Transverse Plane Digital Deformities
Michael S. Downey
Michael C. McGlamry
Sarah A. Spizzirri
Until recent years, discussion of the transverse plane deviation of lesser digits was given nothing more than a cursory mention in the literature. Whether this resulted from limited observation or oversight, unwillingness to describe a condition that was poorly understood, or overshadowing by the more common sagittal plane contracture and subluxation of the toes can only be speculated. Fortunately, this condition is now readily recognized as a significant deformity that can not only be debilitating to patients but also be refractory to treatment. The goal of treatment is to produce a less painful, more rectus digit with reproducible, dependable, and longlasting results.
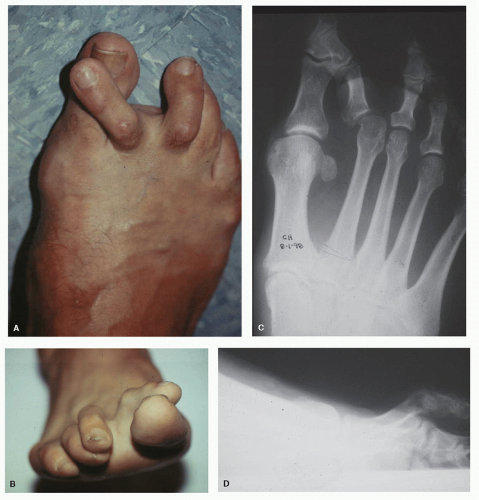
In this chapter, transverse plane digital deformity is defined as the medial or lateral deviation of the longitudinal axis of the proximal phalanx compared with the longitudinal axis of the metatarsal both clinically and radiographically (Fig. 20.1). This condition most commonly affects the second digit with medial deviation at the metatarsophalangeal joint (MTPJ), and this deformity is referred to as the “crossover second toe” (1). Even though transverse plane digital deformities are most frequently seen in the second toe, other rays are often affected (Fig. 20.2).
Although transverse plane deformity of the lesser MTPJ is now well documented, its etiology is not clearly understood and its treatment is not universally agreed upon. In recent years, many articles have suggested potential causes and proposed treatment options. This chapter reviews the currently popular ideas for the etiology, evaluation, and treatment of this still developing and very challenging clinical pathology.
ETIOLOGY
The exact etiology of a transverse plane digital deformity is often difficult to identify and is likely multifactorial. Whatever the cause, the linking element between these factors is damage to the lesser MTPJ capsule, collateral ligaments, and/or plantar plate (PP). Trauma has been implicated as the most frequent underlying cause of this condition, but a focal initiating incident is rarely identified. More commonly, repetitive microtrauma is credited for causing the deformity. Branch (2) and Coughlin (1) correlated high-heeled or narrow-toed shoes with chronic hyperextension or transverse plane forces at the MTPJ that destabilize the joint over time. Not surprisingly then, the incidence has been noted to be greatest in women over the age of 50 (2,3).
Biomechanically, a long or plantarflexed metatarsal, a structurally or functionally short adjacent ray, or the presence of a previous stress fracture of an adjacent metatarsal can lead to increased mechanical forces through the MTPJ and the potential for inflammatory synovitis of the joint (4). Inflammatory synovitis, in turn, may cause rupture or attenuation of the collateral ligaments, capsule, and/or PP, creating a clinically evident transverse plane digital deformity. Johnson and Price (5) recognized that a foot with a vertical oblique midtarsal joint axis creates a medial pull of the flexor digitorum longus tendon inserting into the second digit, thus leading to medial deviation. Close apposition of the metatarsal heads, as in metatarsus adductus, may also play a contributing role in the development of transverse plane deformities (6,7).
When hallux valgus deformity is present, medial deviation of the second digit is easier to explain (Fig. 20.3). With the first metatarsal relatively displaced medially, significant tension is applied to the sesamoid apparatus. The deep transverse intermetatarsal ligament receives medial pull from the sesamoid apparatus, which, in turn, causes medial subluxation of the second MTPJ capsular structures and PP. As the PP shifts medially, it carries with it the flexor tendons. As this imbalance proceeds, the first dorsal interosseous muscle and lumbrical muscle gain mechanical advantage and contribute to the adduction deformity. Over time, the medial second MTPJ structures contract and the thicker lateral structures stretch. Miller noted a similar process associated with a short first metatarsal or a short adjacent lesser metatarsal (8).
Numerous iatrogenic causes have also been associated with transverse plane digital deformities. Due to the presence of several important structures in a confining space, inadvertent injury to an interosseous tendon (IT), the collateral ligaments, or the PP intraoperatively can produce medial or lateral deviation of a lesser digit (9,10). Following the amputation of a digit, adjacent toes have been observed to transversely deviate secondary to loss of the neighboring digit’s “buttressing effect” (11).
Anatomic considerations possibly predisposing the second digit to deviation include an anomalous tendon described as running medial to the extensor digitorum longus tendon and inserting into the base of the proximal phalanx dorsomedially, thus creating a pull not only in the transverse plane but also in the sagittal and coronal planes (12). Also important to note is the shape of the plantar metatarsal head. The lateral plantar condyle is larger than the medial condyle, thus making it easier for the flexor apparatus, once injured, to translocate medially (5).
Inflammatory joint disease and nontraumatic synovitis have been offered as causes of MTPJ deformity in the transverse plane (13). Inflammatory conditions such as rheumatoid arthritis, psoriatic arthritis, Reiter syndrome, and nontraumatic synovitis can cause synovial tissue hypertrophy with eventual joint distention and later disruption of joint capsular and ligamentous structures. This can ultimately result in a transverse MTPJ deformity. Typically, these deformities begin as a
subtle medial or lateral deviation of the digit at the MTPJ. Yu and Judge (14) coined the term “predislocation syndrome” to describe the acute, subacute, or chronic inflammatory condition of a lesser MTPJ, which they felt was a precursor to a lesser MTPJ dislocation.
subtle medial or lateral deviation of the digit at the MTPJ. Yu and Judge (14) coined the term “predislocation syndrome” to describe the acute, subacute, or chronic inflammatory condition of a lesser MTPJ, which they felt was a precursor to a lesser MTPJ dislocation.
EVALUATION
Evaluation of the transverse plane digital deformity includes the standard history and physical examination. Of particular importance are any history of prior inflammatory joint
conditions, history of metabolic disease, past surgical history, and history of any local trauma to the involved area. Careful evaluation should include inspection and palpation, evaluation of the local tissue temperature, active and passive range of motion evaluation, stance evaluation, and radiographs.
conditions, history of metabolic disease, past surgical history, and history of any local trauma to the involved area. Careful evaluation should include inspection and palpation, evaluation of the local tissue temperature, active and passive range of motion evaluation, stance evaluation, and radiographs.
Of specific interest, especially in the early stages of this problem, are localized edema and calor in the flexor tendon sheath or PP at the base of the involved digit or in the joint area. With a local increase in temperature or edema, an early joint problem can often be suspected, even if deformity is not yet apparent. Similarly, fairly significant tenderness is often appreciated with palpation of the base of the proximal phalanx and plantar flexor plate area at the MTPJ level. In the visual absence of deformity, these findings can suggest problems that may ultimately result in deformity.
Neuritic symptoms may often be present and the diagnosis of an interdigital neuroma must be differentiated from a transverse plane digital deformity. Patients with interdigital neuritis often complain of pain radiating into the toes, have pain more localized to the interdigital space than the MTPJ, and have greater pain with Mulder compression technique (15). A diagnostic injection of local anesthetic into the joint will typically help the deviated MTPJ problem, but not the interdigital neuritis (16).
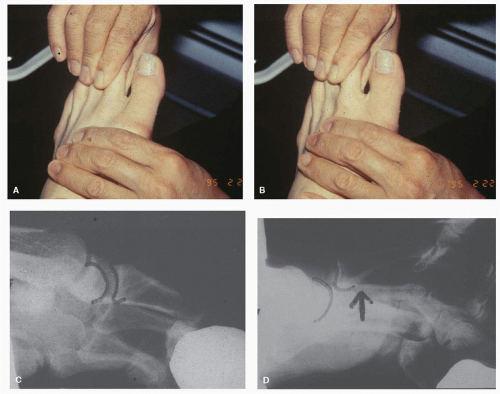
Gentle, passive range of motion evaluation should show an accentuation of the deformity at the dorsal end range of motion as might be seen with a trackbound hallux valgus deformity. This is of particular interest since the primary underlying pathologic force with lesser MTPJ transverse plane deviation seems to be dislocation of the flexor apparatus and PP. Additionally, passive range of motion examination may confirm any abnormality in the quality or quantity of motion. Poor quality of motion or crepitus and/or decreased joint motion might be produced by an articular defect associated with local trauma, such as transient dislocation with cartilage damage at the time of injury or relocation. Passive range of motion examination may also include the Lachman test (4,17), dorsal drawer test (18), or vertical stress test (19) of the lesser MTPJ. These tests are similar and are performed with the metatarsal immobilized firmly in one hand and the proximal phalanx held firmly in the other hand with approximately 20 to 25 degrees of dorsiflexion at the MTPJ (i.e., longitudinal axis of the proximal phalanx relative to the longitudinal axis of the metatarsal) (Fig. 20.4). A vertical shear force is then applied with an attempt made to
vertically dislocate the proximal phalanx at the MTPJ. Deland et al (19) defined a significantly positive test as more than 2 mm of dorsal displacement.
vertically dislocate the proximal phalanx at the MTPJ. Deland et al (19) defined a significantly positive test as more than 2 mm of dorsal displacement.
Active range of motion will often suggest dislocation of the flexor apparatus and PP as the toe will medially or laterally deviate with flexion of the MTPJ. McGlamry (20) found that eliciting the plantar Babinski reflex by stroking the plantar surface of the foot would result not in pure plantarflexion of the toes, but limited flexion along with medial or lateral deviation in patients with transverse plane deformities. Limited motion or pain with either passive or active range of motion can also suggest joint damage or arthritis.
The stance examination is particularly important, as many of these deformities are not evident, especially in the early stages, on non-weight-bearing examination. If weight-bearing evaluation is not possible, the stance position can be reproduced with the use of the Kelikian push-up test (i.e., manual loading of the PPs by applying pressure to the plantar aspects of the metatarsals). Note should be taken of the transverse plane position as well as sagittal plane deviation of each of the lesser rays. Sagittal plane contracture is often associated with the transverse plane deformity. A gap will often be noted between toes when an isolated transverse plane deformity is present. In other instances, all of the toes will deviate in the same direction (see Fig. 20.2). Often with transverse plane deformity, there is concomitant sagittal plane deformity, and the toe will deviate medially or laterally during stance and also will not purchase the weight-bearing surface.
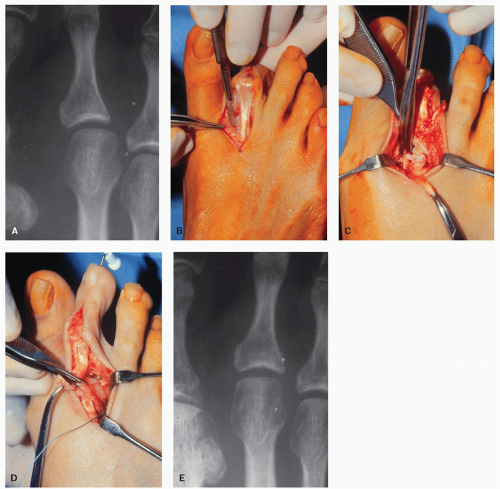
Radiographic evaluation should be undertaken in relaxed stance. For obvious reasons, non-weight-bearing radiographs may not adequately reflect the degree of the deformity. Though no standard angle has been reported in the literature, it is often helpful to record the “digital deviation angle” or the angle created by the longitudinal axis of the proximal
phalanx of the toe and the longitudinal axis of the metatarsal shaft (see Fig. 20.1C).
phalanx of the toe and the longitudinal axis of the metatarsal shaft (see Fig. 20.1C).
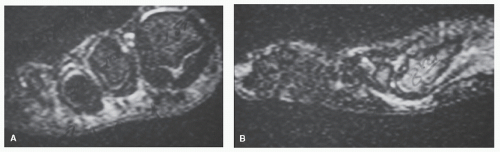
Other diagnostic imaging techniques have also been described, but are usually unnecessary as the clinical findings typically provide the clinician with the means to make the diagnosis. In the early stages of the process, when suspicion of the condition is present without significant clinical deviation of the MTPJ, magnetic resonance imaging (MRI) may be helpful in cases where the diagnosis is equivocal (21,22 and 23). MRI will show gross pathologic changes within the tendon apparatus, joint, and/or PP, but will also demonstrate increased signal intensity even prior to any rupture or displacement of the flexor apparatus (Fig. 20.5). Arthrography has also been noted to demonstrate partial or complete damage to the PP as well as small defects in the joint surfaces (21). More recently, several investigations have shown that musculoskeletal ultrasound can be used to assess the lesser MTPJ joint structures and help differentiate PP pathology from interdigital neuromas and other sources of forefoot pain (24,25,26,27 and 28). Due to the dynamic nature of ultrasonography, it may actually become the modality of choice for such clinical assessments in the not too distant future.
The early condition which potentially leads to transverse plane deviation of the digit has been well described by Yu and Judge (14) as “predislocation syndrome.” Coughlin (17) similarly described various stages of crossover deformity: stage I, synovitis and mild deformity; stage II, dorsomedial deviation; stage III, overlapping of the hallux; and stage IV, frank MTPJ dislocation. As with many conditions early understanding and diagnosis may be the key to the most successful treatment.
TREATMENT
CONSERVATIVE TREATMENT
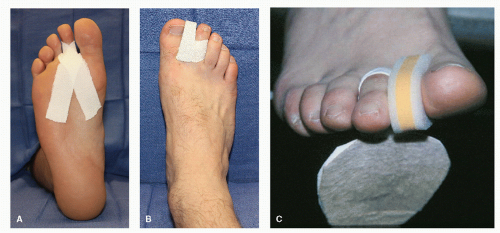
An appropriate trial of conservative care should be attempted prior to considering surgical intervention. This is especially true when a patient presents in the early stages with capsulitis-type symptoms and is diagnosed with “predislocation syndrome.” In milder or acute cases of transverse plane deviation of the digits or in cases of “predislocation syndrome,” treatment with digital strapping and taping, balance padding, and oral anti-inflammatory agents (nonsteroidal and steroidal agents as needed) may completely relieve the patient’s symptoms. Extra-depth or extra-width shoes and toe splints are used for subacute or more chronic conditions. The authors’ preference for initial treatment consists of mechanical therapy with a submetatarsal buildup to offload the affected metatarsal and MTPJ or a forefoot sling pad (i.e., Budin splint) or strapping that realigns the affected MTPJ directly and offloads the toe joint indirectly. If a hallux valgus deformity is present, a toe spacer is also used between the hallux and second toe (Fig. 20.6). In conjunction with the mechanical treatment, nonsteroidal anti-inflammatory drugs or oral steroids (e.g., Prednisone taper) are administered to reduce the associated capsulitis. A small number of carefully placed corticosteroid injections are employed by many clinicians as well, although this is not without some controversy, as others feel such injections can aggravate the deformity. In longer-standing or more severe cases, conservative treatment is seldom effective at alleviating a patient’s symptoms and surgery is often required. Also, if conservative treatment is attempted and the deformity continues to progress or is persistently painful, surgery is indicated (29).
SURGICAL TREATMENT
A plethora of surgical options have been described from simple percutaneous capsulotomy to complex repair and rebalancing of the joint with or without osseous procedures. The specific procedures required should be based on the underlying etiology, degree of deformity, duration of symptoms, and response to past treatment.
Incisional Approaches
Transverse plane digital procedures can be performed successfully under monitored anesthesia care with a local block, general anesthesia, or regional anesthesia. Hemostasis can be obtained with an ankle or mid-thigh tourniquet, with local anesthetics containing epinephrine, or with local hemostasis measures alone. Some surgeons have expressed concern of
extensor contraction secondary to the application of an ankle tourniquet. If that is a concern to the surgeon, the procedure can be performed with a mid-thigh tourniquet or without any tourniquet applied.
extensor contraction secondary to the application of an ankle tourniquet. If that is a concern to the surgeon, the procedure can be performed with a mid-thigh tourniquet or without any tourniquet applied.
Since transverse plane digital procedures are often executed with other procedures, several incisional approaches are acceptable. Described dorsal incision approaches include linear incisions centrally located over the involved metatarsal or the associated intermetatarsal space (30,31), curvilinear incisions again located over the involved metatarsal or intermetatarsal space (11,32,33 and 34), a small “smile” incision (35), a “serpentine” incision (5), or a small transverse incision at the osteotomy site (35). Some of these incisions can be extended both distally and proximally depending on the procedures being performed. Due to the progressive nature of skin healing, incisional scar contractures are often not seen until several months after the surgical procedure and this possibility should be considered preoperatively (32,36). A plantar incision may be used when direct PP repair is planned. However, certain metatarsal osteotomies may be difficult to perform through a plantar approach and a painful, thickened, or hypertrophic plantar scar in a weight-bearing area is always a concern. A dorsal curvilinear incision is recommended not only because of increased exposure secondary to the design of the incision, but also because of the decreased tendency for contractures across the MTPJ which can lead to not only poor patient satisfaction but also possible reoccurrence of the original deformity. Dependent on whether an isolated osteotomy is being performed, the incision can be placed directly over the MTPJ or over the associated intermetatarsal space if adjacent digits are also being addressed.
Soft Tissue Procedures
Even though the emphasis of this chapter is on metatarsal osteotomies, the importance of appropriate soft tissue release and repair cannot be overemphasized. The goal of soft tissue procedures is to realign the PP under the metatarsal, repair damaged joint structures, release contractures across the MTPJ, and create a stable soft tissue envelope. The soft tissue procedures utilized depend on the other deformities present, including whether the deformities are rigid or flexible. Soft tissue procedures for the correction of transverse plane digital deformities have been described including percutaneous or open capsulotomy and capsulorrhaphy, extensor tendon lengthening or tenotomy, PP release, relocation and repair, and tendon transfer. Oftentimes, these soft tissue procedures will be performed in a sequential or “stepwise” manner.
Simple capsulotomy of the MTPJ has been described (37), but is rarely effective for complete correction of the transverse plane digital deformity. This becomes obvious when one understands the etiology of the deformity. Simple capsulotomy will not realign the displaced flexor apparatus. Capsulotomy would only be effective for full correction, if an acute traumatic episode causing rupture of the joint capsule healed with significant medial or lateral scar contracture. In such a circumstance, release of the capsule on the side to which the toe is deviating might be successful in correcting the deformity. More often though, capsulotomy is used in combination with other procedures to correct the deformity.
Similarly, capsulorrhaphy of the MTPJ and extensor tenotomy have been described, but are rarely indicated as isolated procedures for the correction of the transverse plane digital deformity. Capsulorrhaphy is performed on the side opposite the transverse plane deviation. For example, in the medially deviated second toe, a lateral MTPJ capsulorrhaphy may be helpful as an adjunctive procedure in the correction of the deformity. An extensor tendon lengthening or tenotomy can be helpful if the toe is deviating in both the transverse and sagittal planes. Minimal transverse plane correction is achieved with an isolated extensor tendon lengthening or tenotomy.
Release of the PP may be employed as an adjunct in repairing the transverse plane deformity. PP release is performed through a dorsal MTPJ capsular incision with care being taken to protect the articular surface of the MTPJ. The collateral ligament on the side of the joint to which the toe is deviating is then released. The capsule is retracted medially and laterally allowing passage of a McGlamry metatarsal elevator or similar instrument. The joint should be held distracted and the elevator gently inserted to avoid damage to the articular surface. The elevator is then rotated, advancing its leading or cutting edge plantarly and proximally. Experience with this release and instrumentation will confirm to the surgeon the significant adhesion of the PP to the undersurface of the metatarsal in the transverse plane digital deformity and severe hammertoe contracture. Though seldom effective as an isolated procedure, the PP release may prove an important component of the overall repair process in some patients. In the past, many surgeons have felt that once the PP was released, correction could be gained by simply pinning the toe in a slightly overcorrected position and allowing the PP to “scar down” in the corrected alignment. In practice, this did not provide reproducible, lasting correction. This may be due in part to the fact that while the flexor plate may be relocated, in some patients, the long flexor tendon maintains a medial deviation beneath the MTPJ.
Ruch (38) described a partial sectioning of the medial portion of the PP for a medially deviated toe (Fig. 20.7). He reported the procedure worked well for milder cases of transverse plane digital deformity.
Though no specific follow-up reports are noted in the literature, Castellano (39,40) described a direct plantar approach to repair and relocate the displaced PP and flexor apparatus. Ford and associates (18) studied the lesser MTPJ stability provided by both flexor tendon transfer and primary repair of the PP in fresh frozen cadaver specimens, and concluded that primary repair of the PP is a viable alternative to the flexor tendon transfer. To perform a primary repair of the PP, a plantar longitudinal incision is placed directly under the involved MTPJ. Dissection is carried deeply to the MTPJ area. The PP is identified, repaired as needed, and directly sutured in a rectus position. Often a “vest-over-pants” repair technique or the use of adjunctive soft tissue anchors is employed.
Various tendon transfers have also been utilized with varying degrees of success. These procedures would seem to offer the most promise for future nonosseous reconstruction of the transverse plane deviated lesser MTPJ. In 1984, Collins and Collins (11) described a threefold procedure they advocated for correction of a transverse plane digital deformity. Their procedure consisted of the following: (a) sectioning of the short IT on the side of the deviation; (b) dividing and transferring the extensor digitorum longus (EDL) tendon to a more central location at the base of the proximal phalanx; and (c) dividing the contracted extensor sling. Unfortunately, this procedure failed to address the malposition of the PP or flexor apparatus and has not become popular.
Although it is more effective for a sagittal plane MTPJ deformity, the flexor tendon transfer, also known as the flexor-to-extensor transfer or Girdlestone procedure, has been popular as a corrective procedure for a transverse plane digital deformity. For a flexor tendon transfer, the contracted structures on the side of the MTPJ to which the toe is deviated are released through a dorsal incision. Two plantar transverse incisions are then made at the levels of the proximal and distal interphalangeal joints. The flexor longus tendon is isolated and released through the distal incision, and brought out through the proximal incision. The tendon is then split longitudinally, and each end of the tendon is passed dorsally around the medial or lateral sides of the proximal phalanx and sutured together or to the extensor hood apparatus. Care must be taken to pass the tendon slips deep to the neurovascular structures. In a study, which included 6 feet with medial crossover deformity of the second toe, Thompson and Deland (41) reported good success with the procedure. Although these authors concluded that the flexor tendon transfer does not reliably reduce the joint anatomically, they felt it does provide satisfactory pain relief albeit with some joint stiffness.
In 1992, Deland et al (19) described and studied a more anatomic reconstruction of the lesser MTPJ with restoration of the collateral ligaments of the joint with a dorsal or plantar IT (Fig. 20.8). In their procedure, the IT graft is harvested just distal to its musculotendinous junction, and dissected to the level of the PP. Thus, the tendon is left attached to the proximal phalangeal base and PP and freed proximally. A 2.0-mm drill hole is then made 2 to 3 mm proximal and inferior to the lateral epicondyle of the metatarsal. The tendon is then passed through the hole, placed under appropriate tension (i.e., tension significant enough to correct the deformity and yet not compress the joint), and sutured in place. Alternatively, a small bone anchor can be used to accomplish the tenodesis of the tendon to the metatarsal. Deland et al (19) performed their procedure in 10 cadaver specimens and found it provided consistent stability and no restriction of MTPJ motion. To date, their laboratory-proven procedure has not been reported in clinical trials.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree