Glenohumeral joint dislocation is a common sports injury, which occurs most frequently from indirect trauma with the shoulder forced into abduction and external rotation, causing an anterior dislocation. It can however occur as a direct injury by landing on the humeral head, and in any direction. The initial treatment requires reduction of the dislocation as quickly as possible by a competently trained practitioner. Ideally, a prereduction radiograph should be taken to exclude any associated fracture, and the limb should be examined for any neurovascular injury, particularly to exclude an axillary nerve injury. Once the shoulder is reduced it should be immobilized in a sling for 3–4 weeks following a rehabilitation program, progressing from initial isometric cuff strengthening whilst immobilized to external rotation and active movement, avoiding abduction and external rotation for 6 weeks. Young athletes have a high recurrence rate after dislocation and often suffer with instability symptoms. As a result, arthroscopy and stabilization should be considered following a dislocation to reduce these risks from 60% recurrence rate to 5% at 2 years (Brophy & Marx, 2009). Consideration should also be given to the possibility of reduced range of movement following stabilization, particularly in open stabilization. Rehabilitation following surgery is likely to take at least 6 months.
Elbow dislocation occurs predominantly posteriorly as a result of hyperextension of the loaded elbow, and often happens during tumbling or on the vault, but female gymnasts are also at risk on the uneven bars when falling on the outstretched arm during flight skills or changing from the low to high rail. It can be a simple dislocation, but often has an associated fracture, commonly the coronoid process or medial epicondyle apophysis, which can become incarcerated during reduction. It can be associated with both nerve and vessel injury and the distal pulse should be assessed. Once reduced, a radiograph should be taken to exclude any associated fractures. Small coronoid fractures and undisplaced radial head fractures can often be treated conservatively with a sling for comfort, but the aim of all treatment following any elbow injury should be early mobilization, as the most debilitating sequelae is stiffness, which is difficult to treat. If the elbow is unstable after reduction, due to bony or ligamentous injury, surgery should be preferred to any kind of immobilization (Athwal et al., 2011).
The interphalangeal joints of the hand can dislocate, if hyperextended after falling, and can be treated with reduction, followed by radiographic assessment for fracture and subsequent protected mobilization. The thumb metacarpophalangeal joint can be injured leading to rupture of the ulnar collateral ligament if the thumb is forced into hyperabduction in activities such as landing on the parallel bars after flight moves. This will require surgical treatment.
Landing on the outstretched hand on any apparatus puts the bones and joints of the carpus at risk of scapholunate dissociation, which presents with obvious deformity of the hand, gross swelling, and requires urgent surgical treatment to restore the anatomy.
Chronic injuries
Growth-related problems
As gymnastics is a sport which is developed during skeletal maturation, and requiring long hours of repetitive training, there is a significant load placed on the growing structures which can be related to chronic problems.
Traction apophysitis
As in the lower limb, but less commonly, repetitive traction on the growing parts of the skeleton, by ligament strain and tendon pull, particularly during times of increased growth, can lead to inflammatory changes, resulting in pain. These most frequently affect the elbow, particularly the medial epicondyle, but occasionally the olecranon. As with other apophysitides, the treatment is conservative with ice, compression, anti-inflammatory medication, and activity modification, whilst addressing flexibility and strengthening as required.
Distal radius physeal stress fracture (gymnast’s wrist)
This condition is mainly seen in females 12–14 years of age with a training routine exceeding 35 hours per week. The condition may be considered at three stages: stage 1 = pre-radiographic, stage 2 = radial physeal radiographic changes, and stage 3 = stage 2 with secondary ulnar positive variance (Figure 11.2).
Figure 11.2 MRI scan of distal radial physeal stress fracture. Note the high signal in the physeal area (arrows).

In stage 1, diagnosis is made on clinical grounds, and gradual return to activities may be possible in 2–4 weeks. In stage 2, X-ray findings of physeal widening and cystic changes exist, and return is prolonged to 2–4 months. In stage 3, concern for ulnar abutment symptoms and subsequent symptoms apply. No correlation between MRI findings and stages of healing has been found; thus, it is not useful as a prognostic tool.
Early closure of radial physis
Experiments have shown that in a wrist with the arm in neutral rotation 80% of the load is transferred though the radius and 20% though the ulna (Albanese et al., 1989). Forearm supination produces a relative negative ulnar variance, forearm pronation produces a relative positive ulnar variance. A wrist loaded with the forearm in supination produces an increase of load transmitted through the radius. Increased load through the radius may lead to excessive forces resulting in early closure of the physis of the distal radius.
Osteochondritis dissecans
Osteochondritis dissecans (OCD) of the elbow is an idiopathic, localized disorder of the subchondral bone resulting in separation and fragmentation of the articular surface and underlying bone. The first description was by König in 1887, where he thought it was caused by an inflammatory reaction of the cartilage (Edmonds & Polousky, 2013). At present no formal etiology is known, but inflammation does not play a role in the pathogenesis.
It is an increasing cause of elbow pain and dysfunction in the competitive adolescent athlete and can lead to clicking and pseudolocking. It mostly affects the young adolescent athlete involved in high-demand, repetitive overhead, or weight-bearing activities, for example, young male baseball players and female gymnasts.
It should not be confused with Panner’s disease (osteonecrosis of the capitellum), which occurs in mainly male patients younger than 10 years. It may however be the same process with a different course and prognosis.
The process has best been described for throwing athletes. During the late cocking and early acceleration phases of throwing, the elbow is subjected to high valgus stress with distraction forces applied to the medial aspect of the elbow and significant compression and shear forces to the lateral radiocapitellar joint. The extreme, repetitive axial loads in young gymnasts with a frequently increased physiological valgus lead to comparative high loads in these athletes. Repeated radiocapitellar compression on the immature epiphysis from repetitive valgus strain leads to subchondral fatigue fracture. Continued compressive stress leads to ultimate breakdown and fragmentation of the overlying articular cartilage and subchondral bone.
When the subchondral fracture leads to displacement, a subsequent fracture of the overlying cartilage leads to detachment of the fragments resulting in loose bodies.
A subsequent vascular injury to the bone, with a tenuous vascular supply with one or two end vessels to the capitellum may add to the further collapse of the involved part of the capitellum.
Patients complain of pain, first during activities and subsequently during rest. Physical examination sometimes reveals a mild effusion and pain on palpation of the capitellum. Rarely, instability of the collateral ligaments is seen. When an effusion is present there is often limitation of extension.
Radiographic modalities
The classic early findings of capitellar rarefaction, radiolucency, or flattening of the articular surface can be seen on plain radiographs. The typical lesion is located on the anterolateral aspect of the capitellum. Fragmentation with demarcating sclerosis and formation of loose bodies are seen with more advanced lesions. Late findings include radial head enlargement and osteophyte formation.
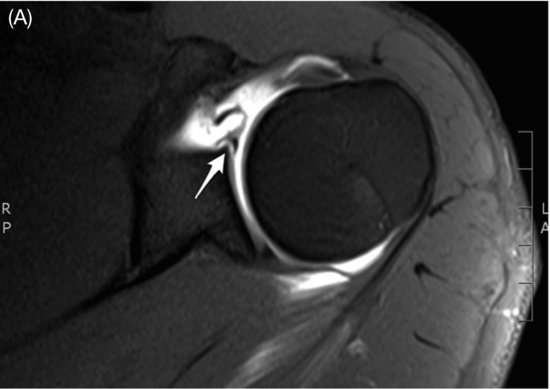
While X-rays are not very sensitive, especially in determining the type of treatment advised, often MRI is added. MRI shows bone changes earlier than a plain X-ray and supplies information about the state of the articular cartilage, vascularity of the fragment (when intravenous gadolinium is used), and stability of the fragment (with the use of intraarticular gadolinium) (Figure 11.3).
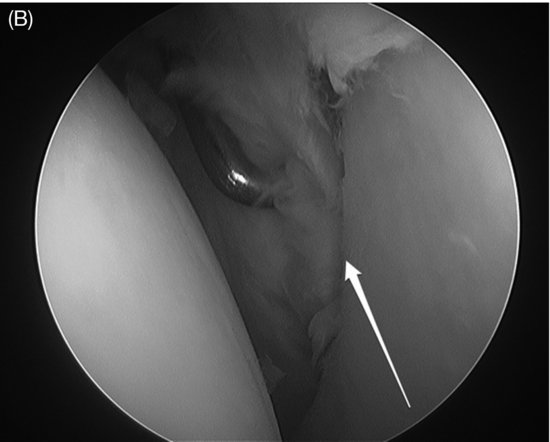
Figure 11.3 Osteochondritis dissecans (OCD) of the elbow. (A) MRI scan. See high signal around the capitellum (arrow). (B) Arthroscopy of defect after excision of loose OCD fragment.


The indications for conservative treatment are radiographic findings of subchondral flattening or radiolucency, a stable fragment as diagnosed with MRI with an open physis of the capitellum. This treatment includes immediate cessation of repetitive stress and, when the ROM is normal, exercises of the elbow. Regular X-rays and MRIs are performed at 6–12 weeks intervals. It typically takes 6 months to confirm healing.
When the fragment is unstable on MRI, or the physis is closed or a loose body is seen on the radiograph, surgery is performed. Most of the procedures can be performed arthroscopically, which enables a full inspection of the joint and leads to a faster rehabilitation. Several arthroscopic treatments are described, and there is no evidence currently for the best treatment. Generally the following guidelines can be used:
- The fragment is still present and the overlying cartilage intact: Either retrograde drilling, using a guide or transchondral drilling can be performed to enhance the vascularity of the bone fragment. Follow-up studies with X-ray or MRI can monitor the healing of the defect.
- The fragment is present but unstable: Fixation with screws, small bone pegs, or other devices can be performed.
- If the fragment becomes detached to form a loose body: The fragment can be removed and the lesion, either treated by drilling or curretting. It is hardly ever possible to replace the loose fragment in the defect.
Alternatively, an osteochondral graft, either from the knee or the rib can be transplanted in the defect. The prognosis of these grafts is not guaranteed and rehabilitation will take more time. Autologous chondrocyte transplantation can be considered, although little data is available on its efficacy for treatment of OCD of the elbow.
OCD of the elbow is not infrequent in young athletes with repetitive loads on the elbow. When diagnosed early and with proper conservative treatment, the athlete can usually resume their activities at the same level. Once surgery is needed, and whatever surgery is performed, the chances of regaining full activities are reduced. Newer techniques hopefully will lead to a better prognosis for the treatment of this disease (de Graaff et al., 2011).
Other common injuries
Shoulder
Shoulder problems often present with pain, which often get labeled with the diagnosis of impingement. Impingement is a clinical sign, rather than a diagnosis, which is caused by irritation of the rotator cuff tendons being impinged upon by unforgiving structures in the subacromial space above (external) or the glenohumeral joint below (internal).
External impingement is divided into primary causes, which are due to outlet obstruction in the subacromial space, and secondary causes, which are due to rotator cuff dysfunction frequently found in conjunction with instability (due to cuff imbalance). Internal impingement is caused by glenohumeral joint instability, such that the cuff insertion gets trapped between the glenoid and the humeral head. This can then lead to pain inhibition compounding the problem by causing cuff imbalance. In gymnasts primary external impingement is rare, as this typically comes on as a degenerative process. Thus, gymnasts presenting with impingement need to have instability and cuff tendinopathy excluded as the underlying cause.
Rotator cuff pathology
The rotator cuff is a group of muscles deep to the deltoid, consisting of subscapularis, supraspinatus, infraspinatus, and teres minor. Together these muscles control the rotation of the shoulder and give control and stability to the glenohumeral joint, where the deltoid provides power. The rotator cuff is susceptible to problems if large loads are put on it as a result of altered biomechanics. Gymnastics is a sport that has a heavy demand of the rotator cuff and the muscles can be worked asymmetrically leading to imbalance of power, which is difficult to address with conditioning exercises. For example, many of the exercises in gymnastics require strength of internal rotation, which if not balanced by training of the external rotators can lead to the humeral head being loaded in internal rotation, which can cause both external (due to reduced subacromial space) and internal impingement (due to relative instability). Superimposed on this impingement is the strength requirement of the disciplines and loading of the joint due to upper limb weight bearing, whilst the cuff tendons are trapped leading to damage not only from physical injury but also ischaemic injury as the blood vessels to the tendons are compressed.
If this continues, the pathology becomes chronic, which is common as the athlete continues to train “through the pain,” and tendinopathy develops, which further exacerbates the imbalance.
Classically, tendinopathy presents as an insidious onset of pain, particularly with certain overhead activities and pain on strength moves of the shoulder. Plain radiographs are frequently normal, but may show some subtle abnormalities of instability, or subacromial changes, and as such are a simple screening tool. Ultrasound scans are operator dependent, and are useful for extraarticular abnormalities, but can miss deep pathology. MRI scanning shows both intra- and extraarticular abnormalities, and with contrast arthrography discovers most pathology.
Rotator cuff tears can occur acutely, after trauma or dislocation, or can develop as the end stage of the tendinopathy process. Acute tears should be picked up by examination of the affected muscle being weak after dislocation or a forced movement during muscle contraction. Chronic tears often present with insidious pain, and weakness may not be apparent as it is considered to be due to the pain. The gymnast will often maintain movement, but certain activities with the arm in abduction become difficult, until eventually they are not possible. This most frequently affects the supraspinatus muscle, but the subscapularis can also be torn, as can the infraspinatus as an extension of the supraspinatus tears.
The treatment of rotator cuff disease should ideally commence with prevention, through good conditioning, and attention to the groups of muscles, which are frequently ignored during training to maintain the balance within the rotator cuff. As the disease process develops into tendinopathy, the treatment should continue with rehabilitation to attain a stable shoulder throughout its range of movement, through stretching any tight capsule and muscle groups, and strengthening any weak groups. This treatment should be developed in conjunction with an experienced physiotherapist.
For rotator cuff tears the only solution in high-demand gymnasts is early intervention with surgical repair, to reduce the risks of propagation of the tear, and subsequent long-term disability with a view to return to pre-injury level.
Shoulder instability
Shoulder instability is a spectrum of disease ranging from recurrent dislocations, through subluxation (partial dislocation with spontaneous reduction), with a feeling of instability, to pain on certain activities typically in abduction and external rotation. The glenohumeral joint is an intrinsically unstable joint. The bony morphology is more like a golf ball set on a golf tee, than a true ball and socket joint like the hip. The humeral head maintains its position in the glenoid through a range of mechanisms both static (bony morphology, labrum, capsulolabral complex) and dynamic (rotator cuff). Both the static and dynamic stabilizers are interconnected through the proprioceptive responses generated by the movements within the shoulder. For example, as the shoulder moves into external rotation the anterior glenohumeral ligaments tighten, acting as a passive limiter (“checkrein”) to further external rotation, but also send a neuronal signal to initiate contraction of the internal rotator subscapularis to stop further rotation. Without this, excessive external rotation may result in anterior translation and eventually dislocation of the humeral head.
Pathological processes, which affect any of the stabilizing mechanisms, can lead to instability of the shoulder. Instability can develop acutely as a result of dislocation (traumatic instability), or can develop in individuals who are susceptible to instability (atraumatic instability). Gymnasts require highly mobile joints, to undertake their disciplines, with a joint capsule and ligament complex that tend to be less tight than in the general population, leaving them at risk of atraumatic instability.
Traumatic dislocations tend to have more obvious underlying abnormalities, such as bony or capsulolabral defects. Those with atraumatic instability can be separated into those with and without structural abnormalities, which may be amenable to surgery. The treatment must be tailored to the individual based on pathology and symptoms.
Clinically the patient describes the shoulder dislocating or coming in and out of the joint. This is also associated with pain and apprehension doing certain activities, typically above shoulder height particularly in abduction and external rotation, although multidirectional instability may describe a feeling of looseness in many positions. Examination should reveal the direction of instability, anterior, posterior, or multidirectional, to aid further investigation. The mainstay of investigations will be through MRI or CT arthrogram, which should identify bony defects on the glenoid and humeral head, labral detachments, capsular abnormalities, and ligament injuries (Figure 11.4).
Figure 11.4(A) Magnetic resonance arthrogram of shoulder with anterior labral tear. (B) Anterior labral tear as seen at arthroscopy.