Total Knee Replacement: Patella Tendon Rupture—Acute
The patellar tendon insertion to the tibial tubercle may be compromised by difficult surgical exposures needed in total knee arthroplasty. Releasing the medial border of the patellar tendon improves exposure but may lead to full detachment of the tendon from the tibia when the knee is flexed and the patella is retracted. Avulsion may also occur in the early postoperative period with vigorous physical therapy or knee manipulation. If the patellar tendon has avulsed, the presenting symptom is the inability to regain quadriceps control in the early postoperative interval.
Indications
- Intraoperative patellar tendon avulsion
- Early postoperative patellar tendon avulsion
- Late patellar tendon reconstructions with good patellar bone
Contraindications
- Deficient patellar bone
- Previous patellectomy
- Severe osteoporosis
Physical Examination
- Inability to straight leg raise
- Progressively severe extension lag
Diagnostic Test
Lateral radiograph to identify patella alta
Special Considerations
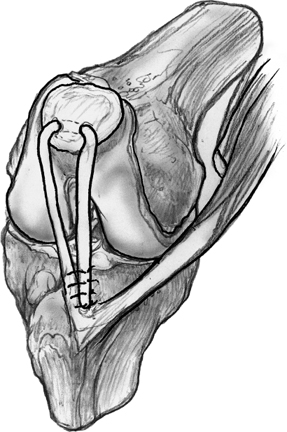
The patellar tendon may incompletely avulse from the tibial tubercle during a difficult knee replacement surgery. The natural inclination of the surgeon is to suture or staple the avulsed portion of the tendon to the tubercle. The patellar tendon is further shortened with this reattachment and may avulse with postoperative therapy. A semitendinosus graft (Fig. 43–1) is a better intraoperative alternative to repair the medial side of an avulsed patellar tendon.1,2
Preoperative Planning and Timing of Surgery
A patellar tendon or Achilles tendon allograft should be available in the event that patellar tendon repair with semitendinosus grafting is unachievable.
Special Instruments
- Tendon stripper
- Carroll tendon retriever (Accurate Surgical Scientific Instruments, Westbury, NY)
- 1/8-inch drill
- No. 2 Vicryl suture on a TP-1 needle or a No. 5 Ethibond suture on a V-40 taper cut needle
Anesthesia
General, spinal, or epidural anesthesia
Patient Position
Supine with the knee and 6 inches of the posterior thigh draped free
Surgical Procedure
- The previous knee arthroplasty incision is opened from the superior pole of the patella and extended distally 3 cm below the pes anserine insertion.
- The pes anserine insertion is palpated over the medial metaphyseal flare to identify the insertions of the gracilis and semitendinosus tendons to the tibia.
- The tendon sheath of the semitendinosus is opened along the direction of the tendon, releasing tendon slips extending distally from the tendon belly over the superficial medial collateral ligament.
- With traction applied to the tendon and the knee positioned in 90-degree flexion, the tendon is palpated four fingerwidths above the popliteal fossa.
- A transverse 2-inch incision is made over the tendon belly above the popliteal fossa. The tendon sheath is opened and the musculotendinous junction is delivered through this incision.
- The tendon is released as far proximally as possible by dissecting the muscle fibers from the tendon at the musculotendinous junction.
- The tendon is pulled into the primary medial parapatellar incision, maintaining the tendon insertion to the tibia.
- A Krakow stitch is placed in the free end of the tendon or, alternatively, a “Chinese finger trap” stitch is made along the course of the tendon.
- A 1/8-inch drill hole is made transversely through the lower third of the patella.
- A tendon retriever is used to pull the suture, followed by the tendon, through this drill hole.
- Tension is applied to the tendon and the patella displaced distally.
- The graft should be tensed and attached at a position that restricts knee flexion beyond 75 degrees.
- The tendon is sutured along the medial border of the tibial tubercle to the periosteum and deep fascia surrounding the pes anserine insertion.
- A tendon retriever is used to pull the suture, followed by the tendon, through this drill hole.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








