Treatment of Overuse Sports Injuries
Carlos A. Guanche
Introduction
Approximately 5% to 21% of all athletic injuries involved the hip and pelvis (1,2). In one study, overuse accounted for 82.4% of the injuries to the hip and pelvis that presented to a general sports medicine clinic (1). Another investigator has cited that 25% to 70% of runners sustain overuse injuries during any 1-year period (3). Regardless of the level of athletic competition whether it be recreational, high school, college or professional, overuse injuries to the hip and pelvis region are equally common. The exact cause of these pathologies has yet to be determined. The etiology seems to be multifactorial and diverse in nature (4,5). With increasing reports in the literature, there has been more awareness of these injuries as an etiology of low back, buttock pain, and groin pain.
One aspect that should be considered is that, by definition, an overuse injury as discussed in this treatise is one without a clear mechanical cause. Namely, disease processes involving tears of the acetabular labrum, femoroacetabular impingement, and dysplasia of the hip are structural problems that lead to hip and lower extremity pain and dysfunction and may improve with rest for a period of time. However, these processes will not completely resolve even with multiple courses of rest as described for most of the other entities discussed in this chapter.
Hip pain in athletes involves a wide differential diagnosis and can, to some extent, be correlated with the age of the patient. Adolescents and young adults are at particular risk for various apophyseal and epiphyseal injuries because of lack of ossification of their cartilaginous growth plates. Older athletes are more likely to present with tendinitis in these areas because their growth plates have closed. Several bursae in the hip area are prone to inflammation and can be a large source of pain and disability. A methodical physical examination that specifically tests the various muscle groups that move the hip joint can help determine a more exact diagnosis for the often vague complaint of hip pain.
History
The age of the patient may suggest different diagnostic possibilities. As mentioned earlier, younger athletes are more prone to apophyseal injuries. Repetitive stress avulsion fractures are also more likely in skeletally immature patients. Bursitis and muscle strains are more likely to be seen in skeletally mature active young adults. Degenerative arthritis becomes more common with advancing age and is seen primarily in older adults.
For all age groups, an accurate diagnosis depends on a careful history. Patients whose hip pain is caused by pathology in other organs may have other associated symptoms. Unexplained weight loss, fever, and night sweats indicate the possibility of a systemic inflammatory process. Genitourinary and abdominal symptoms likewise may indicate that the pathology is located in one of these areas instead of the hip. A careful search for these symptoms is indicated for patients with a history of disease in these systems, as well as for those who do not have findings consistent with musculoskeletal disease.
General Physical Examination Considerations
The physical examination of the hip is similar for athletes of all ages. Using a stepwise approach, including observation, palpation, and testing for range of motion and strength, will help ensure that important findings are not missed.
Observation
A limited functional evaluation includes determining whether the affected leg can bear weight. If it can, important points to observe include the patient’s posture, gait, and ability to transfer independently from standing to sitting to lying down, and then back to standing.
If the patient is able to stand erect, the examiner can estimate the height symmetry of the iliac crests by resting their hands on the iliac wings. If the crests are asymmetric or the patient is unable to stand, the next step is to compare leg lengths: The distance between the anterior superior iliac spine (ASIS) and the medial malleolus of each leg. Leg length discrepancies have been implicated in a number of musculoskeletal hip and leg injuries. Differences greater than 2 cm may merit correction with heel lifts, as these may contribute to overuse injuries such as trochanteric bursitis (6).
Palpation
Palpation can be performed with the patient standing or lying down. Careful palpation of each muscle group in the
area of the symptoms may help to localize vague complaints to a specific structure. In particular, palpation can identify tenderness over the sites of muscle attachment to bone and the bursae.
area of the symptoms may help to localize vague complaints to a specific structure. In particular, palpation can identify tenderness over the sites of muscle attachment to bone and the bursae.
Range of Motion
Normal ranges of motion are dependent on the patient’s stage of skeletal development, with the range tending to decrease as age increases. Decreased range of motion on the side of the affected hip should heighten the suspicion of an underlying injury. Specific injuries may be suggested by certain defects in range of motion (7). Passive and active motion should both be assessed.
Muscular Strength Testing
Muscle strength should be tested for the affected and unaffected hip to enable the physician to compare strength and detect subtle deficits. Hip flexion strength is best tested with the patient in a sitting position, lifting against the examiner’s hand. External and internal rotation also can be evaluated in this position, with the examiner providing resistance against the patient’s lower leg. Abduction and adduction are best tested with the patient supine and the examiner providing resistance against the medial and lateral side of the knee. Extension strength is best tested with the patient prone and the examiner applying resistance against the lower leg. Although the piriformis is an external rotator of the hip, it is best tested with the patient supine.
Functional Anatomy
A complete discussion of hip and pelvic anatomy is provided in other parts of this text. However, some basic anatomical descriptions as they relate to the development of overuse injuries, and in particular stress fractures, will be discussed. In younger patients, nonossified bone present at growth plates such as the femoral head epiphysis and the ASIS apophysis is susceptible to injury until the skeleton matures. Maturation of these growth plates varies by site and among patients. Usually, the last area to mature is the ASIS apophysis, which may be susceptible to injury up to age 25 (8). Active young adults who are skeletally mature are at increased risk for stress fracture of the femoral neck (9). Older adults are at risk for degenerative arthritis and fracture of the femur and pelvis (10).
The important link between the pelvis, trunk, and lower extremities is critical to understand. The bony architecture of the hip joint shows primary compression and tension trabeculae of the femur that carry on through the pelvis, iliac crest, and lumbar spine. This trabecular pattern allows the hip to handle peak focal pressures of approximately 3,000 lb/in2, which occurs from sitting to standing (5). The multiaxial ball and socket joint of the hip has three degrees of freedom, whereas stability is provided through the acetabular triangular fibrocartilage which adds more congruency to the articular surfaces. The biomechanics of the neck–shaft angle of 120 to 130 degrees along with an average of 14 degrees of anteversion allow for angular movements of the thigh to be converted to rotatory (transverse plane) hip motion.
Soft Tissue Overuse Injuries
Bursae
Bursae prevent excessive friction of soft tissue over bony prominences during motion. They may become inflamed and cause “snapping” or pain as the result of repetitive activities or direct trauma. The trochanteric bursa is located lateral to the greater trochanter and is the most commonly injured bursa in the hip. The iliotibial band (ITB) and gluteus muscles pass over this area. Either area can contribute to excessive friction and cause clinical symptoms that are very similar (11).
Falls onto the lateral hip and overuse injuries (especially common in runners and dancers) are the most common causes of trochanteric bursitis. After passing over the greater trochanter, the ITB inserts at the knee on the lateral aspect of the tibia, so patients with ITB syndrome may also complain of lateral knee pain. While the mechanisms vary, the ITB is under tension throughout the hip’s range of motion, and as the hip is extended the ITB lies posterior to the greater trochanter. It moves anteriorly with flexion and in some patients there is a thickened portion posteriorly that can snap over the greater trochanter. The anterior aspect of the gluteus maximus can also create external snapping as it rubs over the greater trochanter. The greater trochanteric bursa may also become inflamed and painful as a result of this mechanical irritation, causing disability. With tightness in the ITB, symptomatic patients complain of pain over the lateral aspect of the hip and may feel snapping at the ITB over the greater trochanter with flexion and extension (Fig. 61.1). Ober test is done to check specifically for ITB syndrome. The patient should be able to drop the affected leg to the table without discomfort while lying on the unaffected side. In patients with ITB syndrome, the maneuver causes pain along the lateral side of the thigh (12).
Treatment, in most cases involves rest and activity modification as well as the use of PT for stretching and modalities in an attempt to relieve the repetitive stress over the bursa. In refractory cases, surgical intervention can be entertained. This involves the creation of a window in the ITB, directly over the trochanteric bursa (13) (Fig. 61.1).
Another commonly injured bursa is the one overlying the ischial tuberosity. Although a direct injury can result in chronic pain, refractory ischial bursitis secondary to partial ruptures of the hamstring origin and secondary bursitis can also lead to disability. Whether the pain is because of the partial rupture or simply due to a painful tendinopathy that may masquerade as ischial bursitis has not really been determined (Fig. 61.2). These injuries can be debilitating and often lead to significant limitations of activities in the population most affected by the problem, namely runners. As with trochanteric bursitis, the initial treatment focuses on activity modification, stretching of the hamstring origin, and the use of modalities. In refractory cases, an injection can be attempted under either radiographic or ultrasound guidance. There is limited data concerning the treatment of
partial avulsions with secondary bursitis (14,15). Cohen and Bradley (14) recommends consideration of nonoperative treatment for acute partial avulsions, whereas Lempainen et al. (15) reported good results with repair of partial avulsion that had failed initial nonoperative treatment. The differential diagnosis includes a hamstring strain, an apophysitis, or even an avulsion fracture in a skeletally immature athlete (Fig. 61.3).
partial avulsions with secondary bursitis (14,15). Cohen and Bradley (14) recommends consideration of nonoperative treatment for acute partial avulsions, whereas Lempainen et al. (15) reported good results with repair of partial avulsion that had failed initial nonoperative treatment. The differential diagnosis includes a hamstring strain, an apophysitis, or even an avulsion fracture in a skeletally immature athlete (Fig. 61.3).
 Figure 61.3. Ischial apophyseal avulsion (black arrows) in a 16-year-old runner. The pain and discomfort had been present for 2 years. |
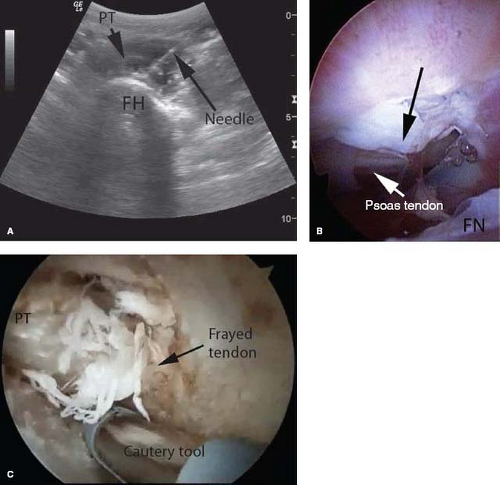
Less commonly injured is the iliopsoas (iliopectineal) bursa, which cushions the iliopsoas muscle as it sweeps over the femoral head and inserts on the lesser trochanter. Patients with an inflamed iliopsoas bursa usually complain of anterior groin pain, which is worse with resisted hip flexion. Once again, refractory cases that do not respond to stretching, activity modification, and PT modalities are considered for surgical intervention. In the case of psoas releases, there are traditional open methods as well as more recent endoscopic treatments that have been described with relatively equal success (16,17,18) (Fig. 61.4).
Apophyseal Avulsion Injuries
Apophyseal avulsion injuries, although rare, are becoming increasingly recognized among young athletes. These injuries are unique to adolescents and are particularly prevalent among those involved in athletics such as football, soccer, gymnastics, dance, hockey, lacrosse, volleyball, and track and field (19). Injuries are typically seen in athletes between the ages of 10 to 25 years old, prior to the completion of skeletal maturation (20).
Although the most common mechanism of apophyseal avulsion is a sudden, powerful contraction of the attached hip muscles, overuse injuries may also occur. Because the apophyses of the femur and pelvis undergo ossification later than other areas of bone about the hip, these areas of attachment of hip and abdominal wall muscle groups are typically weaker than their tendinous attachments. They are thus vulnerable to repetitive, microtrauma-induced apophysitis, or subacute rupture. Therefore, the same mechanism of injury that might result in a muscular strain in the adult patient is likely to cause avulsion or traction injuries in a pediatric or adolescent patient. Similarly, the sort of repetitive overuse microtrauma that can cause tendonitis in an adult patient is likely to be associated with apophysitis in a younger athlete. Areas most commonly affected include the ASIS and the ischial tuberosity, where the sartorius muscle and the hamstring and adductor muscles originate, respectively (21). Involvement of the anterior inferior iliac spine (AIIS), origin of the direct head of the rectus femoris, greater trochanter, into which the gluteus medius and minimus insert, or lesser trochanter, site of the iliopsoas insertion, may also be seen.
The hallmark presentation for acute apophyseal avulsion is an adolescent athlete who presents with acute onset of pain after an episode of strenuous activity. Patients may report feeling a “pop” followed by localized pain, swelling, and tenderness in the affected area. When questioned carefully, most of these patients will indicate that there had been a prodromal period of vague symptoms in the affected area (1). On physical examination, careful palpation of the bony landmarks of the pelvis and proximal femur will reveal localized tenderness. Similarly, active or passive stretching of attached muscle groups will result in reproduction of pain at the site of attachment.
In most cases, plain radiographs of the pelvis along with orthogonal views of the hip can give the necessary information with regard to the size and displacement of the avulsed fragment (Fig. 61.5). Radiographic evaluation may be more difficult in younger patients, and a high index of suspicion should be maintained. MRI is a useful adjunct, particularly when x-rays do not provide definitive diagnosis and as an indicator of degree of displacement. As a general rule, plain films alone are sufficient to diagnose apophyseal avulsion in the majority of cases. Notably, frog-leg lateral radiographs should be ordered in all adolescents complaining of hip pain to rule out slipped capital femoral epiphysis (SCFE).
The overwhelming majority of apophyseal injuries can be treated nonoperatively. Conservative management of nondisplaced and minimally displaced apophyseal fractures should typically include rest, ice, and protected weight bearing with crutches until symptoms resolve. Physical therapy, which should be initiated after a short period of rest, is an important adjunct. Therapy should begin with gentle stretching and passive range of motion exercises. Strengthening exercises that load the area of injury should be avoided until pain is completely resolved (7,22). Though minimally displaced fractures are initially considered nonsurgical problems, follow-up radiographs are needed to assure healing and appropriate development at the site of injury.
On rare occasions, significant displacement of an avulsed fragment or persistent pain refractory to conservative measures dictate the need for surgical intervention (23). There is some controversy in the existing literature as to precisely what degree of displacement warrants surgery (7). Although it is generally accepted that fractures that are either nondisplaced or minimally displaced should be treated nonoperatively, some authors have noted that fractures with any displacement are more likely to end in painful fibrous nonunion, which may limit function and eventually require delayed operative intervention (24). In general, fixation is advocated for displacement greater than 2 cm (25). With regard to the repair, some advocate open reduction internal fixation of the bony fragment, whereas others suggest resection of the fragment and reattachment of the tendon (24). Criteria for return to play should include radiographic evidence of bony healing and the absence of pain during activities similar to those performed in the sport. Time to recovery may vary, with some patients able to return to play in 6 weeks whereas others may require up to 6 months.
Osteitis Pubis
Pubic bone marrow edema likely reflects a degree of bone stress reaction occurring in the pelvis in athletes. In symptomatic athletes with osteitis pubis there are associated injuries at the pubic symphysis joint (26). Osteitis pubis can be thought of as a pubic symphysis joint injury with the stress noted on MRI reflecting chronic biomechanical stress around the joint. The constellation of pubic bone stress and joint injury would lend support to many authors’ speculation on patterns of muscle fatigue, overuse, and overload as the cause of injury around the pubic symphysis (26).
For a clinical diagnosis of pubic symphysis joint injury, there should be tenderness directly over the pubic symphysis. Often, the adductor origins and musculotendinous junction of adductor longus may be the area of pain. With flexion and abduction of the hip, the examiner can more easily localize the pain through careful palpation of the adductor longus origin, the pectineus origin along the superior pubic ramus, and the gracilis at the inferior pubic ramus. Patients may initially have pain with resisted hip adduction when the patient is lying on their side (27). Local anesthetic injection into the pubic symphysis can be used to confirm the diagnosis and this can be done either by palpation or using guided localization using ultrasound or fluoroscopy.
A plain radiograph of the pelvis should be the initial investigation. Although early radiographs may be normal, erosions or progressive decalcification follow until a destructive or lytic phase is apparent. Moth-eaten rarefaction may continue with a U-shaped area of loss of bone and cartilage formed. This phase lasts 4 to 6 weeks, although it may be 8 to 12 months before regenerative changes are seen (28). When reviewing plain x-rays of the pubic symphysis the physician should also be aware that growth changes are not complete until around 23 to 25 years of age. This may lead to some confusion over the clinical significance of the radiologic appearances.
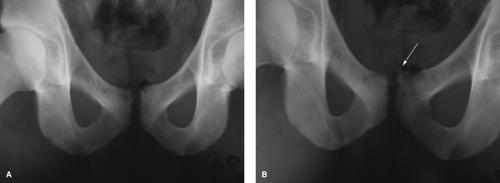
Plain x-rays of pubic displacement on flamingo views have been used to define instability at the pubic symphysis, with a gap greater than 2 mm used to define vertical instability (29) (Fig. 61.6). Triple phase technetium-99c bone scan can used for investigation of pain and is also useful for excluding pelvic stress fractures (30). Magnetic resonance imaging (MRI) with a specific protocol for athletes with groin pain includes an initial sequence surveying the entire pelvis, followed by both fat-suppressed and fluid-sensitive and nonfat-suppressed anatomic sequences and imaging of the joint in the coronal, axial, and sagittal planes (31). Abnormalities commonly seen include parasymphyseal edema, increased signal at the anterior cortex of the pubic body, erosions and cysts at the pubic joint, increased signal within the disc, hypertrophy of the superior pubic ligament, a secondary cleft sign, adductor origin and musculotendinous changes, disruption of the
rectus abdominis/adductor aponeurotic plate, muscle signal changes in the rectus abdominis or adductors, inguinal hernia, and hip joint changes (Fig. 61.7).
rectus abdominis/adductor aponeurotic plate, muscle signal changes in the rectus abdominis or adductors, inguinal hernia, and hip joint changes (Fig. 61.7).
 Figure 61.7. A T2 fat-suppressed coronal image of a stress fracture at the right pubic symphysis (white arrow). |
A conservative treatment program is recommended initially. This algorithm should include a specific exercise program with a focus on stability exercises involving the leg demonstrating the instability on flamingo view x-rays. Although the prognosis of osteitis pubis is usually reported to be excellent, the return to sport rate varies from 14% to 100% (32). In recalcitrant cases surgical fixation can be considered (33).
Muscle Overuse Injuries
Injuries to the anterior muscles of the hip in adults may be seen as part of the epidemiologic progression of the apophyseal avulsion injuries in adolescents. As the growing skeleton undergoes the normal process of ossification of apophyses, the strength of these bony protuberances exceed that of their originating and inserting musculotendinous units. As a result, similar mechanisms of injury transmit abnormal forces to the relatively weaker tendons in the adult, leading to different sites of injury than affect younger patients.
Muscle strains are the most common injuries about the hip and groin resulting from athletic competition (1). Specifically, structures that cross two joints, such as the rectus femoris, iliopsoas, and sartorius, are among the most frequently injured as a result of the tendency toward eccentric contractions (34). The myotendinous junction is the most common site of injury, though the muscle belly injuries can occur as well (1,34,35,36,37). One classification system for quadriceps strain injuries has been applied to strain injuries in other muscles (37). In this system, a grade 1 injury represents a tear of limited number of muscle fibers. Grade 2 injuries refer to the tearing of a moderate number of fibers without disruption of the muscle fascia. A grade 3 strain involves tearing many fibers as well as part of the fascia. A grade 4 injury is a complete rupture of the musculotendinous unit with disruption of all fibers and fascia. Patients who present with more severe, higher-grade injuries are more likely to suffer through a longer recovery and tend to have poorer long-term outcomes.
Rectus Femoris
Because of its biarticular nature, the rectus femoris is the most commonly injured of the four individual quadriceps muscles (38,39). In addition, the rectus femoris is involved in rapid, forceful contractions, because of a high percentage of type II fast-twitch muscle fibers (40




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree