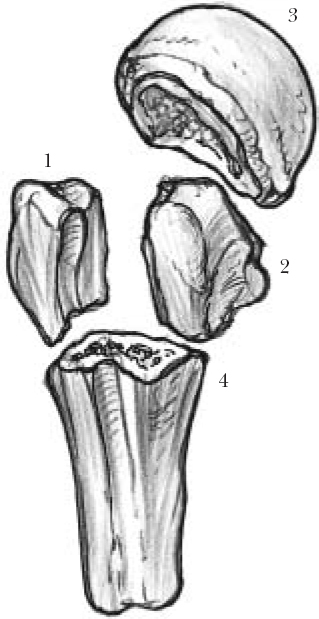
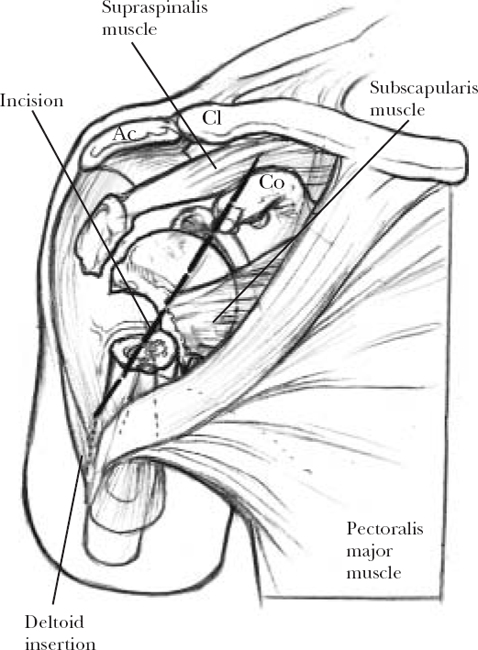
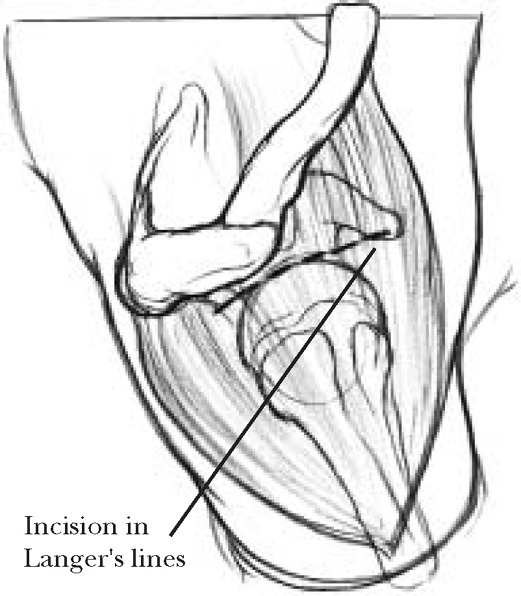
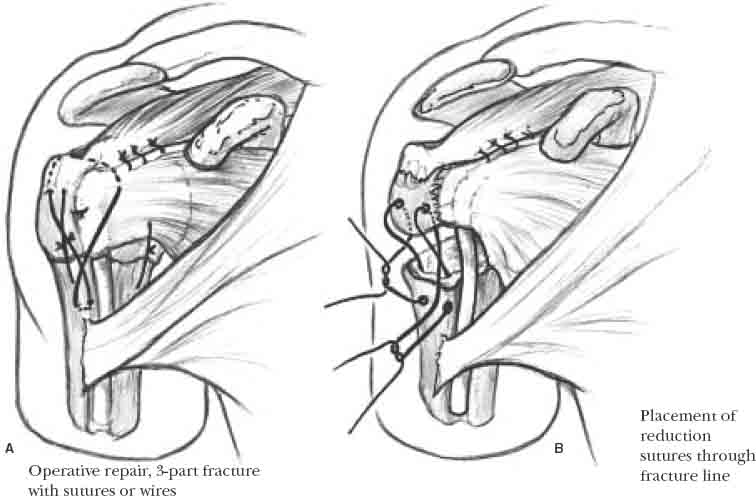
13 With the increasing age of our elder population, the incidence of proximal humerus fractures is increasing. Despite a wealth of literature on the classification and treatment of proximal humerus fractures, a universal treatment protocol has not been well established. Interobserver and intraobserver agreement in the diagnosis and classification of these injuries remains problematic. Regardless of this disagreement, overall good to excellent results support multiple treatment options. Percutaneous reduction and fixation techniques have been developed with the advantages of limited surgical dissection and associated morbidity. New three-dimensional fixation constructs for proximal humerus fractures have been developed that enhance fixation rigidity in difficult comminuted and osteopenic fractures. Although these newer implants are awaiting longer-term clinical follow-up, they provide attractive options for comminuted osteopenic fractures that are not amenable to more traditional fixation. Fractures of the proximal humerus are common and account for 4 to 5% of all fractures.1–3 Court-Brown et al4 prospectively studied the incidence of all classes of proximal humerus fractures over a 5-year period. Proximal humerus fractures occurred predominantly in elderly females; 73% of patients were female, with an average age of 70 years, and the remaining males had an average age of 56 years. The predominant mechanism of injury was a fall from a standing height in 87% of patients. Shoulder fractures that arise from sports injuries and higher energy trauma tended to occur in younger male patients in their third to fifth decades. Patients typically present acutely following a fall from a standing height landing onto the shoulder or the outstretched upper extremity with complaints of pain, swelling, and tenderness in the shoulder. Symptoms of numbness and tingling should be assessed, which suggests an associated neurovascular injury. Hand dominance, occupation, and activity level should be obtained to appreciate the patient’s functional demands and future expectations. The shoulder demonstrates swelling, echymosis, crepitus, and tenderness. The arm is held against the chest wall to avoid painful shoulder motion. A careful neurovascular examination is mandatory to identify any associated neurovascular injuries. The axillary nerve is the most common nerve injured and should be carefully tested with sensation over the deltoid. Deltoid muscle testing is usually compromised secondary to pain. The remainder of the peripheral nerves must also be assessed. Alteration in peripheral pulses suggests injury to the axillary artery, which can occur with fracture-dislocations and can be limb threatening. Echymosis and edema can be significant, and fracture blisters are common in the elderly because of fragile skin. A complete trauma series, including anteroposterior (in the plane of the scapula), lateral (transscapular Y), and axillary radiographs, is required to fully evaluate the proximal humerus. When a standard axillary view cannot be obtained due to pain with abduction of the arm or risk of fracture displacement, a Velpeau axillary view should be obtained in either the upright or supine position. CT is indicated when plain radiographs do not adequately define the displacement, comminution, or articular surface involvement of fracture fragments. MRI is indicated to evaluate associated soft tissues including rotator cuff and labral pathology. Proximal humerus fracture classifications have been developed based on anatomic location, mechanism of injury, displacement of fracture fragments, and vascular supply. Codman5 observed that proximal humerus fractures occur close to the developmental epiphyseal scars and described four main fragments in the proximal humerus (Figure 13-1). Neer’s6–8 four-segment classification considers each Codman fragment a part when the involved fracture fragment has angulation greater than 45 degrees or displacement greater than 1 cm. Fracture fragment displacement results from the rotator cuff and pectoralis major muscle forces. The classification prognosticates viability of the humeral head because blood supply to the head is increasingly compromised with each part fractured. One-part fractures may have one or many fracture lines, but radiographs do not show significant displacement or angulation of fragments. Two-part fractures most commonly involve fracture of the surgical neck with angulation or fracture of the greater tuberosity with displacement. Three-part fractures have a displaced and angulated humeral shaft in addition to one of the tuberosities displaced. Four-part fractures involve displacement of all four fragments. Neer’s classification also subclassifies fracture dislocations and fractures that involve the articular surface of the humeral head. FIGURE 13-1. Codman’s fracture fragments: (1) greater tuberosity, (2) lesser tuberosity, (3) articular surface, and (4) humeral shaft. The original Neer classification has been revised in recognition of the poor outcomes associated with greater tuberosity displacement of more than 0.5 cm.9 Displacement of the greater tuberosity greater than 0.5 cm may lead to significant impingement on the acromion and also decreases the lever arm of the attached rotator cuff muscles, thereby weakening external rotation and elevation. The goals of proximal humerus fracture treatment are to obtain fracture union, preserve function of the shoulder, and avoid complications. Most proximal humerus fractures are minimally displaced and can be treated nonoperatively without hospitalization.4 Early range of motion is essential in optimizing outcome, and Koval et al7,10 recommended that motion exercise be initiated no later than 14 days. Low-demand patients with three-part fractures of the proximal humerus may benefit from nonoperative treatment. In these patients, flexion and abduction greater than 90 degrees is possible and patient satisfaction is high despite nonanatomic reduction.11 Operative treatment is indicated for two-and three-part fractures that do not respond to closed reduction. Surgical neck fractures and three-part greater tuberosity fractures account for the majority of displaced fractures. Factors influencing management include type of fracture, quality of bone and soft tissue, age and reliability of the patient, and patient demands and expectations. Young patients with high demands and expectations have stronger indications to fully restore anatomy to maintain the integrity of the glenohumeral joint articulation. Alternatively, older patients who engage in less strenuous activity with osteopenic bone may not necessitate aggressive attempts at anatomic reduction and fixation. The patient is put in a beach chair position with the bed maximally flexed and the head elevated 60 degrees. The patient’s head is positioned in a well-padded head holder in neutral flexion-extension. The extremity is draped free to facilitate motion of the upper extremity for both reduction of fracture fragments and for visualization under fluoroscopy. Image intensification is most conveniently located at the head of the bed, superolateral to the injured limb. The screen is placed at the patient’s foot. Adequate anteroposterior and axillary views are confirmed prior to draping the patient. The deltopectoral approach (Figure 13-2) may be used for two-part surgical neck, two-part lesser tuberosity, and three-and four-part fractures. A linear skin incision is made from just lateral to the coracoid to the deltoid insertion. The cephalic vein is identified and marks the internervous interval between the deltoid and the pectoralis major muscles. The cephalic vein is retracted laterally with the deltoid. The clavipectoral fascia is incised to expose the subscapularis muscle. Proximally, the tip of the coracoid and the origin of the strap muscles are identified. The short head of the biceps brachii and the coracobrachialis muscles are retracted medially, minimizing the risk of injury to the musculocutaneous nerve and the remainder of the brachial plexus. The subacromial bursa and lateral subdeltoid bursa are freed, and the coracoacromial (CA) ligament is identified. A partial excision of the CA ligament helps superior exposure. A 1 cm release of the superior aspect of the tendinous pectoralis major insertion may be performed to improve exposure of the proximal humerus. A cuff of tissue is left at the insertion that is repaired following fracture fixation. The biceps tendon is identified and helps to orient anatomy that may be distorted from fracture displacement. The biceps tendon is followed superiorly and becomes intra-articular at the rotator interval, between the subscapularis and the supraspinatus. Opening this interval will facilitate exposure of the joint and fracture fragments. Zero or number 2 nonabsorbable braided sutures are placed in the tendinous rotator cuff insertions at the greater and lesser tuberosities to mobilize the fragments as needed. FIGURE 13-2. Deltopectoral approach demonstrating skin incision. AC: acromion; CL: clavicle; CO: coracoid. Two-part surgical neck fractures that require Ender’s rods, isolated greater tuberosity fractures, and three-part fractures that attain adequate closed reduction and impaction of the surgical neck fracture are good candidates for fixation through this approach (Figure 13-3). The superior approach is a muscle splitting-approach through the proximal deltoid. There is no internervous plane. The landmark for incision is the lateral border of the acromion. A 6 cm incision is made parallel to the acromial border approximately 2 cm lateral to the palpable bony margin in Langer’s lines. The deltoid is split in line with its fibers from the edge of the acromion to a point 4 cm distal in a natural raphe between the anterior third and posterior two thirds of the muscle belly. The axillary nerve courses from posterior to anterior within the deltoid approximately 3 to 5 cm lateral to the acromial border. A stay suture tied at the distal extent of the deltoid split prevents propagation of the muscle split that could injure the axillary nerve branches.12 Elevation of the deltoid origin anteriorly off the acromion may improve visualization; however, this is discouraged to minimize the risk of deltoid dehiscence. The inflamed subdeltoid bursa is excised, and the subacromial adhesions are lysed. Internal and external rotation of the arm and longitudinal traction facilitate visualization of the cuff insertions and displaced fragments. FIGURE 13-3. Superior deltoid-splitting approach demonstrating skin incision in Langer’s lines. Two-part greater tuberosity fractures commonly occur in combination with anterior glenohumeral dislocations in relatively younger patients with stronger rotator cuff insertions. The avulsed greater tuberosity is retracted superiorly and posteriorly by the supraspinatus, infraspinatus, and teres minor muscles. Superior displacement of the greater tuberosity can result in subacromial impingement with overhead elevation. Less than 5 mm of displacement may be treated with a short period of immobilization followed by guided rehabilitation. However, the magnitude of acceptable displacement is controversial. A recent study suggested as little as 3 mm of displacement may be unacceptable in an athletic individual.13 For most patients, greater than 5 mm of displacement indicates operative treatment.9 Isolated greater tuberosity fractures are best accessed with a superior deltoid-splitting approach.14 The tuberosity and its tendinous cuff insertions must be mobilized for reduction, which often requires releasing adherent sub-acromial bursal adhesions. Sutures passed through the rotator cuff at its insertion allow control and mobilization of the tuberosity fragment to its fracture bed. Two or three heavy number 5 nonabsorbable braided sutures are placed in the rotator cuff tendon that inserts onto the greater tuberosity fragment (Figure 13-4A). The insertions of the supraspinatus, infraspinatus, and teres minor usually provide stronger fixation than the osteopenic bone of the tuberosity fragment. Drill holes are placed 1 cm distal to the fracture bed in the shaft for transosseous sutures. Over-reduction of the greater tuberosity is prevented if one arm of the suture is passed through the fracture site. The suture is passed through the shaft drill holes and tied sequentially (Figure 13-4B). Once the reduction is confirmed with fluoroscopy, additional suture fixation is achieved with simple or figure-eight passing that incorporates the rotator cuff. The arm is gently moved through an arc of motion to confirm the stability of fixation. Any longitudinal tears in the rotator cuff should be repaired with interrupted number 0 nonabsorbable braided suture. The rotator interval is closed in a similar fashion. This will remove tension from the fracture repair by dispersing load across the rotator cuff expansion. Flatow et al14 studied the outcome of 12 patients treated with open reduction and fixation with heavy non-absorbable sutures through a superior deltoid-splitting approach and attained 100% good or excellent results. When the greater tuberosity fragment is sufficient size, screw fixation augmented with tension band wire has also been shown to yield excellent results in 80% of patients.15 Screw fixation alone may also be considered when comminution is minimal and the bone quality is good (Figure 13-5). Reduction may be achieved either with the open approach or percutaneously, with small bone hooks with fluoroscopy or arthroscopy confirming the reduction. Arthroscopy has additional advantages of visualizing accurate reduction and allowing assessment of the rotator cuff and intra-articular pathology. Jones16 have described a high percentage of patients with associated rotator cuff tear, rotator interval tear, and/or capsulolabral tear that can be treated simultaneously. FIGURE 13-4. (A). Greater tuberosity fracture treated with open reduction and suture fixation. (B). Sutures passed through the fracture to prevent over-reduction. Two-part lesser tuberosity fractures are uncommon, and the diagnosis is often missed. This fracture pattern may occur in combination with a posterior glenohumeral dislocation, and adequate imaging is required to ensure the glenohumeral joint is reduced. Often CT scanning is required to determine displacement and the extent of humeral head articular involvement that may be attached to the lesser tuberosity.17 Large series of two-part lesser tuberosity fractures are absent in the orthopedic literature, and recommended treatment is inconsistent among reports.17–21 Isolated lesser tuberosity fragments displace medially under sub-scapularis tension, and a deltopectoral approach is best. Using the same principles outlined for greater tuberosity fragments, the lesser tuberosity fragment is reduced and is most commonly fixed with suture. Heavy number 5 sutures are placed in the tendinous rotator cuff insertion at the lesser tuberosity fragment. Transosseous tunnels with a 1 cm cortical bridge are drilled in the intact humerus. The fracture is reduced, and the suture repair is completed with rotator interval closure and repair of rotator cuff rents. If the fragment is of sufficient size and the patient’s bone quality is strong, screw fixation, with or without supplemental suture fixation, may be considered. The fracture bed is debrided and prepared for fixation. Biceps tenodesis may be required if the tendon is attenuated, degenerated, or subluxing. Two-part surgical neck fractures are the most common type of proximal humerus fracture. Fracture deformity results from the pull of the pectoralis major on the humeral shaft anteriorly and medially. Three fracture patterns are observed based on displacement of the shaft: impacted, unimpacted, and comminuted.8 Unimpacted fractures have an anteriorly and medially displaced shaft. Comminuted fractures of the surgical neck are grossly unstable. Most impacted proximal humerus fractures are minimally displaced and can be treated in a sling with early mobilization. Nonoperative treatment results have been improved with early range of motion initiated within 14 days of injury.10 Nonimpacted and unstable displaced fractures require operative treatment. Operative techniques include closed reduction and percutaneous pinning (Figure 13-6), open reduction with suture fixation with or without Ender’s rods (Figure 13-7), and open reduction and fixation with either a blade plate or a locking plate (Figure 13-8). The details of surgical techniques for fixation of the surgical neck are described in the section on three-part fractures.
Two- and Three-Part Fractures of the Proximal Humerus
Incidence and Mechanism of Injury
Assessment
History
Physical Examination
Imaging
Classification
Treatment
Surgical Approaches
Deltopectoral Approach
Superior Deltoid Split Approach
Surgical Technique
Two-Part Greater Tuberosity Factures
Two-Part Lesser Tuberosity Fractures
Two-Part Surgical Neck

Two- and Three-Part Fractures of the Proximal Humerus
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








