Chapter 10 Total Ankle Arthroplasty
Development of Total Ankle Arthroplasty Systems
Since the first report of total ankle arthroplasty in the 1970s, more than 20 total ankle arthroplasty systems have been introduced. The first-generation, cemented, constrained designs were very stable but required extensive bony resection for implantation and frequently failed because of loosening, subsidence, and extensive osteolysis. Second-generation, less constrained implants required less bone resection and did not require cement fixation; because shear forces and torsion at the bone-prosthesis were reduced, loosening was less frequent. However, increased polyethylene wear and failure compromised the stability of the components, often leading to painful impingement and subluxation or complete dislocation of the components. Contemporary, third-generation, semi-constrained total ankle systems consist of three components: a metallic baseplate that is fixed to the tibia, a domed or condylar-shaped metallic component that resurfaces the talus, and an ultrahigh-molecular-weight polyethylene bearing surface interposed between the tibial and talar components. Systems in which the polyethylene component is locked into the baseplate often are referred to as “two-piece” or “fixed-bearing” designs, whereas those with the polyethylene component not attached to the baseplate are called “three-piece” or mobile or meniscal bearing systems. Currently, five total ankle arthroplasty systems have been approved for use in the United States by the Food and Drug Administration (FDA), with another in final clinical trials (Table 10-1). Other systems are in widespread use in Europe and Asia (e.g., HINTEGRA, Newdeal SA, Lyon, France; TNK, Kyocera Corporation, Japan; BOX, Finsbury Orthopaedics, Leatherhead, Surrey, UK).
TABLE 10-1 FDA-Approved Total Ankle Arthroplasty Systems
| SYSTEM | FDA APPROVAL | CHARACTERISTICS |
|---|---|---|
| Agility (DePuy, Warsaw, IN) Agility Revision—May 2002—for revision of primary Agility arthroplasty Agility LP—2006—talar component completely covers talus; cemented | December 1992 | Requires syndesmotic arthrodesis, semi-constrained talar component; designed to be used with cement |
| INBONE (Wright Medical, Arlington, TN) | November 2005 | Modular tibial stem, intramedullary instrumentation-alignment |
| Salto Talaris (Tornier, Saint Ismier, France) | November 2006 | Conical talar component, medial radius of curvature greater than lateral; two-piece anatomical, fixed-bearing implant |
| Eclipse (Integra Life-sciences, Plainsboro, NJ) | November 2006 | Medial approach for insertion, cylindrical cuts for tibia-talus; use currently on hold |
| STAR (Waldermar Link, Hamburg, Germany) | May 2009 | Only approved three-component system, tibial fixation with two 6.5-mm cylindrical bars |
| Mobility (DePuy International, Leeds, UK) | Pending | Three-component design, anterior window for tibial stem, in clinical trials vs. Agility LP |
Adapted from Cracchiolo A 3rd, DeOrio JK: Design features of current total ankle replacements: implants and instrumentation, J Am Acad Orthop Surg 16:530, 2008.
Design Rationale
Fixed-Bearing Versus Mobile-Bearing Design
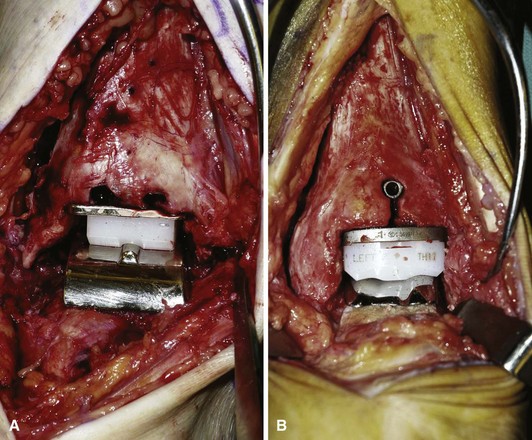
Most modern implants fall into two basic groups: those with the polyethylene component fixed rigidly to the tibial component (Fig. 10-1A) and those with a mobile polyethylene component that has the ability, at least in theory, to move under the tibial component to adapt to changes in joint forces (see Fig. 10-1B). Mobile-bearing designs are used most commonly in Europe and have a long history of outcomes from which they can be evaluated. Another theoretical advantage of these designs is the “forgiveness” of the implant, which allows small variances in alignment to be compensated for by a reorientation of the prosthesis to accommodate the joint forces. The ability of the polyethylene component to move should, in theory, keep the articulation between the talar component and the polyethylene component more congruent and less likely to edge load and have advanced wear. In experienced hands, however, there is a question of how much the polyethylene component actually moves under the tibia. Barg et al. found very little anteroposterior movement of the talar component under the tibia in follow-up radiographs of a three-component, mobile-bearing design and noted that the prosthesis functioned largely like a fixed-bearing design, but with a possible advantage of allowing an individualized position of the polyethylene insert in response to individual soft tissue loads produced by different ankle joint configurations. Aside from the STAR ankle implant (Fig. 10-2), implants approved for use in the United States are fixed-bearing designs (see Table 10-1).

FIGURE 10-2 A and B, STAR arthroplasty in patient with good bone quality and minimal deformity.
(Courtesy of Dr. William C. McGarvey, Houston, TX.)
Alignment
Currently available implant systems are designed to be placed along the mechanical axis of the limb and depend on satisfactory alignment above and below the ankle joint. The most common method of obtaining correct alignment is an external alignment jig, using intraoperative fluoroscopy to judge the alignment. At least one system uses an intramedullary alignment rod (Fig. 10-3). A potential innovation is a tomography-produced customized cutting jig, such as those available for knee arthroplasty.
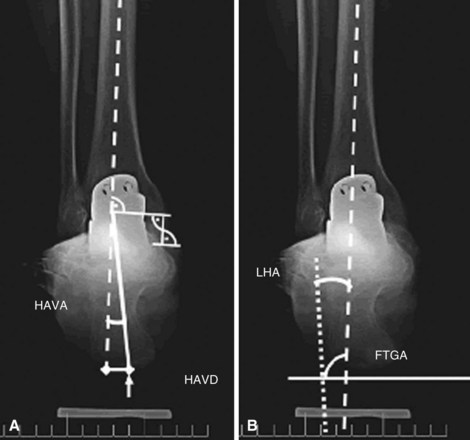
Preoperative Evaluation
At a minimum, standing radiographs of the ankle in anteroposterior, lateral, and mortise views should be obtained. Any suspicion of proximal limb malalignment should be evaluated with standing lower extremity films. Because an accurate assessment of the alignment of the hindfoot is not possible with standing films of the ankle, Frigg et al. described a hindfoot alignment view (Fig. 10-4) that gives a better appreciation of overall alignment and helps to determine if an adjunctive procedure is needed to improve the alignment of the foot distal to the ankle joint. Radiographic evaluation should include assessment of the quality of the bone stock, coronal plane alignment of the ankle with supramalleolar deformities or joint incongruencies, the presence of osteophytes requiring removal, adjacent joint arthritis or malalignment that requires correction, calcaneal pitch angle as a predictor of gastrocsoleus contracture, and the presence of major cysts or defects that will need grafting.
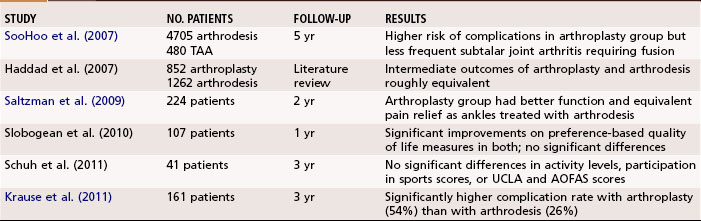
Total Ankle Arthroplasty or Ankle Arthrodesis for Ankle Arthritis
Ankle arthrodesis (see Chapter 11) has long been the “gold standard” for the surgical treatment of moderate to severe ankle arthritis. It is, therefore, reasonable to ask if there is a compelling reason to pursue total ankle arthroplasty as a treatment option for patients with ankle arthritis. Although the patient satisfaction rate after ankle arthrodesis is fairly high, there are certainly circumstances in which arthrodesis might not be the best procedure, including preexisting subtalar or other hindfoot arthritis, contralateral hindfoot or ankle arthritis, and hip or knee impairment such that motion through the ankle joint may be beneficial to the overall limb and patient function.
No level I studies have directly compared the two procedures, and reports in the literature are contradictory (Table 10-2). Longer-term studies are needed to compare these two procedures, but currently available data seem to indicate similar outcomes for patients with arthroplasty and arthrodesis suggesting that careful patient selection is mandatory for the success of either of these procedures in the treatment of ankle arthritis.
Total Ankle Arthroplasty
Patient Positioning
 Most systems require an anterior approach to the ankle. Place the patient supine on the operating table with the foot near the end of the table. Place a small bump or lift under the ipsilateral hip to help place the ankle straight and avoid the tendency of the leg to externally rotate.
Most systems require an anterior approach to the ankle. Place the patient supine on the operating table with the foot near the end of the table. Place a small bump or lift under the ipsilateral hip to help place the ankle straight and avoid the tendency of the leg to externally rotate.
 After induction of general anesthesia, apply and inflate a thigh tourniquet to control bleeding and improve visualization.
After induction of general anesthesia, apply and inflate a thigh tourniquet to control bleeding and improve visualization.
Approach
 Any significant deformity above or below the ankle joint must be corrected before placement of the total ankle implants.
Any significant deformity above or below the ankle joint must be corrected before placement of the total ankle implants.
 The approach is determined by the prosthesis design, and the reader is referred to the specific implant chosen; however, most systems require an anterior approach to the ankle.
The approach is determined by the prosthesis design, and the reader is referred to the specific implant chosen; however, most systems require an anterior approach to the ankle.
 Make an incision from about 10 cm proximal to the ankle joint on the lateral side of the tibialis tendon, over the flexor hallucis tendon. This incision is medial to the most medial major branch of the superficial peroneal nerve, the dorsal medial cutaneous nerve. Often a very small medial branch of this nerve crosses the incision just distal to the ankle joint and must be incised for exposure. The patient should be warned before surgery that a small area of numbness may be present just medial to the incision.
Make an incision from about 10 cm proximal to the ankle joint on the lateral side of the tibialis tendon, over the flexor hallucis tendon. This incision is medial to the most medial major branch of the superficial peroneal nerve, the dorsal medial cutaneous nerve. Often a very small medial branch of this nerve crosses the incision just distal to the ankle joint and must be incised for exposure. The patient should be warned before surgery that a small area of numbness may be present just medial to the incision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree