Treatment of Combined Structural Instability and FAI (Perthes Deformities)
Perry Schoenecker
Thomas R. Lewis
John C. Clohisy
Introduction
Legg–Calvé–Perthes (LCP) is an idiopathic avascular necrosis of the proximal femoral epiphysis of variable extent affecting younger children between the ages of 3 to 10 years (1,2). The histologic response to the acute ischemic process is characterized by osteoblast necrosis, chondrocyte proliferation, creeping substitution, and healing with endochondral bone formation (3). During the inevitable healing process, there is a variable potential for the development of proximal femoral deformity secondary to bony collapse within the epiphysis and/or premature closure of the proximal femoral physis. The extent of involvement and age of patient determines the potential for residual femoral head deformation (4). Treatment of children with acute Perthes disease is designed to contain the hip and minimize permanent femoral head deformity (5,6,7,8,9,10,11). Following healing, most children return to full activity. However, depending on the relative severity of residual deformity (12), patients often note in late adolescence and early adulthood, the onset of hip stiffness, pain, and problematic loss of function.
There has been a recent emergence of a better understanding of the implications of chronic femoral acetabular pathologic impingement which frequently occurs in adolescent and/or young adults who as a child had Perthes disease of the involved hip (13). Accordingly, the goals of containment treatment of acute Perthes disease in childhood should be maintenance of both femoral head sphericity and a congruent hip joint. Stulberg categorized radiographic hip joint outcome morphology of Perthes disease at skeletal maturity into arbitrarily five radiographic femoral head shapes (spherical, aspherical, ovoid and flat, and either congruent or incongruent hip joint types [I to V]) (12).
McAndrew and Weinstein (14), Rowe et al. (15), and recently by Sucato et al. (16) have all reported that notable loss in hip function frequently occurs far earlier in life than what would have been predicted by the Stulberg morphology at the end of growth. In a 20-year follow-up of patients treated in the past with nonoperative methods, Herring et al. reported that surprisingly 22% of Stulberg I and II had Tonnis radiographic arthritis grade of II or III. Fifty percentage of patients with Stulberg types III to V had evidence of arthritis. Of particular concern was the frequent presentation of patients with (Stulberg III) deformity with marked loss of hip function secondary to problematic hip pain in their 20s and 30s, much earlier than previously anticipated. Of note, Stulberg used radiographic evidence of arthritis as an indicator of hip joint disability whereas Herring et al. assessed clinical outcome of residual Perthes disease using a combination of both hip joint function in daily activities and radiographic findings.
Clinical Presentation/Assessment
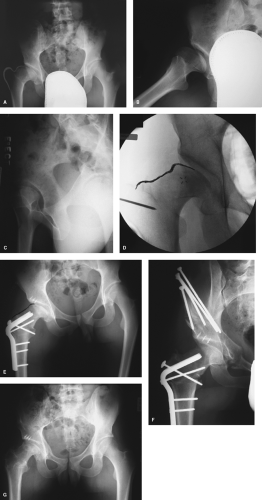
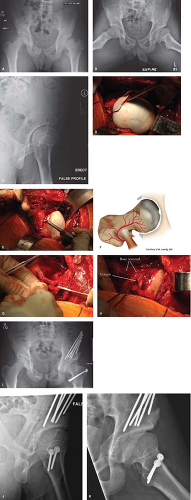
Quite typically, after the resolution of acute Perthes disease in childhood, most patients experience relatively satisfactory hip function often returning to their activities of choice. Later, following an increase gain in body mass noted in adolescence and young adults, patients may begin to experience variably severe problematic hip joint pain, stiffness, and associated limitation in hip function (Fig. 51.1A,B). For some, avoiding high hip stress activities is necessary and may serve to alleviate progression of symptoms. For others, despite restricted activities, bothersome pain often progresses. Patients may be candidates for reconstructive hip joint preservation surgery during which the residual pathomorphologic deformities of a Perthes hip can be comprehensively corrected.
Patients with problematic residual hip joint deformity secondary to Perthes disease typically present because of hip pain that is aggravated with activity. Sitting, walking, and/or running may potentiate the pain. The pain is usually anterior or lateral centered. Patients may give a history of notable limp aggravated with activities. In some patients the limp can be accentuated by a relative hip joint
instability that can develop following acetabular remodeling that occurs prior to skeletal maturation in response to the coxa magna (Fig. 51.1A,C).
instability that can develop following acetabular remodeling that occurs prior to skeletal maturation in response to the coxa magna (Fig. 51.1A,C).
There may be a slight leg-length discrepancy typically with the involved extremity being shorter. Characteristically the range of motion of the involved hip will be restricted in all planes. On careful assessment of motion notably passive hip flexion, internal rotation in flexion, and abduction will be restricted. If possible, comparison to the contralateral hip (typically uninvolved) will help to further identify the restriction of the hip motion characteristic of the problematic post-Perthes hip. The anterior impingement test (flexion with internal rotation and adduction) will be positive. The anterior apprehension test and Patrick test might also be positive for hip joint pain. On occasion the posterior impingement test (passive hip extension with external rotation) may be positive as the circumferentially enlarged femoral head pathologically impinges against the posterior rim of the acetabulum (Fig. 51.2A–C).
Image assessment of the problematic Perthes hip includes essential plane radiographs, typically magnetic resonance arthrogram (MRA), and occasionally computerized axial
tomography (13,17,18,19,20). Femoral head morphology and hip joint congruity are variably assessed on the anterior–posterior (AP) (erect) pelvic, frog-leg, and Dunn lateral views. The lateral head–neck profile is best visualized on the AP radiograph, the anterolateral profile on the 45-degree Dunn lateral view and the anterior profile on the frog lateral views. Relative joint congruity is assessed on all three of these views. The femoral head will be enlarged (coxa magna) aspherical and often assuming a characteristically oval, mushroom, or even a flat shape. The horizontal diameter of the head is often greater than the vertical diameter. The cortical margins outlining the circumferential enlarged femoral head can be seen on the AP radiograph as a “sagging rope sign” (21). This epiphysis will be relatively short, but wide, the neck short, and the greater trochanter “elevated” affecting a relative coxa vara deformity (Fig. 51.1A).
tomography (13,17,18,19,20). Femoral head morphology and hip joint congruity are variably assessed on the anterior–posterior (AP) (erect) pelvic, frog-leg, and Dunn lateral views. The lateral head–neck profile is best visualized on the AP radiograph, the anterolateral profile on the 45-degree Dunn lateral view and the anterior profile on the frog lateral views. Relative joint congruity is assessed on all three of these views. The femoral head will be enlarged (coxa magna) aspherical and often assuming a characteristically oval, mushroom, or even a flat shape. The horizontal diameter of the head is often greater than the vertical diameter. The cortical margins outlining the circumferential enlarged femoral head can be seen on the AP radiograph as a “sagging rope sign” (21). This epiphysis will be relatively short, but wide, the neck short, and the greater trochanter “elevated” affecting a relative coxa vara deformity (Fig. 51.1A).
If Perthes disease occurs early in childhood, acetabular growth and remodeling will occur for the acetabulum to enlarge and assume a contour corresponding to the architecture of the enlarged aspherical femoral head, optimizing joint congruency (Fig. 51.1A). This can be seen on both the AP and false profile views. At times, acetabular remodeling occurs sufficient to render the hip joint structurally unstable (in addition to post-Perthes symptomatic impingement). Relative acetabular insufficiency is best assessed on the erect AP and false profile radiographs. On the AP radiograph the weight-bearing dome of the acetabulum (the sourcil) may be upsloping (>10 degrees, normal 0 to 10 degrees) as measured by the Tonnis angle (17,22). Relative lateral epiphyseal extrusion may exist and the lateral center-edge angle may be decreased (normal ≥25 to 35 degrees). As the acetabulum remodels anteriorly, the anterior center-edge angle assessed on the false profile view will be decreased. If obtained, an MRA confirms the hip joint asphericity and best identifies labral–chondral pathoanatomy. On occasion, a CAT scan may be indicated in surgical planning to further define distortions of the peripheral cortical margins and irregularities in the contours of the subchondral bone of the enlarged femoral head and acetabular contour and relative deficiency.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree