3 Treatment of Glenoid Fractures and Injuries to the Superior Shoulder Suspensory Complex Injuries to the shoulder girdle can range from clinically insignificant avulsion fractures or partial ligament disruptions, to markedly displaced or comminuted fractures that may predispose to long-term shoulder dysfunction. Scapular fractures are relatively uncommon, comprising ~1% of all fractures,1 and only between 10 and 30% of these involve the glenoid.2–5 Because of the thick protective surrounding muscle envelope, the forgiving multiplanar ligaments, and the recoil of the chest wall, direct high-energy trauma is usually necessary to cause a scapular fracture. The significant energy imparted leads to a high incidence of concomitant head, thoracic, shoulder, and other injuries.4,6,7 These multiple associated injuries often distract the surgeon from the scapular fracture, and these fractures are not always readily apparent on initial survey radiographs. Appropriate clinical suspicion, complete radiographic exam, and a thorough knowledge of the osseous and ligamentous anatomy of the shoulder girdle will allow for appropriate treatment to maximize the chance of a good outcome. The initial evaluation of a patient with a potential glenoid or other shoulder girdle injury is a thorough history. For the multitrauma patient, details of the accident scene by emergency personnel or witnesses may give important clues about the mechanism of injury and level of energy involved, as well as any associated life-threatening injuries. A multisystem screening physical exam should be followed by a detailed upper extremity and neurovascular exam. Injuries to the shoulder girdle may reveal pain with passive or active motion, limited motion, ecchymosis and swelling, or gross crepitus. Visible deformity may be notably absent. When the advanced trauma life support (ATLS) protocol has been completed and the patient is hemodynamically stable, a complete radiographic exam is performed. Plain radiographs must include anteroposterior and lateral views in the scapular plane, as well as axillary and West Point views. Ideally, tangential views of the glenohumeral joint should be obtained to evaluate articular displacement and concentricity of the glenohumeral joint. If doubt exists regarding shoulder stability in a small peripheral fracture, fluoroscopic stress views may be helpful.8 Magnetic resonance imaging (MRI) may also be useful in assessing the critical ligament status in minimally displaced fractures. Additionally, several authors have reported on the use of arthroscopic evaluation and assisted reduction of intraarticular glenoid fractures.9,10 Because of the complex bony anatomy, and the often-overlapping cortical bone on x-ray views, complete fracture anatomy visualization can be difficult. Computed tomography (CT) and three-dimensional reconstructions are particularly useful to understand the multiplanar and multifragmented fractures, as well as articular comminution, both of which may affect surgical indications, surgical approach, or choice of instrumentation.4 Fractures of the glenoid may occur extraarticularly, at the neck at the junction of the glenoid and the scapular spine, or may occur through the articular surface. Intraarticular fractures may lead to shoulder instability acutely, or degeneration of the articular surface chronically. Glenoid neck fractures may involve both translational and angular deformity, and can also lead to chronic pain and weakness due to the alteration of glenohumeral biomechanics. The most frequently used classification for fractures of the glenoid cavity is that proposed by Ideberg11 and further modified by Goss12(Fig. 3–1). Type I fractures are the most common fracture pattern, and involve the anteroinferior or posterior articular margin. These fracture types often occur with a glenohumeral fracture-dislocation, and frequently lead to residual instability of the joint following reduction. Type I fractures are distinct from Bankart-type capsular avulsions seen in pure shoulder dislocations and typically involve a larger fragment due to humeral head impaction rather than a capsular avulsion. In type II fractures, the fracture line is transverse or slightly oblique at the articular surface, and exits the lateral border of the scapula inferiorly. When a significant portion of the articular surface is involved, inferior subluxation of the humeral head may be present. The inferior fragment may be pulled and angled distally by the long head of the triceps tendon. Type III fractures occur following a medially directed force with a cephalad component, and the superior one third of the glenoid fossa is affected. The fracture line courses superiorly and usually exits medial to the coracoid at the superior scapular border, and may follow the epiphyseal scar. The direction of the force vector in these injuries often disrupts the superior elements of the shoulder girdle, and may lead to fracture of the clavicle or acromion, or acromioclavicular (AC) separation. Type IV fractures result from a direct medial force. The glenoid is fractured centrally, and the fracture line extends medially to the medial border of the scapula. Type V fractures involve a type IV transverse fracture component with associated superior or inferior fragments as seen in types II and III fractures. Type VI patterns, added by Goss, are comminuted fractures of the glenoid fossa. Figure 3–1 The classification system of Ideberg and Goss for fractures of the glenoid. Fractures of the glenoid neck frequently occur following direct lateral impact on the humeral head, and may occur in concert with other bony or soft tissue disruptions around the shoulder girdle. When double disruptions of the superior shoulder suspensory complex (SSSC) occur, unique biomechanical issues must be considered. The first consideration when evaluating glenoid neck fractures is the inherent stability or lack thereof, for which associated lesions must be considered. These combination injuries are complex and will be discussed further in a later section. Additional specific factors relative to the glenoid neck have significant implications on treatment approaches, however, regardless of associated injuries. In particular, whether or not the fracture is deemed to be stable, malalignment of the glenoid neck may lead to permanent malunion and can have a detrimental effect on shoulder function. The force vector created by the deltoid during initial abduction is a shear force across the glenoid, which is stabilized by the compressive forces of the rotator cuff across an anatomically positioned glenoid. Alteration of this axis results in conversion of the rotator cuff force to shear in the case of inferior angulation, or in a shortened lever arm in the case of a medially displaced glenoid neck fracture.13 For this reason, operative reduction and stabilization of glenoid fractures with evidence of inferior angulation or medial displacement is recommended.13–17 Measurements of angulation must be derived in relation to the scapular body. Some surgeons have advocated the threshold of 40 degrees of angulation or 10 mm of translational displacement as a surgical indication.3,13,18,19 Despite these empiric recommendations, the clinical evidence supporting these indications is sparse. We have found the glenopolar angle (GPA) a useful tool for this purpose. In addition, several authors have correlated the GPA to outcomes after either conservative or operative treatment.15,17,20,21 To obtain the GPA, an anteroposterior (AP) x-ray of the scapula is obtained. Two lines are drawn: the first between the superior and inferior margins of the glenoid, and the second between the superior glenoid and the most inferior point of the scapular body (Fig. 3–2). The GPA is normally between 30 and 45 degrees, and as the glenoid becomes more mis-aligned inferiorly by the pull of muscular attachments and the weight of the extremity, the angle decreases. When the angle is 20 degrees or less, clinically significant angulation exists and we recommend operative intervention based on this angulation alone. Figure 3–2 The glenopolar angle for assessing glenoid neck fractures accounts for the relative inferior tilt of the articular surface. Normal ranges from 30 to 45 degrees. Less than 20 degrees may be a good indicator for operative intervention. Truly nondisplaced glenoid fractures, which have been adequately evaluated radiographically, may be successfully treated nonoperatively. In these cases, we recommend the use of a sling for comfort, and early dependent passive shoulder mobilization, such as pendulum exercises, to minimize posttraumatic shoulder stiffness. Frequent radiographic follow-up is required to ensure the fracture does not displace. The goal of operative reduction and fixation is to correct bony deformity, to prevent chronic glenohumeral instability, and to restore articular congruity to minimize the risk of degenerative joint disease. Due to the relative paucity of long-term clinical outcome data, strict guidelines for operative indications do not exist. Previous authors have advocated surgical treatment when at least 5 mm of articular displacement was present, or with persistent subluxation of the humeral head,1,4,12,22,23 although these parameters are based on very little scientific data. Instability can be anticipated if at least one quarter of the anterior fossa or one third of the posterior fossa is displaced. The surgeon should not rely solely on the fracture classification to dictate surgical approach and fixation techniques. Each fracture should be evaluated for the optimal fixation construct based on ideal biomechanics, and the surgical approach tailored accordingly. However, the fracture type and location of the major fragments does allow for a general approach to the injury. Type Ia fractures are best visualized anteriorly through a deltopectoral approach, which gives adequate access to the anterior glenoid rim. In type Ib fractures, a limited posterior approach to the glenohumeral joint allows for reduction and fixation of the posterior glenoid fossa with small fragment screws. The remainder of the fracture types (types II–VI) involve medial extension of the fracture into the scapular body, and require wider exposure for anatomic reduction and fixation individualized to the fracture. As a general rule, fractures that exit superiorly may be treated with an anterior approach, and inferior fractures are best treated with a posterior approach. For fractures with superomedial extension, a deltopectoral approach may be adequate to control and stabilize the fragment depending on its size. Due to the posterior position of the posterior border of the acromion, visualization of the superior fragment is usually better through an anterior approach. The deforming forces of the long head of the biceps and the conjoint must be counteracted during reduction. Interfragmentary 2.7- or 3.5-mm screws are used for final fracture stabilization. If plates are necessary for fixation, an anterior approach is suboptimal due to limited options of good bone stock for screw purchase posteriorly. When the fracture line extends far medially, we prefer a posterior approach, often supplemented with an accessory superior approach. This technique involves placing a 4.0-mm Schanz pin in the coracoid as a joystick to facilitate reduction. Screws may then be placed from superior to inferior from the coracoid into the scapular spine (posteriorly) or distally into the stout glenoid neck and lateral body depending of the fracture pattern. The posterior approach for superior or medial fracture extension should involve reflecting the posterior head of the deltoid inferiorly and exposing the supraspinous fossa to directly address the fracture. Care must be taken to expose and protect the suprascapular nerve when performing this exposure, and mobilization of the nerve may be the limiting factor in the extent of exposure. Most fractures with medial or inferior extension require a posterior approach to the scapula to visualize, reduce, and stabilize the inferior fragments through the scapular body. Position the patient in a lateral decubitus position with the affected extremity upward. Make a slightly oblique vertical incision, starting from the lateral one third of the scapular spine, angling slightly medially, and extending distally for 15 cm. The posterior head of the deltoid is then reflected from the scapula, and the interval between the infraspinatus and teres minor is identified laterally. The infraspinatus may be mobilized subperiosteally from the inferior scapular fossa as necessary, taking care to protect the suprascapular nerve on its undersurface. The infraspinatus insertion may be partially released from its tendinous insertion, and later repaired, to increase exposure. A T-shaped capsular incision is then made to expose the articular surface (Fig. 3–3). If visualization and adequate control of all the fracture fragments are not possible through this interval, dissection superior to the spine may allow for complete exposure.
Patient Assessment
Glenoid Fractures
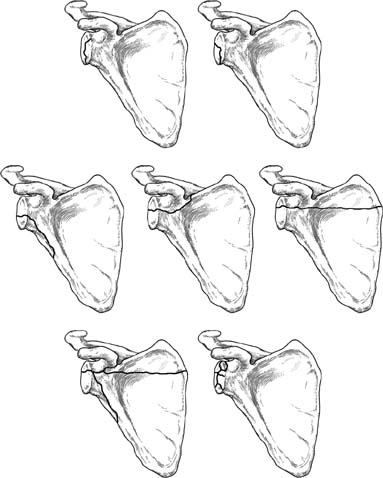
Classification
Glenoid Cavity Fractures
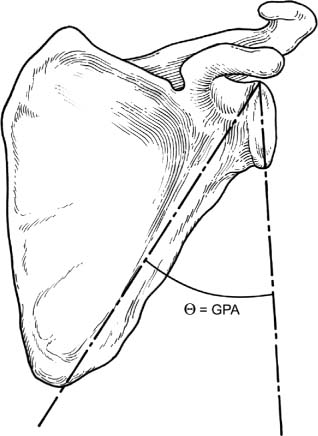
Glenoid Neck Fractures
Treatment
Authors’ Recommended Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree