Core Decompression for the Treatment of Osteonecrosis of the Femoral Head
Lauren E. Geaney
Jay R. Lieberman
Introduction
Core decompression for treatment of osteonecrosis (ON) of the femoral head represents a family of procedures that may include vascularized or nonvascularized bone grafts, bone marrow aspirate (BMA), other biologic agents that promote bone repair, or just the core tract alone (1). In a recent systematic review of the literature we evaluated the results of femoral head saving procedures published over the past 10 years and concluded that core decompression is most effective in the early stages of ON and when the lesions are smaller and involve a limited amount of the weight-bearing surface of the femoral head (2). Core decompression is ineffective when the femoral head has already collapsed (2). In this chapter we will review the most recent techniques for and results of core decompression of the femoral head in the treatment of ON. While we appreciate the contribution of many decades worth of quality investigations, this chapter will mainly focus on the last 10 years of research.
Case Report
Presentation
In this case we will describe the use of core decompression combined with bone morphogenic protein (BMP) and BMA. The osteonecrotic bone in the femoral head is debrided with a burr via the core tract (“core debridement”), and the hypothesis is that the bone marrow cells will respond to the BMP and lead to enhanced bone repair.
GM is a 35-year-old gentleman presenting to the office with a 6-month history of progressive right hip pain, describing it as a constant, dull ache. His pain has now become so severe that he requires a cane for ambulation and has modified his job as a police officer so that he now only performs desk work.
His past medical history is significant for hypertension and a course of steroids 8 years prior for the treatment of Bell’s palsy. He denies any significant alcohol history.
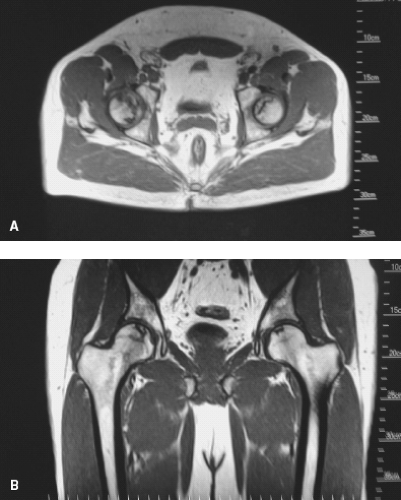
On examination, he walks with a limp and has minimally decreased internal rotation on the right side compared with the unaffected extremity. Radiographs obtained at this time include AP and frog-leg lateral films which showed only mild sclerosis (Fig. 56.1). However, an MRI of the bilateral hips revealed ON of the hip at stage IA/B according to the Steinberg classification (3), and localized in A/B location according to the classification system of the Japanese Orthopaedic Association (JOA), involving some degree of the weight-bearing surface (4) (Fig. 56.2). The asymptomatic hip also had involvement.
Classification
The ideal classification scheme for staging of ON should in-clude the treatment regimen, prognosis and have good intero-bserver and intraobserver reliability. One early classification
system was described by Ficat and Arlet (5,6) and was a four-stage classification scheme based on plain radiographic findings. The four stages were defined as follows: stage 0 was defined as preclinical; stage I is a symptomatic hip that shows no changes on x-rays; stage II is marked by sclerosis of the femoral head; stage III by femoral head collapse and stage IV by progressive loss of joint space (5). This classification was later modified to include IIB as a transitional stage that included the presence of a crescent sign (7).
system was described by Ficat and Arlet (5,6) and was a four-stage classification scheme based on plain radiographic findings. The four stages were defined as follows: stage 0 was defined as preclinical; stage I is a symptomatic hip that shows no changes on x-rays; stage II is marked by sclerosis of the femoral head; stage III by femoral head collapse and stage IV by progressive loss of joint space (5). This classification was later modified to include IIB as a transitional stage that included the presence of a crescent sign (7).
Marcus and Enneking (8) devised a classification scheme prior to this in 1973. Stage I is an asymptomatic hip with normal radiographs, stage II is defined by well-demarcated sclerotic or cystic lesions, stage III is subchondral collapse with a crescent sign, stage IV is flattening, and stage V osteoarthritis and joint space narrowing.
Steinberg et al. (3) subsequently devised the University of Pennsylvania System of Classification and Staging. The advantage of this staging system is that it incorporates MRI to detect a preclinical lesion and determines the size of the lesion (9). There are six stages with the extent of involvement of the head classified as A (<15% involved), B (15% to 30% involved), or C (>30% involved).
The Association Research Circulation Osseous (ARCO) attempted to create a more universal classification system (4,10) which incorporated the quantification system used by Steinberg et al. but added a subclassification of location as medial, central, or lateral. A separate classification system was also created by the JOA and their Ministry of Health which also considers the location and extent of the lesion in the classification (11).
Unfortunately, with multiple classification systems available for use (Table 56.1) it is difficult to compare outcomes of different techniques. A validated universal classification system would be ideal to analyze outcomes of treatment of ON.
Natural History
Interest in the treatment of ON of the hip has arisen from the recognition that the natural history results in poor outcomes. In 1965, D’Aubigne (12) noted that collapse occurred in 20% of hips treated nonoperatively in the first year and by 3 years after diagnosis, only 25% had not collapsed. Half of the patients had progression of disease. Recently, the natural history of ON has been elucidated by following patients who refused surgical management or by following the asymptomatic hip in patients with bilateral disease. In a recent review of the literature, Mont et al. (13) compared the results of core decompression with nonoperative management and found that only 146 of 559 (26.7%) of the patients treated nonoperatively showed no femoral head collapse after a mean follow-up of 34 months and 174 of 219 hips (80%) required total joint arthroplasty over that time. In the patients treated with core decompression, 741 of 1,166 hips (63%) showed no progression and 341 of 1,029 hips (23%) required arthroplasty after a mean of 30 months. Better results were seen in patients with Ficat stage I disease.
Hernigou et al. (14) prospectively followed 40 asymptomatic, small, stage I lesions in patients with symptomatic contralateral disease and discovered that 35 of 40 (88%) of the hips became symptomatic after an average of 11 years. Twenty nine hips (73%) had collapsed at that time. Symptoms always preceded collapse by 6 months and there was an average of 80 months between diagnosis and evolution of symptoms. In a study by Ohzono et al. (15), progression of ON treated nonoperatively was most closely related to the stage of the lesions. Eighty eight percent (28 of 32 hips) of Ficat stage II hips that were also categorized as JOA classification stage IC lesions progressed to Ficat stage III. In addition, 94% (64 of 68) of all patients with JOA 1C lesions had collapsed at 3 years.
There is general agreement that patients with symptomatic ON nearly always progress both clinically and radiographically (15,16,17,18). The results of the studies mentioned above suggest that the timing of the surgery may be delayed until the onset of symptoms since pain usually precedes collapse (1,19). The senior author has had patients in his practice that have had ON for years without collapse of the joint, including the asymptomatic contralateral hip in the case presentation.
Core Decompression
Despite the limitations of the available data, most orthopedic surgeons agree that joint preserving surgery is appropriate because the majority of patients in the precollapse phase are between 20 and 50 years of age (20,21). Core decompression was first described as a technique for diagnosis of ON. Ficat et al. (5) described the procedure as introducing a 6- or 8-mm trephine into the lesion from a starting point on the lateral
cortex of the greater trochanter. This produced a biopsy of bone for definitive histologic diagnosis. Following this procedure, however, it was noted that patients had improved outcomes with good results obtained in 94% of the patients with Ficat stage I disease (5). They concluded that the success of core biopsy was due to decompression of the femoral head, permitting venous drainage, and relieving congestion (5). It was later shown that intraosseous pressure is elevated and the partial pressure of oxygen is lower in patients with ON. Core decompression seems to reverse these effects (22), but the etiology of ON has not been identified.
cortex of the greater trochanter. This produced a biopsy of bone for definitive histologic diagnosis. Following this procedure, however, it was noted that patients had improved outcomes with good results obtained in 94% of the patients with Ficat stage I disease (5). They concluded that the success of core biopsy was due to decompression of the femoral head, permitting venous drainage, and relieving congestion (5). It was later shown that intraosseous pressure is elevated and the partial pressure of oxygen is lower in patients with ON. Core decompression seems to reverse these effects (22), but the etiology of ON has not been identified.
Table 56.1 Summary of Classification Systems for Osteonecrosis of the Femoral Head | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
At the present time, core decompression represents a family of procedures. A single large tract or multiple small tracts may be created in the femoral head and the core decompression may be supplemented with various types of grafts and other biologic agents that may promote bone repair. There is no clear consensus with respect to the ideal candidate for these procedures, nor is there a unified conclusion as to which procedure is most effective.
The success rates of core decompression in the published literature are extremely variable. Some of this arises from the use of multiple classification systems along with the fact that the true natural history has not been definitively elucidate. In addition, the surgical technique varies considerably between surgeons (9), and the definition of success and failure of the procedure is variable. In our opinion, a successful result should provide significant pain relief and prevent collapse of the femoral head for at least 5 years. In a prior decision analysis, we noted that for a core decompression to be cost-effective, it had to delay a second procedure for 5 years (23).
Over the years the reported success rates with core decompression have been quite variable (24) (Table 56.2). Based on the available literature, it appears that outcomes are influenced by the presence of collapse of the femoral head and the extent and location of osteonecrotic lesions. Although the variety of the classification systems used makes it difficult to compare studies, patients with earlier stage lesions that are precollapse, have better results with longer duration of survival (25,26,27,28). One study further differentiated between Steinberg stage IIA sclerotic hips and stage IIA cystic hips. They found that those patients with cystic
changes on radiographs had poorer outcomes than those with pure sclerotic disease (26).
changes on radiographs had poorer outcomes than those with pure sclerotic disease (26).
Table 56.2 Summary of Literature on Core Decompression Within the Last 10 Years | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|