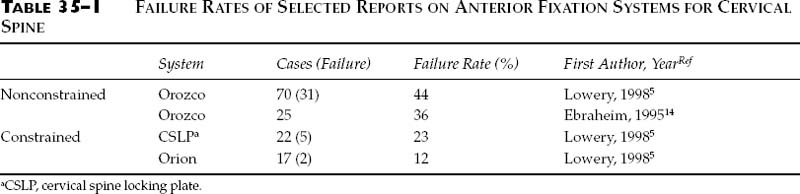
Chapter 35 The anterior cervical plate screw was developed to give a more direct fixation method and to overcome progressive posterior protruding deformity, instability, and graft dislodgment in the treatment of various conditions of the cervical spine.1–3 There are two main types of designs: nonconstrained (such as Orozco plates by Synthes, Paoli, PA) and constrained or locked systems (such as Orion system by Sofamor Denek USA, and AO titanium cervical spine locking plate [CSLP] by Synthes).4,5 Constrained or locking systems significantly increased the rigidity of the tested screw plate systems both initially and after cyclic loading.6 Based on screw purchase, there are unicortical or bicortical screws. The bicortical screws (such as Caspar system, or AcroMed system, Cleveland, OH) have more holding power than that of uni-cortical screws.6 The failure rates are also affected significantly by the length of the segment needing fixation. For example, the failure rates of two-level fixation were lower than that of three- (or more) level fixation.7 For most anterior fixation systems, screws are fixed in the vertebral bodies, which consist of mainly cancellous bone with very thin cortex, so the holding power is not great and the potential exists for loosening of the screw. Morscher et al4 created the AO titanium hollow screw-plate system, which gave good immobilization between screw and plate or screw and vertebral body. Constrained systems, such as Morscher’s CSLP system, prevent motion at the junction between the screw and plate.4,8 However, they do not increase holding power between screws and bone. With bicortical screw systems, such Caspar or AcroMed, screws are inserted through both anterior and posterior vertebral cortices, so the holding power of the screw is much higher but possible spinal cord injury remains as a major concern. Again, hardware failure in this kind of system is not uncommon. Paramore et al9 reported that 11 of 49 patients treated with Caspar plating suffered hardware failure, defined as any amount of screw backout or breakage, plate pullout, or pseudoarthrosis. These authors also concluded that Caspar plate failures are more likely to occur in the elderly and in patients who need longer constructs. Most reports on new systems have relative low failure rates,8,10–12 probably due to the short follow-up periods as stressed by Lowery and McDonough.5 There have been some longer-term reports on the high failure rate of anterior spinal fixation using the above-mentioned methods.13 Common modes of failure include broken and loosened screws or plates.5 The hardware failure rate reported by Lowery and McDonough5 was as high as 35% (44% of the nonconstrained and 18% of the constrained or locked systems) (Table 35–1). For more powerful fixation, pedicle screws have been used through a posterior approach, which has become increasingly popular in recent years.15,16 It is a technically challenging procedure although several reports have shown promise.17,18 The insertion of pedicle screws is associated with a relatively high complication risk and its success strongly depends on the experience of the surgeon. Incorrectly drilled holes or malplacement of the screws can result in nerve root injuries and fracture of the pedicle. A cadaver study using two screw insertion techniques demonstrated a high percentage of screws violating the pedicle despite creation of a laminotomy “window” to directly determine the superior, medial, and interior borders of the pedicle.19 A “blind” technique, using only bony topographical landmarks and a predetermined 30-degree medial and 20-degree superior trajectory, was associated with a violation rate of 47% (Table 35–2). The “window” technique reduced the violation rate to 25%. In a recent similar article, the critical breach rate using three methods (i.e. surface landmarks, laminoforminotomy, and computer-assisted guide system) were 66, 40, and 11% respectively.20 Clinically, studies have reported high complication rates with substantial neurological implications after posterior pedicle screw fixation. According to Esses et al,21 the overall rate of complication in their 617 cases was 27%. They also found that the rate was significantly higher in patients with previous spine surgery (45%).21 In addition, data from the thoracolumbar pedicle screw literature may help to predict the potential high complication rates of cervical pedicle screw procedures. Matsuzaki et al22 found that of 57 patients who received lumbar pedicle screw fixation, 20% had neurologic problems postoperatively and 3.5% had severe sensory impairment. It is known that when a critical breach happened, no matter which surgical technique was used the vertebral artery was likely to be injured in 73%, whereas the exiting nerve root was likely to be injured in 41%.23
A SELF-GUIDED PEDICLE SCREW
FOR ANTERIOR FIXATION OF
CERVICAL SPINE
THE PROBLEM
ANTERIOR PLATE SYSTEMS
POSTERIOR PEDICLE SCREWS
Procedure | Violation Rate (%) | First Author, YearRef |
|---|---|---|
“Blind” techniquea | 47 | Miller, 199619 |
66 | Ludwig, 200020 | |
“Window” | 25 | Miller, 199619 |
techniqueb | 40 | Ludwig, 200020 |
Computer-assistedc | 11 | Ludwig, 200020 |
a “Blind” technique: using only bony topographical landmarks.
b “Window” technique: creation of a laminotomy “window” to directly determine the superior, medial, and interior borders of the pedicle.
c Computer-assisted: computer-assisted image-guided procedure.
LATERAL MASS SCREWS
Lateral mass screws (or transverse process screws) in conjunction with plates have been used for posterior cervical spine fixation.24–27 One advantage is they do not cause as much neurovascular injury as pedicle screws.24,28
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree