70
Triscaphe Degenerative Arthritis
Andrew E. Caputo and H. Kirk Watson
History and Clinical Presentation
A 62-year-old right hand dominant woman who works as a polisher presented with right wrist pain progressively worsening over the last 6 months. She noted significant and progressive difficulty with strength and holding onto small objects. She denied any trauma and noted no specific previous treatment.
Physical Examination
The patient had specific localized tenderness and swelling of the scaphoid-trapezium-trapezoid (STT/triscaphe) joint. This area is located by following the index metacarpal proximally until a recess is palpated. This recess is the dorsal aspect of the triscaphe joint. Passive wrist flexion extension and radial/ulnar deviation were limited with tender end points. Passive forearm rotation was nontender. No other areas of tenderness or swelling were noted. This finding is similar to what is found in most patients with triscaphe degenerative arthritis.
Diagnostic Studies
Posteroanterior and lateral views of the right wrist revealed isolated loss of joint space and subchondral sclerosis of the triscaphe joint (Fig. 70–1). No other radiologic signs of degenerative joint disease were noted in the other areas of the hand or wrist.
PEARLS
- Avoid driving the K wires into the radioscaphoid joint. The surgeon should be able to feel the purchase of the K wires into the subchondral bone of the proximal pole of the scaphoid. Intraoperative fluoroscopy can be utilized to facilitate proper placement.
PITFALLS
- Avoid overcorrecting the scaphoid. As noted above, scaphoid position is critical. The surgeon should be holding the scaphoid position as described while an assistant drives the K wires.
Differential Diagnosis
Carpometacarpal arthritis
Nonpantrapezial
Pantrapezial
Radiocarpal arthritis
Scaphocapitate arthritis
Scaphotrapezial trapezoid arthritis

Figure 70–1 Localized degenerative arthritis to the scaphoid-trapezium-trapezoid (STT)/triscaphe joint is noted with sclerosis and complete loss of cartilage space.
Diagnosis
Triscaphe Degenerative Arthritis (Scaphotrapezial, trapezoid)
Triscaphe degenerative arthritis is the second most common type of degenerative arthritis in the wrist. The most common is the pattern of destruction associated with a scapholunate advanced collapse (SLAC) wrist. The diagnosis is relatively easy when radiographs confirm the isolated joint destruction to the STT joint.
Triscaphe arthrodesis has been successful in the management of patients with this process. Postoperative pain relief and stability are consistently excellent. Wrist range of motion after 4 to 6 weeks of hand therapy (2 to 3 months postoperatively) is usually 50–70% of the contralateral side. At 1 year postoperatively, wrist motion often reaches 80% and grip strength 90% of the contralateral side. Long-term follow-up (up to 27 years) has demonstrated only rare radioscaphoid or other intercarpal degenerative change.
Surgical Management
Position
In the supine position, the affected extremity is prepped free on a hand table. A brachial tourniquet is utilized after esmarch exsanguination.
Approach
The triscaphe joint is approached through a dorsal transverse incision just distal to the level of the radial styloid. A spreading technique is utilized to mobilize and protect dorsal veins and branches of the superficial branch of the radial nerve. Although not done in this case, we now routinely excise the distal 5 mm of the radial styloid with a rongeur, sloping volarly from distal to proximal. A transverse incision is made in the capsule, and the radioscaphoid joint is inspected. If the radioscaphoid joint has significant degenerative arthritis, then a SLAC reconstruction is performed. The distal aspect of the extensor retinaculum is incised in line with the extensor pollicis longus, which exposes the triscaphe joint. The capsule over the triscaphe joint is incised transversely, between the tendons of the extensor carpi radialis longus and brevis.
Resection
The entire articular surface of the scaphoid trapezoid and the scaphoid trapezium joints are removed with a rongeur. The dorsal nonarticular surface of the trapezium-trapezoid are cut back to cancellous bone. Only the proximal half of the trapezium-trapezoid joint is resected. The volar lip of the distal pole of the scaphoid is denuded. Levering the handle of the dental rongeur distally facilitates this resection.
Bone Graft Harvest
The distal radius metaphysis is routinely utilized for the bone graft donor site. The distal radius is approached through a transverse incision 3 cm proximal to the radial styloid. The incision is centered between Lister’s tubercle dorsally and the first compartment radially. The spreading technique is utilized to mobilize and protect veins and the superficial branches of the radial nerve. The flat periosteal surface between the first and second extensor compartments is exposed and confirmed by the presence of the constant longitudinally oriented periosteal artery. The periosteum is incised longitudinally in line with this artery and subperiosteally elevated. Ateardrop-shaped cortical window (∼2 cm long × 1.5 cm wide) is created with an osteotome, and cancellous bone is removed with an 8-mm curette. The cortical window is replaced and secured in position by overlying periosteum and extensor tendon compartments.
Fusion
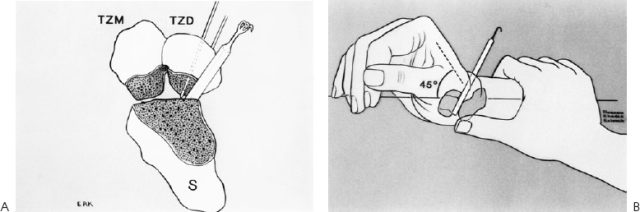
Two 0.045-inch Kirschner wires (K wires) are preset into the trapezoid percutaneously (Fig. 70–2A). The radial K wire is positioned to just touch the surface of the scaphoid, and the ulnar K wire is held back in the trapezoid. The wrist is then placed in full radial deviation and 45 degrees of extension. Concomitantly, the scaphoid is reduced by the surgeon’s thumb to prevent overcorrection (Fig. 70–2B). It is critical to maintain the original external dimensions of the triscaphe joint. To facilitate this, a 5-mm spacer (i.e., the handle of a small hook) is placed into the scaphotrapezoid space and the radial K wire is driven into the proximal pole scaphoid. The spacer is removed and the ulnar K wire is driven into the scaphoid. Viewed laterally, the optimal position for the scaphoid is 55 to 60 degrees of flexion relative to the longitudinal axis of the radius. This angle in a normal wrist is ∼47 degrees.
The cancellous bone is then densely packed into the triscaphe joint space with a dental amalgam tamp. With the external dimensions of the triscaphe joint maintained, this often translates to a 4- to 8-mm gap prior to grafting.