Femoral Head Osteonecrosis: Overview
Michael A. Mont
Aaron J. Johnson
Introduction
The disease now called osteonecrosis was originally described by Haenisch in 1925 as ischemic necrosis in the hip (1), and has been given various names, including avascular necrosis, atraumatic necrosis, and idiopathic necrosis. Its hallmark is bone death, and this most often affects the hip though less commonly other weight-bearing joints (i.e., shoulder, knee). Since its original description, much research has been done to identify risk factors, to classify the progression of disease, and to determine appropriate treatments; however, despite these advances, little is known regarding its exact etiology. Although patients of any age can be affected, those in their third decade of life are particularly prone (2), with an annual prevalence of 10,000 to 20,000 new cases per year in the United States. Without treatment, the natural history indicates that greater than 80% of symptomatic cases (2), and nearly two-thirds of asymptomatic hips will progress to end-stage degenerative joint disease requiring surgical intervention (3,4). Treatment options have evolved to include potential nonoperative pharmacotherapies, joint-preserving surgeries, and various joint-arthroplasty techniques. Various treatment algorithms have been proposed that are most often based on the radiographic extent of the disease.
The purpose of this chapter will be to provide an overview of osteonecrosis of the hip including a description of etiologies, associated risk factors, diagnostic criteria, classification schemes, and a brief summary of various treatment methods.
Pathophysiology and Etiology
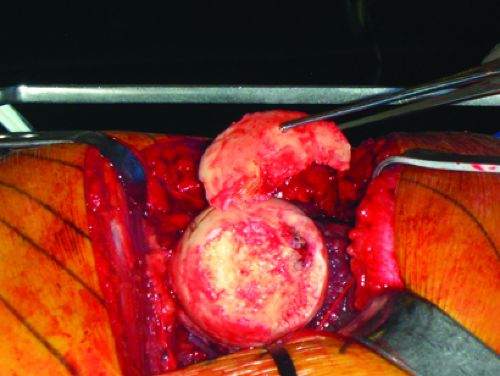
The pathophysiology and etiology of osteonecrosis are not fully understood for atraumatic cases. Studies addressing the natural history of the disease have suggested that the location and size of the lesion affect progression. Lesions smaller than 15% of the volume of the femoral head in asymptomatic patients may heal spontaneously (4). Larger lesions typically undergo a pathologic repair process that eventually leads to collapse of the bone and destruction of the overlying articular cartilage. This reactionary repair process begins with the partial absorption of the necrotic tissue, where new bone is formed over dead trabeculae. This leads to a sclerotic, inflammatory lesion. Following this, osteoclast-mediated bony resorption occurs, along with fibrosis. Small microfractures then begin to develop in the necrotic area, which can accumulate and lead to subchondral fractures. Over time, this will ultimately result in collapse of the femoral head and the painful end-stage degenerative joint disease (Fig. 21.1).
Two different explanations have been offered concerning the occurrence of the above pathologic process: extraosseous or intraosseous. An extraosseous process would occur when the blood flow to the hip has been compromised; intraosseous processes may involve a hyperlipidemic state that ultimately leads to bone death. In addition, vascular embolization and increased intraosseous pressures have been offered as potential mechanisms of altered blood flow.
Regardless of the exact mechanism of vascular insufficiency to the bone, the importance of maintaining blood flow has been described (5). McCarthy summarized the events that occur in osteonecrosis following the initial ischemic event. The hematopoietic marrow is affected first,
followed by fatty marrow, vascular structures, and finally bone itself. Although these are the general events that lead to cell death, the causative events that lead to this pathway are a complex combination of risk factors that are not fully understood.
followed by fatty marrow, vascular structures, and finally bone itself. Although these are the general events that lead to cell death, the causative events that lead to this pathway are a complex combination of risk factors that are not fully understood.
Other investigators have studied the molecular and genetic basis for the disease (6,7,8). One study indicated that a type II collagen gene (COL2A1) may be present in patients who are at risk for osteonecrosis (8). Another study found a gene on the same chromosome as COL2A1 that was associated with familial osteonecrosis (6). Genes that regulate coagulation (7), lipid transport and metabolism (9), and nitric oxide synthesis (10,11) have also been associated with an increased risk for the disease, whereas other genes have been described to be protective against the disease (12). A recent study identified a deficient production of vascular endothelial growth factor-D in the bone marrow of patients affected with the disease (13). These collective and future studies may lead to a better understanding of the possibility of a genetic predisposition to the disease and the potential for osteonecrosis screening tests that could help identify at-risk patients.
Histologically, osteonecrosis has a characteristic appearance. The major difference when compared to a healthy bone is a markedly decreased ratio of normal osteocytes to empty lacunae (14,15). When studying the histologic changes in osteonecrotic bone from patients who were corticosteroid users, more bone marrow edema, fat necrosis, and fibrosis were observed, along with a higher percentage of dead trabeculae, when compared to patients who had osteonecrosis with other risk factors (16). Regardless of the specific causative factor, once bone death occurs, the necrosis and repair process follow a similar pattern. In addition, because the histologic stage does not necessarily correlate with the radiographic stage of the disease, classification systems have been proposed that attempt to grade the extent of osteonecrosis by the degree of osteocyte death, marrow necrosis, and extent of fibrosis (17,18). However, these systems are not commonly used since by being invasive, they are less useful in preoperatively determining an appropriate treatment course when compared to radiographic staging.
Risk Factors
The many risk factors for developing osteonecrosis of the femoral had can be separated into two broad categories: direct causes (including traumatic) and indirect causes. Each has a different proposed mechanism by which it leads to the same final pathologic process, described above. In addition to trauma, other direct causes of osteonecrosis include Caisson disease, Gaucher’s disease, certain coagulopathies, irradiation, and some autoimmune diseases. Indirect risk factors include corticosteroid use, alcohol consumption, smoking, and severe acute respiratory syndrome (Table 21.1).
Traumatic hip injuries are the most common direct cause of disruption of blood flow to the femoral head leading to osteonecrosis. The trauma of femoral neck fractures and dislocations lead to a compromised blood supply. Because there is little collateral vascularization to the hip, damage to the lateral epiphyseal arteries, the femur’s nutrient artery, or the ligamentum teres artery can result in ischemia to a large portion of the femoral head.
Table 21.1 Risk Factors Associated with Osteonecrosis | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Caisson disease, also termed “decompression sickness,” was originally described during the building of the Brooklyn Bridge during the 1870s when workers were subjected to three to four times normal atmospheric pressures (19). It was later discovered that nitrogen disequilibrium was a consequence of rapid changes in atmospheric pressure, resulting in nitrogen bubbles forming in the vasculature that can ultimately cause ischemia in the hip (and other large joints). Although other, more systemic manifestations of the disease have been reported, severe hip pain led to the workers walking with a characteristic forward bend at the waist, which was similar to a “fashionable” trend of the 1870s, whereby women would walk with a similar “Grecian Bend”; hence, the disease has also been given the name “the bends.” Modern manifestations of the disease are seen in miners (or other workers who are subjected to rapid atmospheric pressure changes), SCUBA divers, and pilots who are subjected to rapid changes in altitude (20).
Gaucher’s disease is a lysosomal storage disease that results in fatty accumulation within the organs (including the bone marrow) caused by a deficiency of the enzyme glucocerebrosidase. This fat accumulation can lead to an infarct within the femoral head, resulting in osteonecrosis. As many as 30% of individuals who have Gaucher’s disease may eventually develop this disorder (21).
Inherited coagulopathies (e.g., sickle cell disease, or factor-specific thrombophilic and hypofibrinolytic disorders), autoimmune diseases (e.g., systemic lupus erythematosus), and other disease states (e.g., human immunodeficiency virus) can be risk factors for osteonecrosis. Thrombophilia and hypofibrinolysis are coagulopathies that may lead to ischemic conditions and subsequent osteonecrosis. Severe acute respiratory syndrome (a severe respiratory infection caused by a coronavirus that was responsible for a worldwide epidemiologic crisis in 2003) was recently identified
as a risk factor (22). It is uncertain, however, whether this disease state is an independent risk factor for developing osteonecrosis, or if it is the treatment methods (which often includes the use of corticosteroids) is the cause.
as a risk factor (22). It is uncertain, however, whether this disease state is an independent risk factor for developing osteonecrosis, or if it is the treatment methods (which often includes the use of corticosteroids) is the cause.
Corticosteroid use is the most commonly identified risk factor for the development of osteonecrosis. It was first identified in 1957 by Pietrograndi to have a causal relationship (21). The major mechanism that has been proposed has been a predisposition for fat cells to hypertrophy in response to chronic corticosteroid use in certain individuals (23). Some authors have postulated that this increased marrow volume may lead to higher intracortical pressures and reduced vascular flow in closed compartments, such as the femoral head; others have suggested that use directly inhibits the development and proliferation of the osteoblast, and thereby augments the normal bone turnover process to favor osteoclastic activity (23,24,25). Regardless of the mechanism, it has been shown that a daily dose greater than 2 g for a minimum duration of 2 to 3 months results in an increased risk for developing the disease (26), which usually presents within 3 to 24 months after their initial use (27,28,29).
Japanese studies have correlated risk factors for the development of the disease and have linked alcohol and smoking to osteonecrosis (30,31). People who consume greater than 400 mL per week of alcohol (or approximately 22 alcoholic beverages) have a purported 11 times relative risk when compared to nondrinkers (31). These same studies have also identified a smoking history of at least 20 pack-years as a risk factor (30). For alcohol consumption, the proposed mechanism has been increased hyperlipidemia and fat emboli resulting from liver damage. In smokers, it may be the direct damage to the vasculature by the nicotine. However, it is difficult to separate the effects of smoking and alcohol consumption, as the studies examined the same patient population, and drinking and tobacco use often correlate. Although the exact mechanism is not understood, it may be possible that there is a synergistic effect of the two that leads to osteonecrosis in genetically susceptible individuals.
Patient Work-up and Diagnosis
The following section will outline the clinical, radiographic, and intra-operative tests that are useful in the diagnosis of osteonecrosis. The acute onset of groin pain with intermittent pain on ambulation is the hallmark of this disease; however, 10% to 15% of patients may present with nonspecific pain. It is often described as deep and throbbing, occasionally with noted radiation to the knee. If the location of the pain is uncertain, a diagnostic hip injection can be helpful in confirming the source as intra-articular.
It is important to evaluate each patient with respect to their age, activity level, and general health, in order to best develop a treatment algorithm specific to their needs. Severe systemic illnesses or short life expectancy may preclude any or certain surgical treatment methods. In addition, highly active patients may be more demanding and consider different interventions than a more sedentary patient. Also, the morbidity of the proposed procedure must be considered, as well as its impact on potential future arthroplasty procedures. For example, total hip arthroplasty is reportedly more difficult in patients who have undergone prior free vascularized fibular grafting (32) or proximal femoral osteotomies.
Duration of symptoms has also been suggested to have had an effect on treatment outcomes. Beaule et al. (33) reported a better prognosis for patients treated with total hip resurfacing arthroplasty who had symptoms less than 12 months at the time of treatment. He noted that patients who had symptoms longer than 12 months had more acetabular involvement, and consequently had a shorter time to conversion to total hip arthroplasty. In addition, Mont et al. (34) have reported on patients with 45 osteonecrotic hips with a mean follow-up of 2 years (range, 20 to 39 months), and showed that there were more patients who had improved Harris Hip scores and lower revision rates if their symptoms were less than 6 months in duration (80% success, 24 of 30 hips), as compared to patients with symptoms of longer duration (57% success, eight of 15 hips).
Plain radiographs and magnetic resonance are the main imaging modalities used to aid in the diagnosis. Previous authors have described radiographic signs of osteonecrosis, separated into major and minor criteria (35). Major criteria include well-demarcated sclerosis and subchondral collapse (“crescent sign”) on plain radiographs, and hypointense banding on T1-weighted magnetic resonance imaging (MRI) (Figs. 21.2 and 21.3). Minor criteria are joint space narrowing with femoral head collapse, mottled sclerosis, and




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree