) and flexor carpi ulnaris (FCU), the pronator teres (PT) and pronator quadratus, and the palmaris longus (PL). The FCR, FDS, PL, and FCU have a common flexor tendon originating from the medial epicondyle. The FDS tendons split at the proximal phalanx before inserting onto the middle phalanx, while the FDP tendons course through this split to insert onto the distal phalanx. Five annular and 3 cruciate pulleys prevent the flexor tendons from bowstringing.
The lumbrical muscles serve to modulate flexion and extension at the MCP joints. The palmar interossei adduct the fingers while the dorsal interossei abduct them. Each lumbrical muscle takes origin from an FDP tendon and inserts along with the interossei onto the middle and distal phalanges by way of the lateral bands. The abductor pollicis brevis (APB) and flexor pollicis brevis (FPB) abduct and flex the thumb while the adductor pollicis (AP) adducts it. Similarly, at the hypothenar eminence, the abductor, flexor and opponens digiti minimi abduct, flex, and oppose the little finger.
The brachioradialis (BR) and extensor carpi radialis longus (ECRL) originate from the distal lateral humerus, whereas the extensor carpi radialis brevis (ECRB), extensor digitorum communis (EDC), extensor digiti minimi (EDM), and extensor carpi ulnaris (ECU) originate in a common extensor tendon on the lateral epicondyle. The extensor indicis (EI) originates from the proximal ulna and interosseus membrane and inserts onto the middle and distal phalanx of the index finger. At the MCP joints, the central tendon slips of the EDC insert by way of sagittal bands down to the volar plates for better leverage in extending the proximal phalanx. The central tendon slips continue onto the middle phalanx while the lateral bands converge onto the distal phalanx.
The distal biceps tendon inserts on the radius while the brachialis inserts on the ulna. The supinator has a superficial head originating from the lateral epicondyle and proximal ulna and inserting next to the bicipital tubercle of the radius, and a deep head originating from the proximal ulna and inserting opposite the PT on the radius. The triceps tendon inserts onto the olecranon. Its anterior fibers originate from the medial head and posterior fibers from the lateral and long heads. The anconeus muscle originates from the lateral epicondyle and inserts on the olecranon.
The median nerve courses medial to the brachial artery at the elbow, passes under or between the two heads of the pronator teres, courses between the FDS and FDP muscles in the forearm and then enters the carpal tunnel along with their tendons and the FPL. The ulnar nerve enters the forearm deep to the two heads of the FCU and courses under it all the way to the wrist. The radial nerve enters the forearm under the BR and then splits into its deep and superficial components. The deep radial nerve courses between the superficial and deep heads of the supinator to become the posterior interosseus nerve. The superficial radial nerve continues under the BR to the hand dorsum. The common digital nerves arise from the terminal median and ulnar nerves and split at the metacarpal heads to become the proper digital nerves.
Although a comprehensive review of the musculoskeletal ultrasonography of the hand, wrist, and elbow is beyond the scope of this article, our goal is to provide a physiatric perspective and overview, starting distally and moving proximally.
Ultrasonography of the hand, wrist, and elbow
Tendon ruptures are the most common reason for musculoskeletal ultrasonography referrals from hand surgeons to our practice. The identification of ruptured tendon ends and whether the rupture is complete or incomplete is rewarding, yet time consuming. In these cases, it is often useful to scan the normal contralateral or a similar finger for comparison.
Ultrasonography findings of tendon rupture include loss of or replacement of the regular hyperechoic fibrillar tendon pattern with irregular hypoechoic fluid and debris. It is important to scan the tendon sheath in the long and short axes to identify the ruptured tendon ends. When the rupture site is identified, careful inspection and palpation along the tendon may reveal a subtle step-off defect, further confirming the diagnosis.
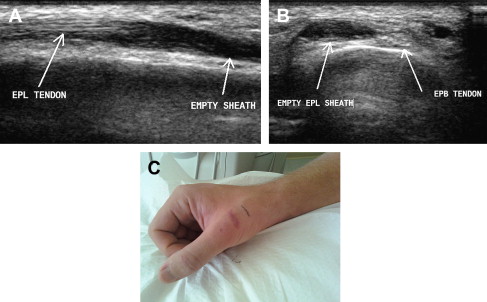
Extensor pollicis longus (EPL) tendon ruptures may occur in association with tendon degeneration, rheumatoid arthritis, previous fractures of the distal radius, or penetrating trauma, and may result in loss of ability to extend the interphalangeal (IP) joint of the thumb. In the setting of a prior surgical attempt to repair the tendon, the differential diagnosis includes failure of repair, rerupture, scarring, or contracture ( Fig. 2 ).
Rupture of one of the EDC tendons resulting from high-velocity axial loading of an extended finger is referred to as baseball or mallet finger. The tendon avulses from its distal insertion at the proximal aspect of the distal phalanx, often taking a piece of bone with it. Ultrasonography reveals absence of echoes at the usual location of the distal tendon, and lack of visualization of tendon movement on passive flexion and extension of the DIP joint. The distal tendon tip, often including a hyperechoic-appearing speck of avulsed bone, can be found more proximally, typically at the level of the middle phalanx. The possibility of an associated fracture of the phalanx must be considered for this and all other tendon injuries involving high-velocity trauma.
Rupture of the central slip of the extensor tendon at the proximal middle phalanx precipitates subluxation of the lateral bands to each side with the eventual development of Boutonniere deformity. Ultrasonography has the potential to identify these ruptures early, leading to appropriate treatment and prevention of progressive deformity.
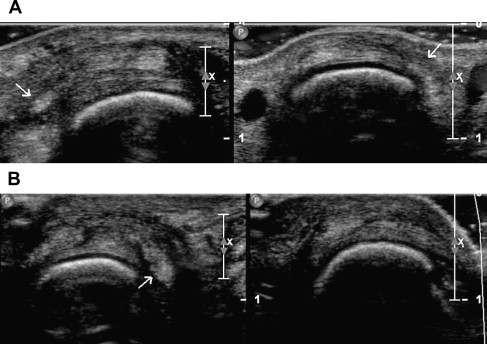
Extensor hood injuries at the MCP joints, including tears of the sagittal bands, are known as boxer’s knuckle. These injuries occur as a result of acute or repetitive trauma from punching with a clenched fist and are characterized by impairment of finger extension at the MCP joint ( Fig. 3 ). Differential diagnosis includes fracture, contusion, synovitis, collateral ligament injury, and capsular tear. Dynamic ultrasonography reveals either subluxation or dislocation of the extensor tendon from its midline position opposite the side of sagittal band rupture or, if two tendon slips are present, separation of the slips with each slip subluxing to one side.
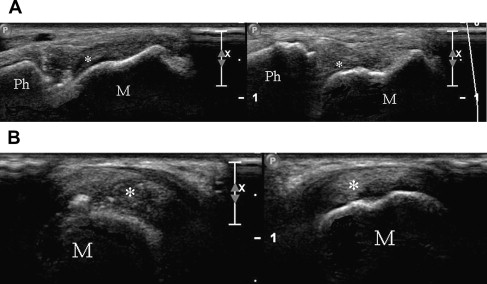
Ruptures of the lateral collateral ligaments of the MCP joints of the fingers can be diagnosed with ultrasonography ( Fig. 4 ). The collateral ligaments take origin from small concavities at the dorsal aspect of the metacarpal heads. Because the location of the ligaments is dorsal to the axis of rotation, they become tight when the finger is flexed and relaxed when the finger is extended.
Flexor tendons can rupture in their mid-substance as a result of degeneration or penetrating trauma, resulting in loss of active flexion at the DIP, PIP, or IP joints. Ultrasonography reveals a discontinuity in the regular hyperechoic tendon fibrillar pattern ( Fig. 5 ). Finding the proximal end of a ruptured flexor tendon can be especially challenging when the tendon has retracted into the wrist. The search for the tendon can be facilitated by comparison with the unaffected contralateral side. Once the ruptured tendon ends have been found, their location has to be identified at a specific distance from an easily identifiable landmark such as the MCP or radioscaphoid joint, which can be identified later using fluoroscopy equipment in the operating room.
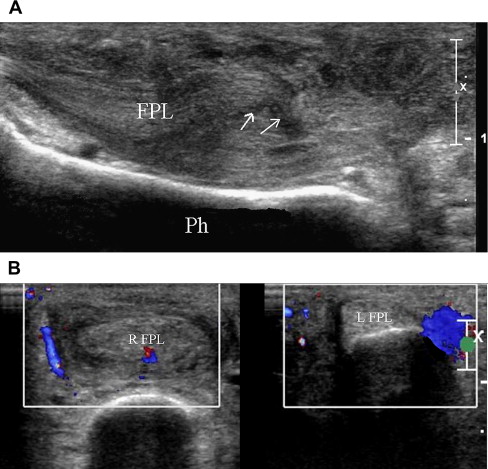
FDP tendon rupture, occurring as a result of acute loading such as grabbing another player’s shirt during football or rugby, is known as jersey finger. On examination, the patient cannot actively flex the DIP joint. Ultrasonography reveals a fragment of bone marking the distal tendon end next to a hypoechoic empty distal tendon sheath. Five types of jersey finger have been described, with the tendon retracting into the palm (type I), lodging at the PIP joint (type II) or at the fourth annular pulley because of a bony avulsion (type III), separating from the avulsion and retracting into the palm (type IV), or involving a fracture of the distal phalanx (type V).
Five annular and 3 cruciate pulleys hold the FDP and FDS tendons in place. Pulley ruptures are common among rock climbers and in occupations involving high finger flexion forces. The most commonly ruptured pulley is the second annular (A2), located in the middle of the proximal phalanx. Dynamic scanning reveals bowstringing of the flexor tendons and the ruptured pulley.
Trigger finger occurs as a result of a mismatch in size between the A1 pulley and the flexor tendons. Besides classic triggering, symptoms may include a vague sense of tightness in the fingers, pain in the palm of the hand, or a fixed flexion deformity of the finger. More subtle presentations include weakness of finger flexion or extension or pain in the thenar eminence. We have found trigger finger to be the cause of the chief complaint in some patients referred for electrodiagnostic consultation, with the only finding being tenderness at the A1 pulley.
Ultrasonography findings of trigger finger include hypoechoic thickening and hypervascularization of the A1 pulley, focal enlargement of the tendons and tendinosis, an associated ganglion cyst, or an abnormality of the volar plate. Treatments have included use of a splint, blind or ultrasonography-guided corticosteroid injections, percutaneous release, and open surgery.
Bodor and Flossman used a short-axis, ultrasonography-guided trigger finger injection technique, noting complete resolution of symptoms in 90% of patients at 1 year following a single injection, which was statistically significant compared to the approximately 56% success rate reported for blind injections.
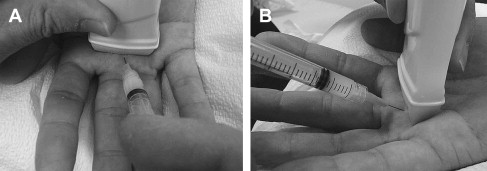
Using this technique, the patient is asked to sit across from the examiner and next to the ultrasound machine with the palm up on a pillow. First, the MCP joint is identified in the long axis and placed in the middle of the screen, and then the transducer is rotated 90° to obtain the short-axis view ( Fig. 6 ). At this location, the underlying distal metacarpal bone appears convex, in contrast to the proximal phalanx that appears concave. Careful scanning back and forth between these two surfaces reveals a hypoechoic interval, which is the joint space. It is a good idea to practice this maneuver; the visual and scanning skills learned are useful in visualizing other structures such as the triangular fibrocartilage of the wrist, the medial meniscus of the knee, and the cervical zygapophysial (facet) joints.

The A1 pulley is visualized at the MCP joint along with a triangle consisting of the pulley, the flexor tendons, and the metacarpal bone (see Fig. 6 ). Using a slightly angled (70° coronal, 45° sagittal) short-axis approach ( Fig. 7 ), we aim for the middle of the triangle and insert a 30-gauge, 25-mm needle. As soon as the needle enters the skin, we inject lidocaine 4% (0.25 mL) to provide near-instant anesthesia while advancing the needle slowly toward the target triangle using real-time ultrasound guidance. When the tip of the needle is under the A1 pulley and inside the triangle ( Fig. 8 ), we inject a little more lidocaine to ensure good flow; if not the needle is adjusted or replaced with a larger gauge one. The syringes are then switched and 0.5 to 1 mL of a mixture of 2:1 triamcinolone acetonide 40 mg/mL and lidocaine 4% is injected.
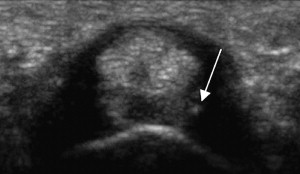
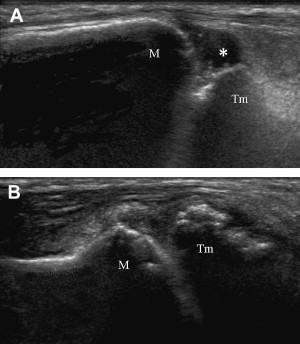
The carpometacarpal (CMC) or trapezium-metacarpal joint of the thumb is the most common site of symptomatic osteoarthritis in the hand. Ultrasonography may show effusion, osteophytes, and subluxation ( Fig. 9 ). A short-axis, ultrasound-guided approach minimizes discomfort when injecting corticosteroid or viscosupplement. A randomized controlled trial of hylan G-F 20 versus saline injections in women with bilateral CMC joint arthritis found statistically significant improvements in pain and function at 6 months. Another study found that a single ultrasonography-guided injection of hyaluronic acid resulted in half the patients not requiring nonsteroidal anti-inflammatory drugs at 1-month follow-up.
Gamekeeper’s or skier’s thumb involves the UCL of the thumb, and occurs after a fall onto the extended abducted thumb. Gripping and holding reproduces the pain, and tenderness is present at the thumb MCP joint medial joint line. Martinoli describes 3 grades of injury: (1) distal insertion rupture with avulsion of a speck of bone from the proximal phalanx; (2) mid-substance rupture with the ligament ends contained by the adductor pollicis fascia; (3) rupture with displacement of the proximal end of the ligament away from the distal end and above the adductor fascia, referred to as a Stener lesion and which requires surgery. Identification of Stener lesion requires careful scanning and an intimate understanding of the anatomy, covered in several excellent texts.
The scaphoid-trapezium-trapezoid (STT) and pisotriquetral (PT) joints are often affected by osteoarthritis, and result in pain at the base of the thumb and ulnar aspect of the wrist. Injections to the STT joint are best done via a dorsal approach and to the PT joint via a medial approach. Correlation with an anatomic model of the hand and wrist is useful before performing an injection.
Carpal tunnel syndrome (CTS) is a common reason for hand, wrist, and elbow referrals to physiatrists. For most of the patients referred to us with this condition, we provide electrodiagnostic testing, education, and ultrasound-guided carpal tunnel injections. Before any injections, we assess the location of the median nerve, assess its cross-sectional area and mobility, and assess whether bowing of the flexor retinaculum or a median artery is present. We have performed more than 1800 ultrasound-guided carpal tunnel injections between 2003 and 2010 with only 1 complication: infection resolving with antibiotics in a patient with a previous history of infection.
We typically use a short-axis technique similar to our approach for trigger finger, but with a slightly steeper angle in the sagittal plane. The patient is seated across from the physician, and the hand is in supination and resting on a pillow ( Fig. 10 ). The fingers are flexed to maximize space between tendons (which taper distally) and relaxed to minimize tendon tension and allow the needle to pass more easily between them. A short-axis view of the median nerve and flexor tendons is then obtained at the distal wrist crease ( Fig. 11 ). A diagonal cleft between flexor tendons is identified and centered on the screen. This cleft or opening between tendons is typically located halfway between the median and ulnar nerves and between the middle and ring finger flexor tendons; however, in a minority of the population, the nerve lies more medially, and a cleft or opening lateral to the nerve has to be used.
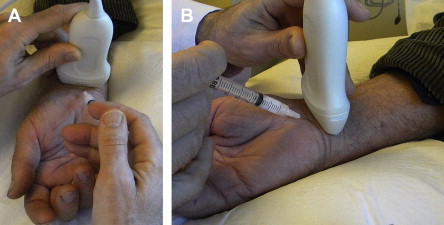
When doing injections via either the short- or long-axis approach, it is important to remember that the needle insertion site is always outside of view of the ultrasound beam, so it is important to briefly scan right over the insertion site to make sure any sensitive structures such as the median nerve, ulnar nerve, or artery are not in the way.
The distance between the skin insertion site and the target is calculated using the ultrasound machine caliper tool or visually estimated based on the scale of the screen; then a 30-gauge, 25-mm needle is inserted just distal and a few millimeters medial to the exact mid-point of the transducer. The needle is directed slightly obliquely such that it passes through the diagonal cleft, ideally with minimal to no contact with the tendons as it approaches the target under the middle of the transducer. The syringe is held lightly in the hand to facilitate sensing the needle slipping between the tendons instead of going into them. When the needle is in place within the superficial row of flexor tendons, 1.5 mL of triamcinolone acetonide, 20 to 40 mg, and normal saline are injected.
After the needle is withdrawn the patient is asked to extend the fingers, thus drawing medication into the carpal tunnel. When combined with the use of a wrist splint at night, the injection typically provides complete relief of symptoms in patients with mild to moderate CTS for 6 months. The advantage of this technique is that it deploys the thinnest possible needle the shortest distance, with minimal to no tendon contact.
Smith and colleagues described a long-axis ulnar approach carpal tunnel injection technique in which a 27-gauge, 38-mm needle is directed from superficial and lateral to the ulnar artery and nerve toward the median nerve. Hydrodissection is used to peel the median nerve away from any adhesions. The long-axis technique ensures that the needle tip and shaft are seen at all times. We have found this technique to be especially useful in cases of failed carpal tunnel surgery when injected into the transverse carpal ligament and the middle of the carpal tunnel, where the nerve and tendons are closely packed. We have also used this approach to inject lidocaine and diagnose the source of pain in cases of flexor tendon impingement arising from a palmar fixation plate and screw ( Fig. 12 ).
Six tendon compartments are present in the dorsal wrist and forearm, laterally to medially, as follows: E1, abductor pollicis longus (APL) and extensor pollicis brevis (EPB); E2, ECRL and ECRB; E3, EPL; E4, EDC; E5, EDM; and E6, ECU. The tendons are prone to friction, overuse, and the development of effusions or tenosynovitis (which would be more accurately described as tenosynovosis).
The tendons are most easily identified by first identifying the Lister tubercle, which is the bony prominence at the dorsal distal radius. The EPL (E3) is located immediately medial to the Lister tubercle or in a groove on top of the Lister tubercle. The tendons that lie immediately lateral to E3 are those of E2 (ECRB and ECRL), whereas those that lie immediately medially are those of E4 (EDC).
de Quervain tenosynovitis involves the E1 tendons, the APL, and EPB, where they cross the radial styloid. Focal tenderness and pain with simultaneous thumb flexion and ulnar deviation of the wrist is present. Ultrasonography findings may include an effusion, tendon enlargement, and hypoechoic thickening of the sheath; sometimes only tenderness to palpation is present ( Fig. 13 ). The APL tendon can have a multilamellar appearance in normal subjects, and this was found to be present in up to 89% of cadaver specimens in one study. A short or long-axis corticosteroid injection can be provided into the tendon sheath or between the tendons.
Intersection or oarsman’s syndrome is a friction syndrome occurring at the intersection of E1 (APL and EPB) and E2 (ECRL and ECRB) in the distal forearm. Ultrasonography findings, if present, include thickening of the tendon sheaths or the presence of fluid between them. Focal tenderness to palpation at this location is specific for the diagnosis. Ultrasonography-guided corticosteroid injection and avoidance of direct pressure and exacerbating activities can help in resolving this problem. A friction syndrome can also occur more distally at the intersection of E2 (ECRL and ECRB) and E3 (EPL).
EDC tenosynovitis is characterized by pain and tenderness over E4. It must be noted that the normal EDC tendons pass under a fairly thick (1–2 mm) retinaculum at the distal wrist. This retinaculum causes acoustic shadowing mimicking the appearance of a fluid collection and tenosynovitis. One must be careful to examine the EDC tendons from several different angles to differentiate between this effect and a true fluid collection.
The fifth compartment, E5, comprises the EDM, which overlies the distal radioulnar joint. Rupture of the EDM may occur in association with rheumatoid arthritis, radioulnar dislocation, or arthrosis and Kienböck disease.
The ECU comprises the sixth compartment, E6, and is a fairly thick, round tendon that can be identified in its groove at the dorsal medial ulna. This tendon’s round form follows its function in resisting forces from multiple angles. The ECU functions as an eccentric wrist stabilizer in racquet sports such as tennis, and is susceptible to overuse and subluxation if its overlying retinaculum is stretched or torn. Dynamic sonography should be performed to look for abnormal volar subluxation and a torn retinaculum ( Fig. 14 ).
The triangular fibrocartilage complex is a homogeneous structure consisting of, but not dissectible into, the ECU tendon sheath, the triangular fibrocartilage (TFC), the meniscus homologue, and the volar and dorsal radiocarpal and ulnar collateral ligaments.
Scanning is best done with the wrist in neutral flexion and maximum radial deviation. The ECU tendon and distal ulna are first visualized in the long axis, following which the transducer is rotated 90° to view the short axis. Scanning continues slowly distally until the hyperechoic cortex of the ulna disappears. At that point, the area seen under the ECU is the TFC ( Fig. 15 ). The meniscus homologue lies slightly more distally and immediately adjacent to the triquetrum.
Ultrasonography findings of a TFC tear include hypoechoic fluid that may contain hyperechoic debris. The detection of TFC tears using ultrasonography remains difficult and insensitive, despite Chiou and colleagues having reported a sensitivity of 68% and specificity of 94% using equipment available in 1998. In their 2008 article, Taljanovic and colleagues were able to achieve an 82% concordance between ultrasonography, arthrography, and magnetic resonance (MR) arthrography for imaging of the TFC in 13 patients. Ultrasonographic visualization of the deep portion of the TFC next to the radius remains a technical problem.
The scapholunate ligament consists of dorsal and volar components, which maintain the relationship between the scaphoid and the lunate during wrist loading and movement ( Fig. 16 ). Acute tears lead to pain and weakness, an increase in distance between the scaphoid and lunate, palmar flexion of the scaphoid, and dorsal flexion of the lunate and proximal migration of the capitate. Chronic tears lead to the scapholunate advanced-collapse wrist with osteoarthrosis of the radioscaphoid and capitate-lunate joints.










