The Vegetative State
About 20% of survivors of severe TBI remain unresponsive 1 month after injury. After 2 to 4 weeks of unconsciousness, coma evolves into the vegetative state, a condition of wakeful unresponsiveness that is characterized by the presence of spontaneous sleep-wake cycles but absence of cortical activity as judged behaviorally (
154).
Patients who are vegetative 1 month postinjury still may experience substantial recovery, but their chances of doing so diminish over time. Of patients who are vegetative at 1 month, there is approximately a 50% chance of regaining some degree of consciousness within a year and approximately a 28% chance of improving to a level of independence (
155).
Patients continue to emerge from the vegetative state following trauma for at least a year, with rare individuals showing recovery of consciousness even later (little research is available for follow-up periods greater than a year), but nearly all are severely disabled if their emergence is this delayed (
156). The term
persistent vegetative state has been used extensively in the literature, but without consensus on its definition. It has been suggested that this term be abandoned because it confuses diagnosis (vegetative) with prognosis (persistent). Emergence from the vegetative state following nontraumatic injuries (such as cardiac arrest) is far less likely overall, and very few patients emerge beyond 3 months postinjury (
155). This suggests that patients with traumatic injuries complicated by substantial secondary anoxic injury are also likely to have a poorer prognosis than those with uncomplicated trauma.
The following factors have positive prognostic significance for emergence from unresponsiveness: young age, reactive pupils and conjugate eye movements, decorticate posturing rather than decerebrate or flaccid states, early spontaneous eye opening, absence of ventilator dependence or hydrocephalus, shorter time between injury and rehabilitation admission, better scores (within the vegetative range) on the DRS, and more rapid early functional improvement (
157,
158,
159). Unfortunately, no set of prognostic variables is precise enough to guide early clinical decision making. The life expectancy of those who remain permanently vegetative is not precisely known, but one study of patients in vegetative states of mixed etiologies revealed that almost 75% had died within 5 years (
160). Similarly, TBI survivors with severe mobility impairments (though not necessarily vegetative) have a reduced life expectancy due primarily to cardiovascular disease, respiratory disease, choking, and seizures (
161).
The minimally conscious state (MCS) refers to individuals who show some evidence of awareness in the form of visual tracking and/or motor behavior that is nonreflexive and contingent on environmental events (e.g., intermittent following of simple commands, replicable pulling out of tubes) but who
do not consistently follow commands or communicate intelligibly (
162). The MCS, like the vegetative state, can be a transitional state on the way to greater recovery or it can be the permanent functional plateau (
163). Misdiagnosing patients who are in the MCS as vegetative may occur more than 40% of the time, highlighting the need for rigorous diagnostic assessment (
162,
164).
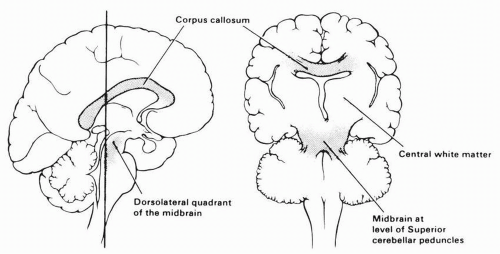
Initial coma in TBI probably reflects disruption of brainstem-alerting mechanisms, often with relative preservation of higher brain structures. Brainstem-alerting mechanisms tend to recover with time, however, resulting in return of the sleep-wake cycle. Thus, a vegetative state of long duration generally includes extensive damage to subcortical white matter in higher brain regions, including the thalamus (
165,
166). Akinetic mutism and the locked-in syndrome may be confused with the vegetative state, but akinetic mutism generally involves damage to the medial frontal lobes, and hypertonia and posturing are absent. The locked-in syndrome generally results from a bilateral pontine stroke, and there is evidence of preserved consciousness and communication through eye movements (
167,
168).
Establishing emergence from the vegetative state can be done clinically, by observing for volitional responses to the environment, such as following commands, orienting visually to salient objects, attempting to remove tubes and restraints, and the like. Essentially, any behavior that is nonstereotyped and that indicates some evaluation of environmental stimuli is evidence of emerging consciousness. A formal and quantitative assessment strategy is an absolute requirement in working with vegetative and minimally conscious patients; without this, team and family members will disagree about whether or not evidence of consciousness is present and whether improvement is occurring. Several standardized scales are available for objectively grading responsiveness in vegetative and minimally conscious patients (
169,
170,
171,
172), although only the Coma Recovery Scale-Revised (
169) incorporates items that explicitly mark the boundary between VS and MCS. In addition, the principles of single-subject experimental design can be used to answer important clinical questions in individual patients, such as whether they can see (
173), follow commands (
174), or reliably use a yes/no signaling system; or whether they respond to therapeutic medications (
175). Assessment should take place repeatedly and at various times of day because patients may respond inconsistently, particularly as they are first emerging from the vegetative state. When family members report observing volitional behavior that has not been witnessed by staff, individualized assessments of the relevant behaviors can be conducted. Family members may overinterpret reflexive or coincidental behaviors, but staff members may fail to elicit the patient’s best performance. Definitive assessment of the vegetative state must await withdrawal of potentially sedating drugs and ruling out peripheral sensory and motor deficits (e.g., blindness, deafness, extensive polyneuropathy) (
164,
176).
The possibility that patients who appear vegetative may have some degree of consciousness that is not reflected in observable behavior has been explored recently using functional imaging and event-related potential (ERP) methods. These studies suggest that there exist patients who are capable of following commands to engage in specific mental activities that can be detected physiologically, even though they cannot produce observable behavioral responses (
177,
178). It is not yet clear how many patients classified as vegetative may be conscious as assessed by more subtle methods, or whether such patients have a better prognosis for the emergence of functionally useful behavior.
Many treatments have been attempted for patients who are in the vegetative state, but none has been subjected to an adequate controlled clinical trial. The pathologic heterogeneity of unresponsive states makes it unlikely that one treatment will help all affected people. Deep brain electrical stimulation of the mesencephalic reticular formation or nonspecific thalamic activating system has been reported to improve the clinical status in some vegetative patients, but small heterogeneous samples and early treatment make it difficult to rule out spontaneous recovery (
179,
180,
181,
182). A more recent report of late recovery of a patient in MCS after thalamic electrical stimulation does not appear attributable to spontaneous recovery (
183). Dopaminergic pharmacologic treatments, including L-dopa, bromocriptine, and amantadine, also have been reported to be of help (
184,
185,
186,
187). Since all these treatments primarily augment ascending arousing influences, they would seem unlikely to benefit patients with extensive cerebral lesions. Coma stimulation (involving the systematic and frequent provision of sensory stimulation to all sensory modalities) has been widely advocated (
75), but studies on it, like those on the pharmacologic agents, suffer from serious methodologic flaws, which have been summarized in review articles (
188,
189). Large, multicenter clinical trials will be needed to definitively assess the value of early treatments designed to improve recovery, because of the confounding and variable effects of spontaneous recovery. However, such trials are fraught with practical and ethical challenges, particularly when they involve a placebo treatment (
190). A number of case reports have been published in which patients who had been vegetative for several years after traumatic or anoxic injuries paradoxically regained consciousness following the administration of a single dose of zolpidem, and whose consciousness could be maintained by repeated dosing of the drug (
191). The mechanism of zolpidem response is currently under investigation. The proportion of VS patients capable of responding to zolpidem is unknown but appears to be small (
192).
In the absence of definitive treatments to alter the prognosis in the vegetative state, the main goals for rehabilitation are to optimize medical stability, preserve bodily integrity, and objectively define the patient’s current sensory and cognitive capacities with measures that can be monitored for change over time (
156,
176). This includes screening for adverse medical events such as undiagnosed seizures, hydrocephalus, and endocrine disorders. Attempts to optimize pulmonary hygiene and maintain skin integrity are also essential. Aggressive treatment of hypertonia and contractures is warranted early because they predispose to skin breakdown, interfere with positioning, and
are costly and time consuming to manage in the chronic stage. Finally, sedating medications should be avoided until the prognosis has declared itself. This includes a variety of antispasticity, anticonvulsant, antihypertensive, anticholinergic, and antihistaminic agents that may have subtle cognitive effects in susceptible patients.
Regular evaluation with a quantitative assessment scale should be carried out. This will reveal subtle improvement that should lead to updated treatment plans, deterioration that should lead to further diagnostic evaluation, or no change, which should lead to family counseling about prognosis and planning toward home or chronic care placement. When a patient remains permanently vegetative, or when a patient remains minimally conscious but has left a specific advance directive, the possibility of forgoing further medical treatments and even life-sustaining fluid and nutrition may be discussed with the family after careful review of local legal guidelines relevant to this area and any institutional policies and ethical guidelines relevant to end-of-life determinations. However, as mentioned, a small number of vegetative or minimally conscious patients may continue to improve over several years, making the determination of permanence more difficult (
193).
Mild TBI
At the other end of the spectrum from unresponsive states is the patient with mild, or minor, TBI (MTBI), which may occur with or without impact to the head. This is generally defined as a TBI with the following characteristics:
Loss of consciousness, if any, 30 minutes or less
PTA 24 hours or less
Initial GCS 13 to 15
No focal neurologic deficit
Negative CT and/or MRI
The initial symptoms of the cerebral injury may be difficult to disentangle from those of the common coincident injuries to the scalp, neck, and peripheral vestibular apparatus (
194). Acute complaints after MTBI typically fall into three symptom clusters (
195):
Cognitive: difficulties with attention, speed of information processing, and memory
Affective: irritability, depression, anxiety
Somatic: headache, dizziness, insomnia, fatigue, sensory impairments
Headaches are the most common and persistent symptom and the symptom that most strongly differentiates those with mild TBI from trauma controls (
196). These symptoms clear within the first few weeks or months postinjury for the majority of patients. Group studies have generally revealed impaired speed of information processing in the early hours or days after injury, but no decrement, or only modest or transient decrement, on neuropsychological measures for individuals with MTBI compared to uninjured controls beyond the first 2 weeks after injury (
197). For a proportion of individuals (15% to 25%), however, difficulties persist and are associated with social and vocational failure seemingly out of proportion to the severity of the neurologic insult (
197). The etiology of these persistent complaints (often termed
postconcussion syndrome, PCS) has been elusive and remains controversial. Premorbid factors such as substance abuse, psychiatric disorder, and age have been implicated but do not explain all cases of persistent disability. The presence of other stressors, preinjury psychological problems, being a student or being in a demanding occupation, being injured in a motor vehicle accident and/or having neck or back injury have also been associated with poorer outcomes (
196,
198). The idea that pending litigation or financial gain accounts for PCS has not been confirmed (
195). In one SPECT study, MTBI patients with unusually persistent disability showed hypoperfusion in the anterior mesial regions of the temporal lobes (
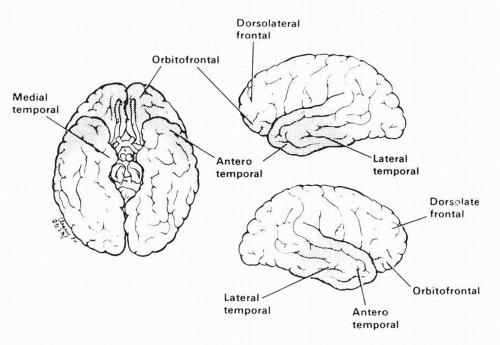
199). There is probably no one cause of PCS; premorbid variables, idiosyncratic neurologic vulnerability, and psychological reactions to acute symptoms may all be found to play roles.
The treatment of MTBI should include patient and family education about the typical symptoms and their time frame, and guidance on how and when to resume preinjury activities. Patients with persistent symptoms may benefit from psychotherapy (
200), pain management protocols (
201), or holistic community reentry programs offering these components along with education, vocational counseling, and group support. Many of the somatic symptoms are responsive to interventions that can be provided by an experienced physical therapist in conjunction with judicious use of medications. Therapeutic interventions may include vestibular habituation exercises (
202), Rocabado exercises (
203), myofascial release, trigger point injections, nonsteroidal anti-inflammatory medications, and muscle relaxants. For more extensive information, the reader is referred to more detailed publications on this aspect of brain injury (
197,
204,
205,
206).
Prompt diagnosis and treatment of “concussion” in sports related injuries has received increased public awareness. Practice parameters have been established by a subcommittee of the American Academy of Neurology and recommendations were also derived from the Second International Conference on Concussion in Sport (
207,
208). A Standardized Assessment of Concussion was developed to provide a sideline evaluation that could be performed by nonphysicians (
209). Computerized neuropsychological tests have been developed for more standardized evaluation and to provide baseline data to which subsequent postinjury data can be compared (
210,
211).
TBI in Children and Adolescents
Children and adolescents are a high-risk group for TBI, with etiologies varying by age group. Falls and child abuse are overrepresented among infants and toddlers, accidental injuries and motor vehicle accidents in school-age children, and injuries due to violence and risk-taking behavior among adolescents.
The management and sequelae of TBI in children and adolescents are very similar to those of adults, but there are a number of issues that are specific to children. On the
one hand, it may be challenging to disentangle neurological recovery from normal growth and maturation. On the other hand, young children may appear to have minimal deficits after TBI, since the skills expected of them are minimal, only to reveal increasing developmental lags as they mature. Because “independence” is not expected of healthy children, many children with TBI are sent home without rehabilitation services, with their parents providing the assistance needed to function safely (
212).
Although it has been estimated that 20,000 children and adolescents reenter school each year with significant disabilities related to TBI, surveys of special education services estimate that only about 12,000 of the more than 5,000,000 U.S. special education students receive services due to a TBI (
213). This discrepancy may have several sources. Children already receiving special education services, particularly those with ADHD, are overrepresented among those injured, and they may retain their original etiology’s label; children may “grow into” their educational disability without the educational system recognizing their prior injury; and some school systems keep records by educational needs rather than etiology (
212,
213). Policy recommendations for improving special education services for this population have been published (
213).
Problems with attention and concentration appear to be among the most frequent sequelae of TBI in children, as they are in adults, occurring in up to 50% of survivors, although as many as 19% of those injured carried a premorbid label of ADHD (
5,
36). Learning and memory difficulties are also relatively common in those with severe injuries (
5). Language impairments have also been reported in children injured in the preschool years (
214). In children with severe TBI, injury to the frontal lobes may result in executive dysfunction (
215). In general, many children with mild injuries make a good recovery. Children with severe injuries show the most persistent cognitive impairments, with those injured prior to age 8 showing less recovery than those aged 8 to 12 years (
5). This is not consistent with the premise that younger children show increased cerebral plasticity in the face of injury, but rather suggests there are periods of increased vulnerability (
216). TBI may also have important effects on emotional adjustment in children and adolescents, with depression, dysthymia, and anxiety disorders among the most common new problems (
36). In a study of college students with a history of mild TBI, intellectual impairments were not found, although the students with prior TBI had increased levels of subjective distress in several subscales of the Symptom Checklist-90—Revised (
217).
Family function also has a significant influence on outcome following pediatric TBI (
4), and there is also reason to be concerned about the impact of the child’s injury on the family. In particular, it has been suggested that siblings of children with TBI-related disability may experience adverse impact themselves, including greater psychopathology, depression, or reduced emotional well-being and more negative relationships (
218).
The preponderance of data suggests that pediatric TBI is underreported and underrecognized in its importance. A high proportion of children with a history of TBI are likely to present with educational special needs, cognitive problems, and psychological/behavioral problems. The fact that some of these children had such problems premorbidly, coupled with the delay between injury and appearance of the problems, may contribute to their underrecognition. Thus, it appears crucial that children with significant TBI be identified and tracked so that the relevance of their TBI to future problems and needs does not go unnoticed.
TBI in the Elderly
As discussed previously, the incidence of TBI is high among the elderly, with up to 86% of TBIs in those over 65 due to falls (
219). Although mortality at a given level of severity is higher among the elderly than among younger individuals, there is also some evidence to suggest cognitive impairments are more severe and functional outcomes poorer, in those who are older (
127,
220). Considerable controversy exists about the prognosis for functional recovery among elderly survivors, due to the fact that many older patients with TBI were already suffering from functional decline at the time of the injury, and to the fact that those elderly patients admitted to rehabilitation facilities are a highly selected group. Research that avoided this selection bias by enrolling elderly patients in acute care, found that GOS scores of moderate disability, or good recovery never occurred in those with GCS scores less than 11 (
221). This was true even among the subgroup with mild original injuries and subsequent deterioration to lower GCS scores. Though it appears likely that the functional prognosis for elderly patients is, indeed, worse than for younger ones, there is also a concern that this may contribute to a self-fulfilling prophecy, in which elderly survivors of TBI are not given the same rehabilitation opportunities as their younger counterparts.
Understanding the rehabilitation problems and needs of the elderly presents some of the same challenges as those seen in the pediatric population. In a retired population, what are the appropriate standards for community integration? If the normal developmental sequence is for an increasing prevalence of disability and need for assistance with aging, how does one assess the outcome of the rehabilitation process against this moving functional target? But, unlike children with TBI, whose parents are already in the role of caregiver, elderly survivors of TBI may have few support options. A spouse may already have died or be too frail to provide the necessary care, and adult children, if any, may be unwilling or unable to provide sufficient assistance. In the absence of family and community supports, therefore, a nursing home destination may seem to be a foregone conclusion, further eroding optimism about the cost effectiveness of aggressive rehabilitation interventions.