Trochanteric Osteotomy
Brian J. McGrory
Key Points
• Contemporary uses include difficult exposure and soft tissue tensioning.
• Obtain stable, reliable fixation.
• Avoid full weight bearing and active abduction until healing is achieved.
Introduction
Leopold Ollier initially described trochanteric osteotomy (TO) as part of the lateral approach to the hip for surgeries such as joint excision and hip arthrodesis,1 and Charnley popularized TO for total hip arthroplasty (THA) exposure.2,3 Because first-generation implants were monolithic and were available only in limited sizes, trochanteric advancement was a usual part of the standard procedure.
Once a commonplace surgical technique for primary and revision THA, TO has become a tool that is rarely needed. The trochanteric flip osteotomy and the extended trochanteric osteotomy are used much more regularly today (for specific purposes), but each is the subject of its own chapter. Specific advantages of TO include exposure and soft tissue tensioning. The decision to proceed with osteotomy must balance the need for these benefits with associated increased surgical time, postoperative limitations, and risk of complications.
An orthopedic surgeon should be able to perform a TO and reliably repair it. A plethora of specific osteotomy techniques and fixation methods are described in the literature, but no one method has been conclusively shown to be advantageous. This chapter will review indications and contraindications and preoperative planning and will highlight major osteotomy variations and fixation techniques; postoperative care and recognition and treatment of TO complications will also be discussed.
Indications/Contraindications
Contemporary THA accentuates a streamlined approach to surgery and recovery while maximizing long-term success. Present-day exposure techniques and modular implants make the routine use of osteotomy obsolete. In 1984, Hamblin4 estimated that 10% to 20% of hips require TO for restoration of normal joint anatomy, but this estimate is likely high by today’s standards. Rates of TO reflect geographic trends and surgeon preferences. In my single-surgeon practice, the incidence of trochanteric osteotomy in primary hip replacement is only 0.3% (5/1720) over the past 10 years. The incidence during the same time period is higher for conversion to THA (1.2%, 2/172) and is even higher for revision THA (2.1%, 9/420, excluding extended trochanteric osteotomy). Current indications for trochanteric osteotomy are limited to cases of difficult surgical exposure and soft tissue tensioning.
In the infrequent THA that requires enhanced exposure, osteotomy may be extremely useful. Examples include cases in which a very complex acetabular reconstruction is performed, as in severe developmental dysplasia of the hip (DDH), pelvic discontinuity, and tumor removal. Ankylosis linked to take-down of a prior fusion or marked rigidity due to heterotopic ossification may also require TO. Severe protrusio acetabuli is sometimes associated with inability to dislocate the hip; osteotomy may be a useful tool in these cases. Striking femoral malformations found in some cases of DDH, Paget’s disease, and post-traumatic or postsurgical abnormalities may also lend themselves to TO.
Many of these deformities require appropriate soft tissue balancing, as well as exposure. In a situation with a marked hip varus deformity or one in which it is necessary to correct unacceptable laxity of the abductors for any reason, osteotomy and trochanteric advancement may be quite useful. Although contemporary implants allow the ability to modify soft tissue balance, trochanteric advancement is sometimes necessary in cases of leg length inequality (Fig. 20-1A and B) or of revision surgery with a nonmodular femoral component. It is also useful in cases of osteotomy in which the femur is shortened or the hip is unstable because of a high hip center.
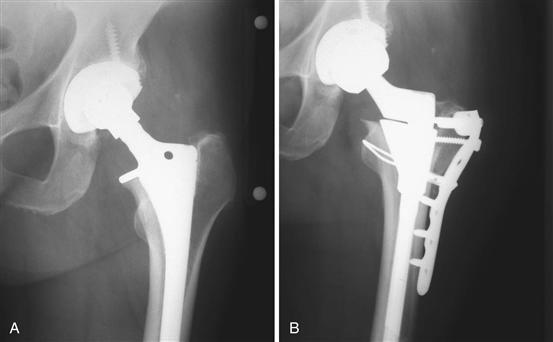
Figure 20-1 Anteroposterior radiographs of a hip replacement with unacceptable leg lengthening (A) before and (B) after revision surgery with trochanteric osteotomy and advancement. Internal fixation using a locking plate with cable augmentation.
Osteotomy is not indicated today in most cases of THA because adequate exposure and tensioning of the hip can be reliably achieved without associated increased risks, increased surgical time, and postoperative restrictions of this procedure. Even when TO appears indicated, osteotomy is contraindicated in some circumstances. Alternative methods of exposure, such as myofascial flap,5 should be strongly considered in cases of pathologic bone (e.g., fibrous dysplasia of the proximal femur). In revision surgery with severe trochanteric osteolysis, extending the trochanteric osteotomy to an area of thicker and more viable bone (distally) should be considered. Another option in this scenario is the bulk allograft and locking plate technique introduced for trochanteric fracture through osteolytic bone.6 In cases of ankylosis with abductor scarring, the surgeon should be prepared to release the abductors (the so-called abductor slide technique7). Surgeries that leave a large proximal prosthesis or bone cement in the greater trochanteric bed are likely to lead to nonunion and are relative contraindications to TO. If exposure is not attainable by other means, the potential consequences of a nonunited trochanter must be accepted or trochanteric osteoplasty considered.8
Preoperative Planning
The one factor that a surgeon has greatest control over in attaining an excellent outcome is a well-executed surgical strategy. In hip replacement surgery, this is best achieved through preoperative planning. A trochanteric osteotomy (and subsequent fixation) must be part of that plan in some circumstances.
If an osteotomy is anticipated, the optimal type and fixation method are chosen to maximize healing, minimize postoperative restriction, and allow an efficient surgery. These plans should be included in the consent process discussion with the patient. Preoperative radiographs should be used to anticipate the precise location of the osteotomy and whether advancement is needed. Any special tools or implants can then be made available.
Osteotomy Techniques
TO techniques can be generally divided into standard, slide, and repeat osteotomy groups. Multiple variations of the standard and slide categories have been developed; these will be highlighted.
Standard
The standard TO was originally popularized for use in hip arthroplasty by Charnley,2,9 and later was optimized by many surgeons, including Harris.10,11 After exposure of the hip, a Cushing elevator is inserted from anterior to posterior in the interval between the tendon of the gluteus minimus and the superior part of the hip capsule. Next, the origin of the vastus lateralis is elevated from the vastus tubercle. The osteotomy cut traverses the sulcus between the lateral portion of the origin of the vastus intermedius muscle and the insertions of the gluteus medius and minimus. The osteotomy is started 1 cm distal to the vastus tubercle and is performed with an oscillating saw or osteotome, which is aimed at the Cushing elevator (Fig. 20-2). Once the trochanter has been cut, it is retracted proximally, and the short external rotators are released from the trochanteric fragment. This enhances mobilization of the trochanter proximally. Healing rates of the standard osteotomy vary, but in one large study of 804 cases (725 primary and 79 revision), 8 osteotomies (1%) did not heal. Delayed union of the osteotomized trochanter (defined as that occurring more than 6 months after the procedure) was noted in 17 (2.3%) primary cases and 6 (7.6%) revision cases.10
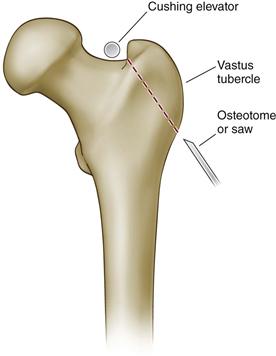
Figure 20-2 Standard trochanteric osteotomy. (Redrawn from McGrory BJ, Bal BS, Harris WH: Trochanteric osteotomy for total hip arthroplasty: six variations and indications for their use. J Am Acad Orthop Surg 4:258, 1996.)
Modifications of the Standard Osteotomy
Chevron.
Bi-plane, dihedral, or chevron osteotomy (CO) was first described by Debeyre and Duliveux12 and was later popularized by Weber and Stuhmer.13 This technique is said to allow immediate rotatory stability and at the same time permits near-anatomic replacement of the trochanteric fragment. It is not indicated in cases of trochanteric advancement. Weber compared two groups of 69 patients with standard and chevron osteotomies and noted a nonunion prevalence of 11% in the standard group and 1.5% in the chevron group.14 Berry and Muller reported trochanteric union rates of 98% for primary surgery (53 hips) and 97% for revision surgery (74 hips) with this technique.15 These results were confirmed by Wroblewski and Shelley in a larger group of 222 primary and revision surgeries.16
Several technical variations are available for the CO. Similar to the flat standard osteotomy, the CO starts 1 cm distal to the vastus tubercle. The anterior and posterior limbs are equal in size and the thickness of the apex adequate to avoid fracture. The limbs are angled approximately 30 degrees from the apex; the trochanteric cancellous surface is concave and the femur surface convex (the “chevron” is in the sagittal plane). Cuts can be made with a narrow oscillating saw, a straight or chevron-shaped17 osteotome, or a Gigli saw. The Gigli saw method, as presented by Wroblewski and Shelley,16 starts by passing a 4-mm smooth Steinmann pin into the center of the trochanter, directing it 45 degrees to the shaft of the femur. The saw is then passed craniad to the femoral neck at the junction of the greater trochanter with the superior part of the femoral neck. The saw lies proximal to the pin and is directed distally, cutting anteriorly and posteriorly, creating a CO (Fig. 20-3).
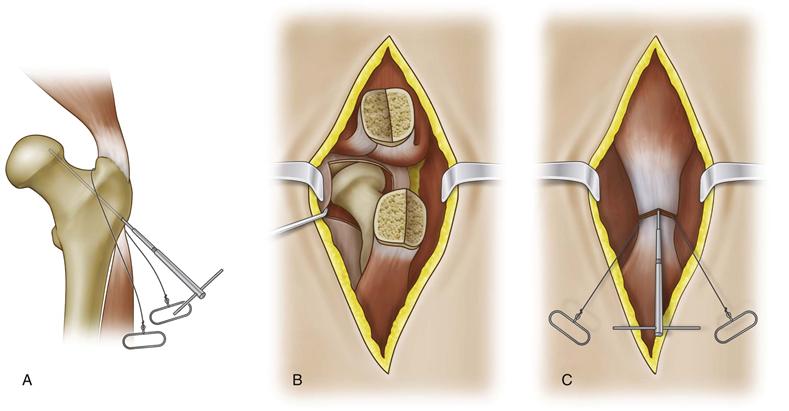
Figure 20-3 Chevron osteotomy. This specific technique was described by Wroblewski and Shelly.16 (Redrawn from Wroblewski BM, Shelley P: Reattachment of the greater trochanter after total hip replacement. J Bone Joint Surg Br 67:736, 1985.)
Oblique
McGrory, Bal, and Harris described a partial osteotomy that was devised to increase the somewhat limited exposure that is sometimes attained with a direct lateral approach for primary total hip replacement while minimizing the risk of posterior dislocation.11 The anterior portion of the osteotomy begins over the palpable sharp ridge that is the limiting structure of the anterior aspect of the insertion of the abductors. The anterior portion of the osteotomy is similar to, but slightly craniad to, that used for a standard TO. The posterior bone cut remains superficial to the intertrochanteric ridge and the insertion of the short external rotators (which are left attached to the femur). Thus the fragment is wider anteriorly than posteriorly but contains all of the insertion of the gluteus medius and gluteus minimus. The trochanter is reflected proximally, and an anterior capsulotomy is performed. The hip is dislocated anteriorly. In 26 consecutive cases, the authors reported a nonunion rate of 4% (1/26) using this approach, with no postoperative instability.11
Posterior
Several authors have reported variations of a technique credited to Iyer18 for THA with modification of a limited posterior trochanteric osteotomy. The osteotomized bone fragment includes the posterior insertions of the short external rotators and the posterior capsule. Similar to the oblique osteotomy, this variation was designed to enhance postoperative stability. Sanchez-Sotelo and associates reported that radiographic union was achieved in 94% (64/66) of primary hip replacements, with two cases of postoperative instability.19 Stuchin and Millman,20 after adapting this technique for revision surgery and using heavy, nonabsorbable sutures for fixation, reported their results of 47 revision procedures in 35 patients. No dislocations or significant complications were reported, and no loss of reduction or nonunion occurred at the osteotomy site.
Trochanteric Slide
The anterior trochanteric slide technique, or the sliding trochanteric osteotomy, is a widely used alternative to the standard trochanteric osteotomy.21–24 The idea of keeping the tendinous portions of the gluteus medius and vastus lateralis intact during posterior exposure of the hip was first described by McFarland and Osbourne,25 although it was Mercati and colleagues26 and English22 who described this concept in conjunction with an osteotomy. The goal was to convert the tensile forces placed across the detached bony fragment to compressive forces that would counteract the pull of the abductors in the coronal plane. These changes are thought not only to prevent migration but also to encourage rapid union. Other advantages include preservation of some abductor function, even if union fails, and possible increased blood supply to the trochanteric fragment.27 Glassman described this approach in detail in 1987 and popularized its use in revision surgery.21
The skin incision with this osteotomy diverges anteriorly from the course usually taken with a posterior approach. It parallels the anterior border of the greater trochanter before continuing posteriorly, along with the fibers of the gluteus maximus. The gluteus medius muscle is isolated anteriorly and posteriorly, and the fascia overlying the vastus lateralis is incised for 10 to 15 cm distal to the vastus ridge and 1 cm anterior to the intermuscular septum. The vastus lateralis is then elevated subperiosteally from the femoral shaft and is retracted anteriorly.
The osteotomy cut, usually performed with an oscillating saw, is oriented in the sagittal plane and begins just medial to the tendinous insertions of the gluteus medius into the greater trochanter. The osteotomy exits distal to the vastus ridge, so that the origin of the lateralis is preserved in continuity with the bony wafer. The osteotomy fragment is somewhat thinner than for a standard trochanteric osteotomy (Fig. 20-4).
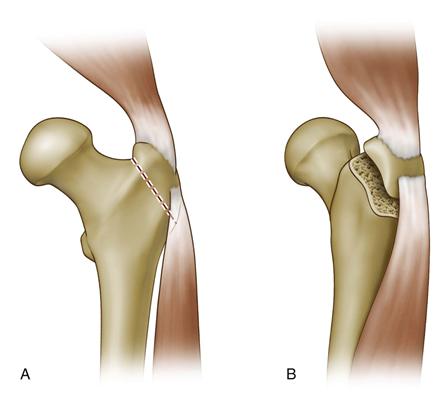
Figure 20-4 Anterior trochanteric slide osteotomy. (Redrawn from Harris WH: Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. J Bone Joint Surg Am 51:737, 1969.)
Once the trochanter has been osteotomized, it is retracted with its muscular sleeve craniad and commonly is held with a self-retaining retractor. The external rotators and the gluteus minimus are then divided close to their insertion and are preserved for reattachment after reapproximation of the trochanter. Dislocation is usually accomplished with the hip in adduction and external rotation, and the leg is placed anteriorly in a sterile bag. Alternatively, the hip can be dislocated posteriorly, but in this case, a posterior incision is needed.
Glassman and colleagues reported on slide osteotomy for 90 THAs, of which 88 were revision cases. Nine osteotomies (10%) resulted in nonunion, and seven of the nine had proximal migration of the osteotomy fragment. No cases of instability were reported; however, 23 hips (28%) were noted to have an abductor lurch.21
Modifications of the Trochanteric Slide
Maintaining Posterior Attachments.
Goodman and co-workers28 modified the slide technique to preserve the posterior capsule and the external rotators on the proximal femur, with translation of the osteotomized fragment anteriorly. This change imparts increased resistance to posterior hip dislocation. In their report, 14.8% (4/27) of the acetabular revisions performed using a traditional trochanteric slide dislocated and required a closed reduction within 1 year of surgery. With maintenance of the posterior attachments, only 3.3% (1/30) dislocated. This difference was found to be statistically significant. When this technique was used for complex hip arthroplasty in 83 surgeries followed for up to 126 months, 77 (84.4%) healed with bony union, 9 (10.8%) had fibrous union, and 4 (4.8%) had nonunion. Six patients (7.2%) developed a new abductor lurch, and 4 (4.8%) postoperative dislocations occurred.29
Triplanar Slide.
Ackerman and Trousdale recently reported a modification of the trochanteric slide osteotomy, which they call a triplanar trochanteric osteotomy.30 This variation not only preserves the posterior structures, it also adds further stability through a triplanar or chevron geometric contour. The “chevron” in this case, however, is in the coronal plane (Fig. 20-5).
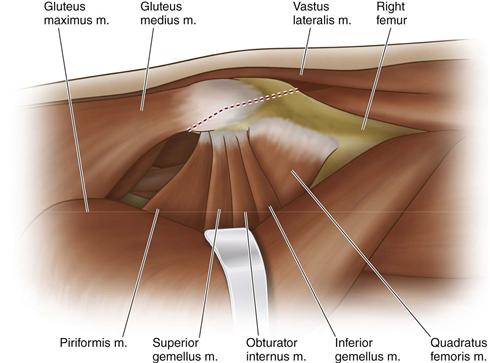
Figure 20-5 Chevron modification of the trochanteric slide osteotomy as described by Ackerman and Trousdale.30 (Redrawn from Ackerman DB, Trousdale RT: Triplanar trochanteric osteotomy: a modified anterior trochanteric slide osteotomy. J Arthroplasty 23:459, 2008.)
After exposure of the trochanter, the interval between the gluteus medius and the gluteus minimus is developed, and the medius is retracted anteriorly. The minimus, short external rotators, and piriformis remain posterior to the retractor. A point is then identified along the posterior border of the greater trochanter, approximately equidistant from the tip of the trochanter and the vastus ridge. The thickness is estimated, and a goal of 2 cm is marked with electrocautery (outlining the apex of the chevron-shaped osteotomy). With care taken to leave the vastus lateralis in continuity distally, the osteotomy is carried 90% to 95% of the way and then is levered and fractured anteriorly (leaving an anterior vertical ridge). This ridge resists anteriorly directed forces after reduction, allowing for anatomic reduction.
Step.
Schoeniger and associates have proposed another modification of the slide osteotomy that consists of similar soft tissue attachments but with a unique bony contour, again to add stability during bony reattachment.31 The superior cut of the step osteotomy is performed similarly to the traditional slide, but a diagonal step is added. The step is inclined 20 to 30 degrees inferiorly on the anterior side, with a 5-mm step depth. This osteotomy has been shown by in vitro testing to be a more stable construct than the commonly performed slide osteotomy.
Anterior Trochanter Only.
Dall32 is credited with a technique of slide osteotomy that is based on the transgluteal approach of Hardinge.33 The gluteus minimus is split for 2 cm proximal to the tip of the greater trochanter, and the vastus lateralis is split distally in line with its muscle fibers. A Gigli saw is then passed superficial to the capsule anteriorly, but deep to the anterior one half of the gluteus medius and gluteus minimus. A partial (anterior) osteotomy is then performed with the hip adducted, slightly flexed, and internally rotated. The saw is directed as far posteriorly as possible to avoid making the osteotomy fragment too small. The triangular bone fragment that is created carries the anterior one half of the gluteus medius, gluteus minimus, and anterior vastus lateralis. The hip is dislocated anteriorly by this approach.
Split Trochanter (Stracathro).
McLaughlin has described the Stracathro Hospital technique, which splits the trochanter into anterior and posterior fragments.34 Two wafers of trochanter are created by first dividing the gluteus medius and vastus lateralis. The short external rotators remain attached to the posterior fragment. After hip implantation, the trochanteric fragments fall back into place and are anchored with sutures to the soft tissues. This type of osteotomy may not be advisable for revision surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








