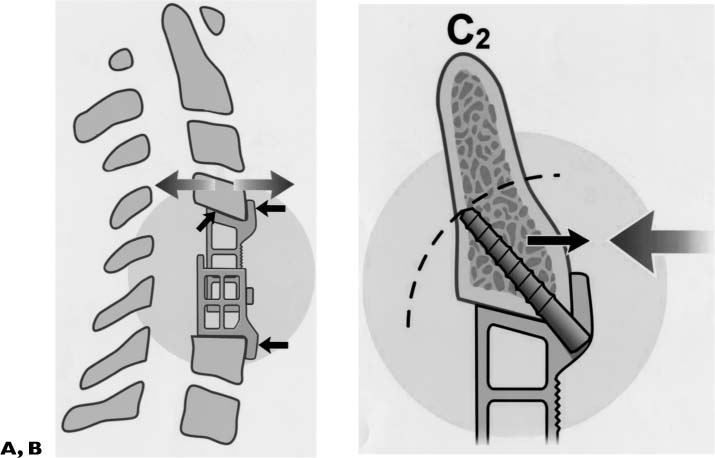
Chapter 36 There are 8 million Americans with osteoporosis in whom 1.5 million fractures are diagnosed each year. Of these, 750,000 occur in the spine. Though most common in postmenopausal women, vertebral compression fractures occur in both sexes, every age group, and all races.1 The risk of fracture for a reduction in bone density of one standard deviation is 10% and is twofold for every reduction in standard deviation beyond. The cost of osteoporosis is great: $14 billion in 1995 alone. Most cases arise in the elderly. Other risk factors include positive family history, poor diet, immobility, alcohol use, smoking, caffeine, use of anticonvulsants or methotrexate, hyperthyroidism, elevated glucocorticoids or steroid use, neoplasm, chronic inflammatory disease, and poor nutrition. Other causes of bone softening should be ruled out, such as osteogenesis imperfecta, osteomalacia, rickets, osteitis fibrosa, and Paget’s disease. Patients present most commonly with back pain, usually of a nonradicular nature. Most cases of osteoporotic fracture are treated with bracing and pain control, but patients with progressive deformity, instability, or loss of alignment may be candidates for vertebroplasty or surgery. Endoscopic or percutaneous vertebroplasty (the injection or instilling of polymethylmethacrylate or other bone substitutes into the vertebra) is a reasonable treatment for preventing further collapse of one or several vertebrae and in some instances for reestablishing vertebral height. However, there are real risks of vertebroplasty, including extrusion of compound with epidural compression of the spinal cord or nerve roots, systemic embolization of particles and consequent death, immune reaction to the injected compound, and infection. When stability, severe pain, or neurological deficit is an issue and when the patient is deemed a reasonable surgical risk, then more definitive surgical treatment should be considered. Posterior stabilization and fusion is appropriate in many cases of instability or severe intractable pain. However, anterior column instability with progressive kyphosis, loss of vertebral height and alignment, ventral compression, or impending compression of the spinal cord or nerve roots might best be treated anteriorly, and vertebrectomy may be the treatment of choice. Similarly, vertebrectomy and anterior column stabilization is often the treatment of choice for metastatic disease of the spine. Metastatic disease of the spine is common; the spine is the most common site for osseous for metastatic deposits, with 5 to 10% of all cancer patients ultimately developing epidural disease. While most patients are treated with palliative radiation and steroids, those with intractable pain, instability, and neuraxial compression are suitable candidates for tumor resection and stabilization.2 Vertebrectomy from an anterior approach is most often preferred as 85% of metastatic disease arises ventral to the spinal cord in the vertebral body. Other indications for surgery include recurrence of tumor after radiation and chemotherapy, patients with solitary lesions where resection may be curative, and patients in which open biopsy is required. There are four major problems encountered with most anterior stabilization devices, particularly when treating soft or osteoporotic bone. First, the “piston effect” or subsidence of the graft or device into the adjacent vertebra, which causes loss of vertebral height. There may be loss of alignment with increased kyphosis, and often persistent pain from microinstability; secondly, the inability to provide inline distraction to safely accomplish reduction of fracture and kyphosis; thirdly, the inability of the construct to engage and incorporate the strongest parts of the vertebra; fourthly, the inability to place the instrumentation in regions difficult to access, such as the cervicothoracic junction and the upper cervical spine. Instrumentation failure occurs commonly in poor-quality bone in consequence to screw pullout, subsidence of construct, and graft failure. Successful fracture reduction, stabilization, and fusion require a strategy that enjoins natural anatomical features into a rigid, load-sharing construct. Four design features of the TPS (Figs. 36–1A,B) exploit the natural anatomical and biomechanical features of the spine, which are permissive to reconstruction of poor-quality bone. The first anatomic feature availing itself to construction is the ventral anterior edge of the vertebra (the “ventral lip” of the vertebra). While the soft cancellous core of the vertebra is incapable of resisting pistoning of a device or fusion substrate, the ventral lip of the vertebral body, hardened through Wolff’s Law, provides an excellent platform for reconstruction. The “boundary effect” of Benzel refers to the ability of the edge of the vertebra to carry a greater load than the softer centrum.3 To avoid pistoning of spacer or graft into osteoporotic bone, the surgeon therefore must incorporate the “boundary” into the construction. The fully integrated flanges of the TPS maintain the position of the spacer at the edge of the vertebral body (Fig. 36–1A) to utilize the boundary effect. The flanges are furthermore load bearing and anatomically contoured to minimize translational movement. A second anatomical feature, the slope of the end plate of the vertebra above, lends itself to bracing the upper end of the graft or spacer. The ventral lip of the vertebra above, which in part covers the disc space, is too often resected by the surgeon to create an inter-space that is more perpendicular to the spine; removing this ventral lip permits the surgeon to more easily place the graft or implant. However, the sloped upper surface of the TPS accommodates this natural feature as a brace to avoid kick out (Fig. 36–1A). The cephalad surface of the TPS device, angled at 15 degrees, conforms to the diagonal slope of the vertebral end plate above. With distraction, this bevel locks the device in place behind the vertebra above, providing the “bracing effect.” A third feature is the relationship of the screws (angled at 45 degrees) to the instantaneous axis of rotation (IAR). The IAR is the axis perpendicular to the plane of motion and passing through a point that does not move for a given motion at a given instant.4 The IAR, or the point around which the vertebra rotates in flexion and extension, lies toward the ventral inferior aspect of the vertebra.4 Altering the rigidity of any spinal motion segment results in a change in the IAR. A rigid, load-bearing device under compression (such as the TPS), placed into the anterior part of a corpectomy defect, changes the point around which the spine pivots.5 The center of rigid load bearing and the IAR thus move ventrally and inferiorly in the upper vertebra and ventrally and upward in the lower vertebra of the construct. Movement in flexion/extension occurs in an arc around each respective IAR. The vector of pullout force, and therefore pullout tendency, is greatest along any tangent to the path of rotation around the IAR. A screw placed perpendicular to the path of movement will see zero pullout force, though shear forces will be maximal. TPS screws are angled at 45 degrees away from the path of movement and are therefore subject to less pullout force (Fig. 36–1B). That is, the screw angle is advantageous in resisting screw pullout, by virtue of the trajectory of the screw with respect to the vector of pullout force. FIGURE 36–1 (A) The fully integrated flanges of the TPS maintain the position of the spacer at the edge of the vertebral body to utilize the boundary effect. Translational movement is minimized by the flanges. In addition, the upward bevel and flange create a “bracing effect.” (B) Screws are angled at 45 degrees, away from the path of movement, and therefore subject to less pullout force. The TPS has several other design features that enhance construct stability in osteoporotic bone. The strength of any columnar construct relates in part to the number of intermediate stays or supporting elements. By providing in-line distraction to the collapsed spine, the TPS is able to entrain the support of paraspinal ligaments. This restoration of paraspinal ligament tension is paramount in maintaining stability of long constructs. Secondly, the 45-degree screw angle allows for longer screws. A 45-degree angle permits a longer screw purchase by a factor of sine 45 degrees (Fig. 36–1B). Thus at the 45-degree angle, 20 to 22 mm screws may be safely used without violating the posterior cortex. These longer screws have a significant advantage in soft bone as screw pullout strength is proportional to screw length. Central to the design of any spine device is the concept of subsidence, the settling or loss of vertebral height following fusion due to pistoning of graft or intervertebral spacer into adjacent vertebral end plates. All constructs undergo subsidence with loss of construct height. The result is a glacial (or not so glacial) tendency toward kyphosis. Most of the settling of the construct takes place within the first few weeks after implantation. “Permissive spine deformation,” which normally occurs and which does not result in instability or excessive loss of correction, has been termed dynamism by Benzel.4 Failure of an instrumentation system to minimize or take into account subsidence, however, results in excessive kyphosis, possibly graft fracture, pseudoarthrosis, and/or screw pullout. The TPS was designed to minimize subsidence through load sharing, multiple points of fixation, longer screws, and incorporation of the strongest part of the anatomy, the ventral lip. Fully constrained screws, integral flanges, and nonorthogonal surfaces with large contact surface area confer resilience against compression, rotational, and translational forces. The toggling and translational movements between plate and graft (or graft spacer) do not occur in the TPS, because of the integration of plate and spacer. The most important feature of the TPS is the ability to provide in-line distraction. In-line distraction accomplishes restoration of vertebral height, alignment, and tightening of the paraspinal ligaments. The forces of distraction are applied anterior to the IAR, allowing for restoration of lordosis. With soft bone, there is minimal risk to the vertebral body, because of the broad surface area through which the distraction takes place. Restoration of lordosis is of great importance. Apart from the adverse consequences relating to load bearing, posture, and gait, there is growing evidence that loss of the normal lordotic curvature of the cervical spine results in increased adjacent segment disease. More important than disc degeneration, however, are the deleterious effects of kyphosis (stretch and shear) on the spinal cord.6,7 To wit, the wall of the anterior canal increases from 9.5 cm in extension to approximately 11.5 cm in flexion; thus, the spinal cord shortens and thickens on extension and lengthens and thins on flexion.8,9
TPS DEVICES FOR TREATMENT OF
VERTEBRAL TUMORS AND
PATHOLOGICAL COMPRESSION
FRACTURES
BIOMECHANICAL THEORY UNDERLYING THE TELESCOPIC PLATE SPACER
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree