CHAPTER 50 Transforaminal Lumbar Interbody Fusion
Anterior lumbar fusion was first described by Muller in 1906.1 Evolutions of the technique have included modifications of the abdominal approach to a less invasive, mini-open technique and the use of interbody cages or structural allografts augmented with autogenous iliac crest graft, local bone graft, or, more recently, recombinant human bone morphogenetic protein (rhBMP-2).2–5 Without the augmentation of posterior support, it has been well recognized that there is an increased rate of graft subsidence.1,6 The combination of anterior lumbar interbody fusion with a posterolateral instrumented fusion (360-degree fusion) has been shown to yield fusion rates of greater than 95%.7 Anterior lumbar interbody fusion has significant potential morbidities, however, including potential injury to the great vessels, abdominal hernia, injury to the sympathetic chain with subsequent sexual dysfunction, and thromboembolus secondary to retraction of the artery.8–10
Recognition of the biomechanical advantages of an anterior lumbar interbody fusion augmented with rigid posterior instrumentation led to the development of posterior-only approaches to the disc space to eliminate the approach-related morbidity of anterior interbody fusions. Posterior lumbar interbody fusion was developed to provide access to the disc space via a bilateral posterior approach with retraction of the thecal sac. Posterior lumbar interbody fusion is limited in its use to below the level of the conus, however, owing to the degree of thecal sac retraction necessary. Because of the retraction of the neural elements with posterior lumbar interbody fusion, there is concern for injury to the nerve roots, pain syndromes secondary to injury of the dorsal root ganglion, and cerebrospinal fluid leaks.11
Anterior lumbar interbody fusion via a transforaminal posterior approach (transforaminal lumbar interbody fusion [TLIF]) was first described by Harms and Rolinger in 1982.12 Using a transforaminal approach via osteotomy of the pars interarticularis and inferior articular facet allows for facile access to the disc space with minimal retraction of the neural elements, avoids the morbidity of an anterior approach,13,14 and has a lower complication rate than direct posterior lumbar interbody fusion.11 Accessing the disc space via a posterior annulotomy, approximately 56% of the endplate can be prepared for fusion15 with placement of bone graft and interbody implant. Combined with standard posterolateral instrumentation, decortication, and bone grafting, radiographic fusion rates greater than 90% can be achieved.16 Published outcomes of single-level TLIF and multilevel TLIF are equivalent or better than anterior and 360-degree fusions, with restoration of the disc space height.16,17 TLIF has been shown to result in significant savings relative to anteroposterior interbody fusion, owing in part to the decreased operating room time, less blood loss, and shorter hospital stays.18
Although some degree of restoration of disc space height with TLIF has been documented, the magnitude of restoration has been shown to be less than that achieved via anterior lumbar interbody fusion.19,20 Similarly, longitudinal studies have shown a progressive loss of restored lordosis, as the fusion construct over time tends to drift back to the preoperative sagittal balance. The clinical significance of radiographic differences between anterior lumbar interbody fusion and TLIF is unknown because these radiographic differences have not been shown to correlate to differences in outcome measures.20
Radiculopathy secondary to a foraminal disc herniation is difficult to address adequately from a midline approach and decompression owing to limited access to the lateral foramen. A far-lateral or foraminal disc herniation may be managed with a facetectomy, facilitating a transforaminal approach to the nerve root.21 TLIF may be considered as treatment for a foraminal disc herniation, particularly in the setting of significant loss of disc space height, because one may directly decompress the nerve root with the facetectomy, achieve an interbody and posterolateral fusion, and achieve indirect decompression with increase in the disc space height.
Advances in less invasive spine surgery, mini-open approaches, tubular retractors, and percutaneous instrumentation systems have been applied to TLIF, and minimally invasive TLIF procedures have been proposed to address the morbidity of the posterior midline approach. Preliminary studies have suggested that minimally invasive approaches may result in less blood loss and shorter hospital stays.22–24 These preliminary reports are case series, however, so the results must be extrapolated to general practice with caution. Prospective randomized studies are needed comparing less invasive or minimally invasive TLIF procedures with the standard open midline approach to compare clinical outcomes and radiologic indices (disc space height, graft placement, lordosis, and fusion).
Surgical Procedure
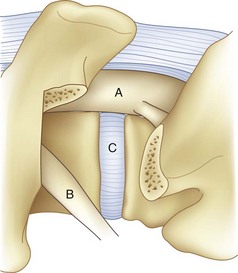
For transforaminal access to the disc space, it is necessary to remove the entire facet joint effectively on one side. This is accomplished by removing the inferior articular process of the cephalad level with an osteotomy through the pars interarticularis. This osteotomy should be performed on the side of greatest neural pathology; the osteotomy through the pars should be done as cephalad as possible to maximize the exposure but with care not to violate the pedicle itself (Fig. 50–1). Before the osteotomy, the ligamentum flavum should be completely freed from the lamina with a curet; particularly in the setting of a revision procedure, removal of the ligamentum and associated adhesions after the osteotomy may prove difficult and increase the risk of incidental durotomy. The transforaminal approach may be done either in concert with a midline laminectomy or with preservation of the spinous processes and midline ligamentous structures. To preserve the midline structures, one first makes the osteotomy up the medial aspect of the ipsilateral lamina, with the second osteotomy across the pars interarticularis as close as possible to the inferior margin of the cephalad pedicle. The inferior articular facet may be grasped with a Leksell rongeur or pituitary and rotated away from the underlying dura, taking care to remove any ligamentous adhesions with a curet.
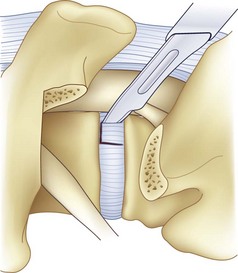
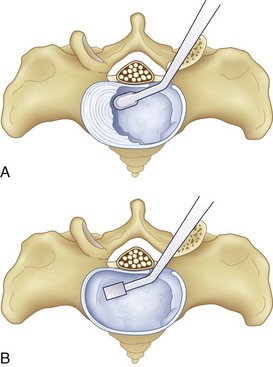
After completion of the surgical exposure of the transforaminal zone as described, a nerve root retractor should be placed medially to protect the thecal sac. With appropriate surgical exposure, only minimal retraction should be necessary as protection against incidental durotomy during the annulotomy. The posterior anulus should be incised widely with a box cut, with care taken to visualize the exiting and traversing nerve roots (Fig. 50–2). After completion of the annulotomy, the discectomy may be started with a pituitary rongeur and curets. A forward angled pituitary is necessary to enter the disc space on the contralateral side of the patient. When removing the disc and cartilage from the endplates, care must be taken not to violate the subchondral bone. Angled curets and chondrotomes should be used to remove the cartilaginous endplate from the far lateral side. A thorough discectomy and endplate preparation are essential, but absolute care must be taken not to violate the anterior anulus or subchondral bone (Fig. 50–3).
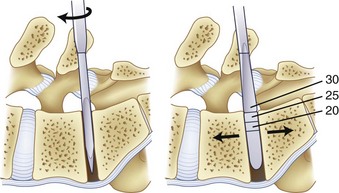
As the discectomy progresses, sequential dilation of the disc space should be accomplished with serial dilators. When impacting the dilators into the disc space, care must be taken to follow the sagittal plane of the interspace to avoid driving the dilator through the endplate, particularly in an osteoporotic patient (Fig. 50–4). If necessary, exposure may be aided by distracting between the spinous processes with a lamina spreader. After distraction, the assistant must hold the lamina spreader to stabilize it because inadvertent dislodgment may place the contents of the spinal canal at risk. The posterior lips of the vertebral bodies may be removed with osteotomes so that they are flush with the concavity of the endplate; if not removed, the interbody implant may be undersized (Fig. 50–5). After dilation to an appropriate size, the trial implant should be placed, with care taken to tamp it appropriately medial and anterior.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree