Treatment of Slipped Capital Femoral Epiphysis Deformities in Skeletally Mature Patients
Nathaniel J. Nelms
Rafael J. Sierra
Introduction
Slipped capital femoral epiphysis (SCFE) typically occurs in patients between the ages of 10 and 16. The capital epiphysis displaces posteriorly and inferiorly with respect to the femoral metaphysis and results in a varus, extension and external rotation deformity of the femur. The majority of patients are treated with semiurgent pinning in situ under fluoroscopic imaging without attempts at reduction because of the risk of osteonecrosis associated with manipulative reduction. Although in situ pinning stabilizes the hip and leads to closure of the physis, there is concern over the consequences of leaving the physis in a nonanatomic position.
The deformity caused by SCFE causes limitation in hip range of motion and leg-length discrepancy related to the degree of deformity. With hip motion, this deformity may lead to early joint damage and eventual osteoarthritis. Joint damage may occur via femoroacetabular impingement (FAI) and possibly by altered hip joint orientation. In addition, chondrolysis and osteonecrosis of the hip with subsequent degenerative joint disease remain a problem even with in situ hip stabilization. Historically manipulative treatment of SCFE deformity has led to unacceptably high rates of femoral head osteonecrosis causing acceptance of limitations imposed by the deformity.
The Structural Deformity
The deformity results from an apparent posterior and varus rotation of the femoral head relative to the neck. Abraham et al. (1) detailed the anatomic changes seen in hips undergoing arthroplasty for degenerative disease with prior SCFE. Hips with SCFE deformity which develop osteoarthritis are characterized by the following: (1) loss of head/neck offset; (2) acetabular neck impingement; and (3) loss of superior peripheral articular cartilage adjacent to the superior neck. This is distinct from hips with primary osteoarthritis where there is usually preservation of the head–neck offset, absence of acetabular neck impingement, and preservation of the superior peripheral articular cartilage. Also as a result of the deformity, thinner superior femoral head cartilage is exposed to higher joint reactive forces which are more typically experienced by areas of thicker cartilage.
The structural deformity associated with SCFE results in decreased hip range of motion. Mamisch et al. (2) simulated range of motion using CT data from patients with SCFE. These authors demonstrated that the femoral metaphyseal morphology and degree of slip determine the severity of motion restriction. Even hips with mild slip angles can have limited range of motion if a decreased head–neck offset is present. In moderate slips, flexion, adduction, and internal rotation are limited because of an inevitable loss of femoral head–neck offset (Fig. 50.1).
Several authors have observed some remodeling of the deformity (3,4,5,6,7). The observed remodeling is accompanied by variable improvement in hip motion. This may be associated with decreasing synovitis and resorption of bone on the anterior metaphysis with the deposition of bone posteriorly. Most remodeling appears to occur in the first 6 to 12 months. Remodeling may improve the head–neck offset by smoothing the anterior metaphyseal prominence; however, the spatial relationship of the head to the neck does not normalize. In addition, remodeling can theoretically convert a slip where there is “impaction” impingement of the prominent metaphysis against the acetabulum to “inclusion” impingement where the rounded but still prominent metaphysis enters the joint causing damage, a deformity that could lead to sheer damage of the articular cartilage (8,9) Fraitzl et al. (10) reported on 16 patients with unilateral mild SCFE who were treated with in situ pinning. In this group of patients followed for an average of 14.4 years (11.3 to 21.2), an anterior impingement sign on clinical examination was present in 37%, which was not significantly different from the rate in the contralateral prophylactically pinned hips. So even after prophylactic pinning of an asymptomatic contralateral hip, structural abnormalities of that hip can still lead to impingement. Structural
abnormalities in unslipped hips with contralateral SCFEs have been described to include decreased femoral anteversion and acetabular overcoverage or retroversion (11,12). In this group of hips, radiographic evaluation demonstrated that none of the hips with mild SCFE had normal head–neck ratios or alpha angles (10). Mean hip internal rotation was significantly decreased compared to the contralateral hips. Despite the relative lack of clinical symptoms in this small group of patients with mild slips, there were marked morphologic changes of the proximal femur which could predispose them to impingement-related joint damage in the future.
abnormalities in unslipped hips with contralateral SCFEs have been described to include decreased femoral anteversion and acetabular overcoverage or retroversion (11,12). In this group of hips, radiographic evaluation demonstrated that none of the hips with mild SCFE had normal head–neck ratios or alpha angles (10). Mean hip internal rotation was significantly decreased compared to the contralateral hips. Despite the relative lack of clinical symptoms in this small group of patients with mild slips, there were marked morphologic changes of the proximal femur which could predispose them to impingement-related joint damage in the future.
FAI and HIP Damage
Leunig et al. (8) described the intraoperative findings in 13 consecutive adolescents (14 hips) undergoing surgical hip dislocation following SCFE. All hips had femoral metaphyseal damage consistent with FAI. Thirteen hips had extensive damage to the labrum, and 12 hips had damaged anterosuperior cartilage. Cartilage abrasion was observed even in those patients who had been symptomatic for only a few weeks. In all patients the metaphysis was level or extended more anteriorly than the femoral head revealing rough edges and in some cases bleeding ulcerations of the metaphyseal surface. Independent of the degree of SCFE, flexion of the hip joint and internal rotation caused impingement of the metaphysis against the superomedial acetabulum and labrum. Acetabular cartilage damage appeared in forms ranging from chondromalacia, to cleavage, to full thickness loss of cartilage. Acetabular cartilage damage extended from the rim into the joint by 1 to 1.5 cm and along the rim for up to 3 cm (see Case 1).
Sink et al. (13) described similar evidence of early joint disease in 38 hips treated with in situ pinning at a mean of 20 months prior to surgical hip dislocation. The group consisted of 8 mild, 19 moderate, and 11 severe slips. None of these hips had prior slip progression after fixation, screw penetration, or avascular necrosis. Cartilage damage was present in 32 hips and labral injury in 33 of 38 hips.
Goodman et al. (14) evaluated a large group of cadaver skeletons to identify hips with post-SCFE morphology. The characteristic findings of previous SCFE deformity were present in 6% (215 specimens). The acetabular bone was evaluated for significant arthritic changes without reference to the femoral morphology. Thirty-eight percent of hips with prior SCFE deformity had evidence of significant osteoarthritis in contrast to 26% of morphologically normal hips.
Clinical Implications of FAI in SCFE
FAI commonly occurs and may go undetected after SCFE. Dodds et al. (15) have reviewed the clinical findings and slip characteristics of 49 patients (65 hips) to assess the symptoms and outcomes after skeletal maturity. The average age at presentation was 12.2 years. The stability of the slip was available in 82% of patients. Sixty-two percent were stable. Fourteen percent were preslips (grade 0), 58% were grade 1, 20% were grade 2, and 8% were grade 3. They were able to contact 38 patients (78% of the study cohort) with 51 SCFEs. The authors reported that 15 hips were painful (31%). The mean Harris Hip Score was 96.6 and the clinical findings of FAI were present in 33% of the hips. A recent unpublished study from the Mayo Clinic has also reported that 41 hips from a group of 170 hips in 146 patients who underwent in situ pinning continued to have pain at an average of 19 years. Pain rated by visual analog scale was 2.5 (range: 0 to 10). The mean UCLA score was 8 (range: 3 to 10), and the Marx activity score was 5 (range: 0 to 16). The mean Harris Hip Score was 90 on the affected side.
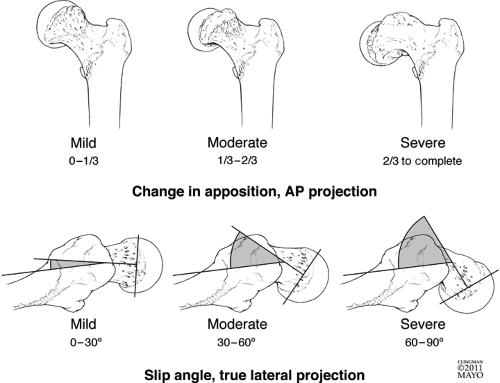
Classification
The post-SCFE deformity can be classified either by slip angle or by the SCFE slip percentage. The slip angle is measured by drawing a line parallel to the long axis of the femoral neck and the angle formed by a line parallel to the long axis of the epiphysis. Angles less than 30 degrees are considered mild, between 30 and 50 moderate, and over 50-degrees severe slip angles (Fig. 50.2). The SCFE slip percentage is considered mild if it is less than 25% of neck diameter, moderate 25% to 50% of the neck diameter, and severe if there is greater than 50% of slip of the epiphysis with respect to the neck diameter. Femoral head translation on the neck is not taken into account in these classifications however, and may actually be of utmost importance in the management of these hips as a combined angular and posterior translational deformity is seen quite often.
With the existing classifications, it is the severity of hip slip angle and percent of slip in addition to the restrictions in range of motion and clinical symptoms that will help determine the appropriate treatment for these patients. The data available to guide treatment for the healed post-SCFE deformity is limited. There is often a mix of patients within the papers and healed SCFEs are treated but often not enough data is presented to allow accurate extraction of surgical technique or even outcomes pertaining to this special group. We, therefore, present the data available and then describe the author’s preferred technique for management of the healed post-SCFE deformity. The surgical strategies will be presented as (1) hip arthroscopy techniques, (2) open approaches without proximal femoral osteotomies, and (3) open approaches with proximal femoral osteotomies.
Hip Arthroscopy Technique
Femoral Head–neck Junction Osteochondroplasty
For hips with mild slip angles resulting in little deformity, osteochondroplasty of the head–neck junction is a proposed treatment for the resultant femoroacetabular impingement. Leunig et al. (16) report treating three patients with acute mild slips using single-screw fixation followed by arthroscopic osteochondroplasty of the prominent metaphysis. Two of these patients had slip angles of 18 degrees and the third a slip angle of 23 degrees. All slips were classified as stable and had positive impingement signs. In two cases, preoperatively there was no hip internal rotation and in the third internal rotation was 20 degrees less than the contralateral hip. During arthroscopy all hips demonstrated anterolateral labral fraying with adjacent chondromalacia. Postoperatively the alpha angles corrected from 80 to 42 degrees, 90 to 50 degrees, and 88 to 44 degrees. At follow-up ranging from 6 to 23 months, the patients were pain free and resumed all activities. Impingement testing had returned
to normal and hip internal rotation was within 10 degrees of the contralateral hip.
to normal and hip internal rotation was within 10 degrees of the contralateral hip.
Hip arthroscopy can also be used for the treatment of the healed SCFE hip. Whether to perform the femoral head osteochondroplasty through the scope or open depends on the surgeon’s expertise and how high on to the neck the deformity extends. The AP radiograph of the hip can give significant insight as to how far the cam lesion or proximal femoral deformity extends. Even mild slip angles present a level of deformity that is difficult to treat arthroscopically alone as the femoral bone extends above the retinacular vessels (see Case 1). The authors recommend arthroscopic treatment of the cam lesion in patients with mild slips which maintain at least 5 to 10 degrees of hip internal rotation at 90 degrees of flexion and no involvement of the femoral neck above the retinacular vessels. The amount of femoral neck which can be removed without undue risk of femoral neck fracture is certainly less than 30% of the neck diameter but this data cannot be used indiscriminately in this patient group as posterior translation of the head occurs and needs to be taken into consideration during preoperative planning (17).
Open Approaches and Techniques (Without Proximal Femoral Corrective Osteotomy)
Osteochondroplasty can similarly be performed via an anterior hip arthrotomy or a surgical hip dislocation. In 1957, Heyman et al. (18) reported performing femoral osteoplasty of the metaphyseal prominence in SCFE. This was performed via a Smith-Petersen approach with the additional use of bone block epiphysiodesis when the physis had not yet closed. Significant improvements in range of motion and function were reported in 21 hips treated in this manner. There are reports of modern anterior mini-open approach describing femoral head–neck junction osteochondroplasty (19,20). This approach also has difficulties in exposing and treating the posterolateral aspect of the femoral head–neck junction but may be more precise for this location than hip arthroscopy. These papers do not give any details specifically about SCFE patients.
Surgical hip dislocation as described by Ganz et al. (21) allows direct visualization of the femoral head and acetabulum permitting dynamic visualization of impingement (see Case 2). This method has the advantage of allowing the most complete visualization of the femoral head and acetabulum including a dynamic assessment of impingement. Shin et al. (22) reported using a surgical hip dislocation in 23 hips of 21 patients with mean age of 15.7 years. This included seven patients with SCFE of which four had healed SCFE deformities. Two patients with mild slips were treated with osteochondroplasty alone, two patients had addition of an intertrochanteric osteotomy, one a base of neck osteotomy, and two had an open reduction of unstable severe slips with subcapital cuneiform osteotomy. Only one patient developed femoral head osteonecrosis but was found to have an avascular head at the time of surgical dislocation. Rebello et al. (23) reviewed 57 patients (58 hips) with developmental conditions including Perthes, SCFE, DDH, and osteonecrosis treated via a surgical hip dislocation. The average age was 15.7 years (range: 8 to 38) with mean 41.6-month follow-up. This group included 29 patients with SCFEs of whom 17 had prior screw fixation and 1 a prior osteotomy. Treatment of the SCFE patients included a head–neck osteoplasty in seven, intertrochanteric osteotomy in five, intertrochanteric osteotomy with osteoplasty in eight, femoral neck osteotomy in four, and open reduction and fixation in five with unstable SCFEs. In the SCFE patients, WOMAC average pain scores improved from 7.9 to 3.5, stiffness from 2.9 to 2.3, and the function score from 18.7 to 11.1. The overall rate of osteonecrosis was 7% (4/57). Three were associated with femoral neck osteotomies and the other with an intertrochanteric osteotomy. (Two of the femoral neck osteotomies were done for severe SCFE deformity with closed or partially closed femoral physis and the other for delayed presentation of an undiagnosed femoral neck fracture.
Surgical hip dislocation in the older patient with a healed SCFE deformity allows for precise correction of the anatomy. It is through this approach that the surgeon can dynamically assess impingement and decide whether femoral head neck osteochondroplasty alone is sufficient or whether realignment procedures are required as well. A definite advantage of hip dislocation over other surgical approaches to treat SCFE hip deformity is the ability to progressively extend the approach into other procedures such as a proximal femoral osteotomy at the neck or intertrochanteric region and advancement of the trochanter for relative neck lengthening as needed. It is the author’s surgical approach of choice for the patient with higher slip grades in whom obligate external rotation at 90 degrees of flexion is seen, many times with some external rotation contracture (i.e., minus IR) (see Case 3).
Open Approaches with Corrective Proximal Femoral Osteotomies
Proximal Femoral Osteotomies
Realignment procedures for moderate and severe slips have been described at the subcapital, cervical, base of neck, intertrochanteric, and subtrochanteric levels. The risk of osteonecrosis at the time of realignment is greater the closer the osteotomy is performed to the physis. This can be explained by injury to the blood supply of the epiphysis. On the other hand, correction of the deformity closer to the epiphysis allows potentially more anatomic restoration of the proximal femur and normalization of hip range of motion.
In choosing a treatment for SCFE deformity the degree of slip can serve as a guide to choose whether femoral head–neck osteochondroplasty or an osteotomy would be most beneficial. This concept is illustrated by the report of Szypryt et al. (24




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree