30
Tibial Spine Fracture
Tibial spine avulsion fractures represent an avulsion of the tibial eminence at the anterior cruciate ligament (ACL) insertion. Poncet first described eminence fractures in 1875. In the early literature it was felt that this was an injury that was exclusive to immature knees and therefore seen only in children. However, the more recent literature has clearly demonstrated that this fracture is seen in the adult population as well, accounting for up to 40% of all the eminence injuries seen in some series. Although the injury occurs with greater frequencies than originally felt, compared with in-substance ACL ruptures, it is relatively uncommon. Although the injury represents a ligamentous avulsion of the ACL insertion, there is a fair amount of overlap between split-type tibial plateau fractures and this injury. In some cases, they occur together (Fig. 30-1), whereas in other cases in which the eminence fracture is an isolated entity, the fracture line can extend either medially or laterally to include parts of the weight-bearing surface of the tibial plateau (Fig. 30-2).
The mechanisms of injury are similar to those of an ACL rupture. These include valgus external rotation, deceleration injuries, and, in skiing, the boot-induced injury caused by landing on the tails of the ski, resulting in anterior knee translation as the tibia is levered anteriorly against a stiff and high ski boot. The other mechanism that is seen in skiing is the “phantom foot” caused by a backward fall between the skis, creating a hyperflexion, internal rotation torque to the leg, resulting in ACL disruption. Although these injuries are seen more and more frequently secondary to sports injuries, they are also reported as a result of motor vehicle accidents and pedestrian trauma from motor vehicles.
Meyers and McKeever1 have provided the most widely used classification system for spine avulsions. They divide the injuries into three types. Type I is a nondisplaced or minimally displaced spine avulsion. Type II is an avulsion where the anterior third to half of the bony fragment is tipped in the bony bed, with the posterior aspect of the avulsion still in place. Type III represents a completely displaced fracture fragment. They further subcategorize type IIIs and describe a type III where the bony fragment is actually flipped. Although the classification has been useful in comparing treatments for various injury types, there are some shortcomings to be considered. The x-ray classifies the fracture based on its final position and does not represent maximum displacement at the time of injury, and therefore likely underrepresents the amount of instability associated with the fracture. It is likely, therefore, that most fractures classified as type II were type III at the time of injury. The classification system describes only the bony position but does not provide any information about soft tissue damage. Even injuries that have been determined to be type I injuries with minimal or no displacement have been shown to have an entrapped meniscus blocking complete reduction. Other injuries have clearly demonstrated that the meniscus or the intrameniscal ligament can frequently be entrapped in the bony avulsion, making closed management an unacceptable option.
Treatment recommendations have varied, but the classic recommendation calls for extension casting for type I injuries, extension casting versus possible open reduction and internal fixation (ORIF) for type II injuries, and ORIF for type III lesions. As we examine these treatment recommendations, one must ask the question, What other intraarticular fractures of the knee are treated with cast immobilization for 4 to 6 weeks? In all other interarticular fracture patterns, modern management has focused on anatomic reduction and rigid stabilization to allow for early range of motion, thus preserving the interarticular environment and the articular cartilage. McLennan2 reviewed management of type III fractures, comparing closed reduction and casting (group I) versus arthroscopic reduction and casting (group II) versus arthroscopic reduction and internal fixation (group III). He found Lysholm scores higher in groups II and III than in group I. Both the Tegner score and the International Knee Documentation Committee (IKDC) scores were highest in group III, intermediate in group II, and lowest in group I. When the knees were reexamined arthroscopically, only group III showed the fragment to be reduced, with groups I and II showing greater than 3 mm of offset. Arthroscopic examination also demonstrated that the chondromalacia of the patellofemoral joint that McLennan observed was directly related to the period of cast immobilization used for fracture management. He concluded that arthroscopic reduction with internal fixation produced more predictable results and was the treatment of choice for type III fractures. This recommendation has been extended to include type II fractures by other authors.

Figure 30-1 (A) Lateral magnetic resonance imaging (MRI) demonstrating a combination of plateau fracture and tibial spine avulsion with the anterior cruciate ligament (ACL) remaining intact. (B, C) Arthroscopic reduction and percutaneous fixation of both the plateau fracture and the tibial spine avulsion.
In a study completed at my institution, we reviewed 22 patients with tibial spine avulsions. The indications for surgery were x-ray evidence of displacement or instability demonstrated with a positive Lachman’s or positive pivot-shift test. All but two of the cases were treated arthroscopically.
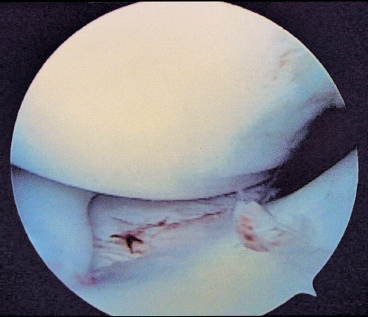
Figure 30-2 Tibial spine avulsion demonstrating extension of the fracture into the weight-bearing surface of the medial plateau.
Surgical Technique
The knee is placed in a leg holder and flexed off the end of the operating table. A tourniquet is placed on the proximal thigh. The nonoperative leg is supported on a foam cradle and abducted to the side (Fig. 30-3). Inflow is provided through a superomedial portal, the scope is placed through an anterolateral portal, and the probe and operating instruments through an anteromedial portal. The hematoma is evacuated using motorized suction. It is not necessary to employ a tourniquet in the majority of cases, as the pump provides adequate joint distention. The fragment or fragments are identified and debrided of all soft tissue around the margin to allow for good visualization of both the bony bed and the fragment (Fig. 30-4). The fat pad is debrided as necessary to obtain complete visualization of the anterior aspect of the joint. The avulsed eminence is elevated, and the bony bed is debrided of all hematoma and loose cancellous bone. The knee is carefully inspected for any entrapped meniscus or intermeniscal ligament (Fig. 30-5). When there is evidence of an entrapped meniscus, the meniscus is pulled out from under the bony fragment with a probe using an accessory portal if necessary, and the bony fragment is pushed into its bed, allowing the meniscus to return to its anatomic position. In the case of the intermeniscal ligament, if it is impossible to pull the intermeniscal ligament from the area, it is excised.
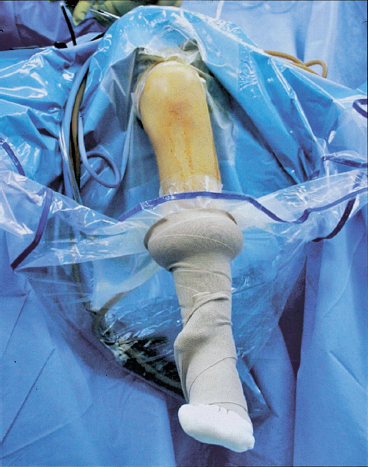
Figure 30-3 With the knee in a leg holder and the end of the table flexed, one has excellent access and control of the spine avulsion.
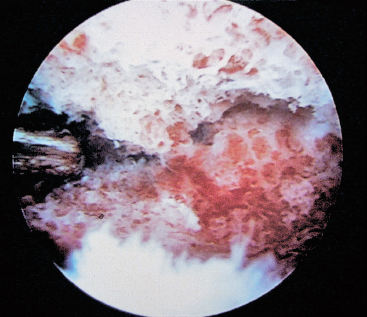
Figure 30-4 The synovial resector is used to debride all clot and loose bone from between the avulsed fragment and the tibial bed.
One of two fixation techniques is employed: cannulated screws or nonabsorbable suture. When cannulated screws are used, the fracture fragment is reduced into its bony bed and held with a probe through the anteromedial portal. A guidewire for the cannulated screw is passed percutaneously through a midmedial patella portal, and, at times, a midlateral patellar portal pierces the bony fragment and is taken distally and posteriorly until the pin engages the posterior cortex of the tibia (Fig. 30-6). Fluoroscopic control is used to be certain that the guidewire does not overpenetrate the posterior cortex. Once reduction is verified and the guidewire is checked for length using a guidewire of equal length, a 4.0 mm cannulated screw [Synthes (USA), Paoli, PA] is passed percutaneously and advanced through the spine and to the posterior cortex of the tibia (Fig. 30-7). Fluoroscopy is used frequently as the screw is passed to protect against pushing the guidewire in advance of the screw. One must watch the screw arthroscopically as it enters the joint to be certain that the threads of the screw do not contact the articular surface of the femoral condyle as it passes by the condyle into the bony fragment. Typically, one screw completely stabilizes the fracture. If the fracture is large enough, a second screw is added for further stabilization (Fig. 30-8).
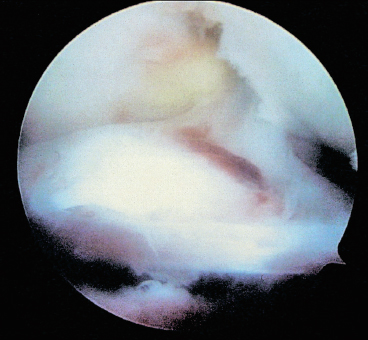
Figure 30-5 Arthroscopic view demonstrating interposition of the intermeniscal ligament between the spine avulsion and the tibial bed.
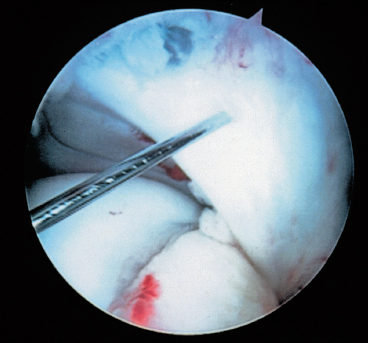
Figure 30-6 Percutaneous fixation of the spine avulsion through a midmedial patellar portal.
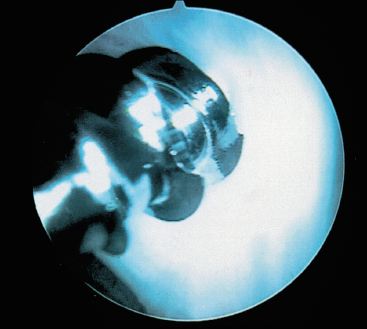
Figure 30-7 A 4.0 mm cannulated screw being passed through a midmedial puncture wound into the spine avulsion.
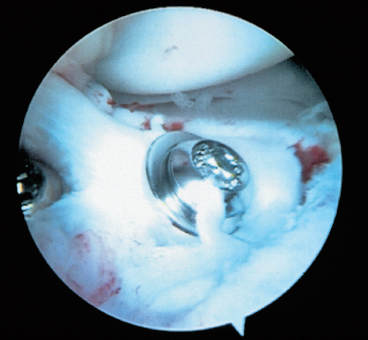
Figure 30-8 Arthroscopic image of a spine avulsion following percutaneous fixation with two cannulated screws. A washer has been used in this case but is generally not necessary.
Screw fixation is an excellent technique in those patients where the bony fragment is large enough to accommodate the screw and in those patients where the growth plate is nearly closed or completely fused. In children with open growth plates or in situations where the fragment is not large enough to accommodate a screw, suture fixation becomes an excellent surgical option.
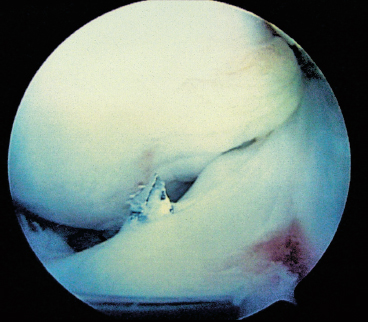
Figure 30-9 A guidewire entering the medial aspect of the spine avulsion following percutaneous fixation through a midlateral patellar portal.
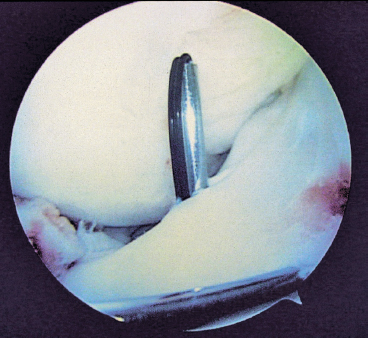
Figure 30-10 A Hewson suture passer has been placed through the tibial hole entering the joint on the medial aspect of the spine avulsion.
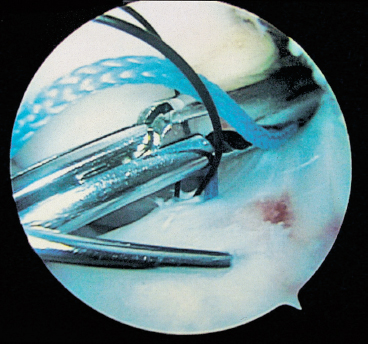
Figure 30-11 A No. 5 Ethibond is passed through the anteromedial portal, through the Hewson suture passer, and pulled out the anteromedial cortex.
The knee is positioned in a similar fashion, and instrumentation is introduced as described earlier. With a probe through the anteromedial portal, the fragment is pulled into the bony bed and held in a reduced position. A smooth Kirschner wire (K-wire) is inserted through a midmedial or midlateral patellar portal, advanced through the fragment, and passed distally and posteriorly to the posterior cortex of the tibia, holding the fragment reduced. An ACL guide inserted through the anteromedial portal is used to pass a 5/64-inch pin retrograde from the anteromedial tibial metaphysis entering the joint at the medial aspect of the avulsed fragment (Fig. 30-9). The guide pin is removed and replaced with a Hewson suture passer (Fig. 30-10) (Smith and Nephew Endoscopy, Andover, MA). Through the anteromedial portal, a No. 5 Ethibond (Ethicon, Somerville, NJ) is passed into the joint, through the loop in the suture passer, and pulled distally, exiting the anteromedial tibial cortex (Fig. 30-11). Both suture ends are secured with a hemostat. The ACL guide is reinserted, and a second 5/64-inch guide pin is passed into the joint starting 1 to 2 cm lateral to the first wire and entering at the lateral aspect of the spine avulsion. The pin is removed and replaced with the Hewson suture passer (Fig. 30-12). The opposite end of the No. 5 Ethibond is passed through the anteromedial portal, through the loop, and pulled through the joint and out the anteromedial tibial cortex, creating a loop of No. Ethibond suture that passes from the medial to the lateral aspect of the spine avulsion, exiting the tibial metaphysis (Fig. 30-13). A crochet hook is used to pull both sutures through one puncture hole on the anteromedial tibia (Fig. 30-14). The suture is toggled between the two limbs to be certain it slides effectively and that there is no soft tissue interposed. The knot is tied and passed directly down to the tibial metaphysis through the puncture wound while observing with the arthroscope to be certain that adequate tension is created in the intraarticular space to hold the fragment firmly in the bony bed (Fig. 30-15).
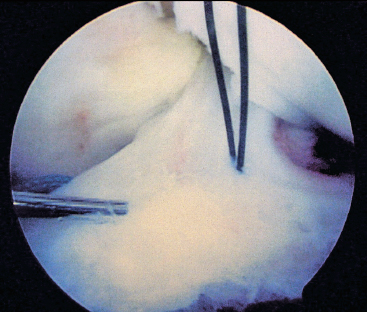
Figure 30-12 A second guidewire has been drilled and replaced with a second Hewson suture passer. This will receive the opposite end of the No. 5 Ethibond suture.
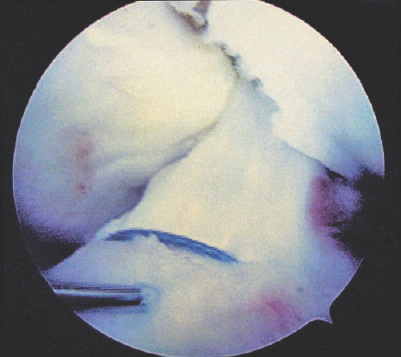
Figure 30-13 A No. 5 Ethibond crosses from the anteromedial to the anterolateral aspect of the spine avulsion, with temporary fixation maintained with the guidewire.
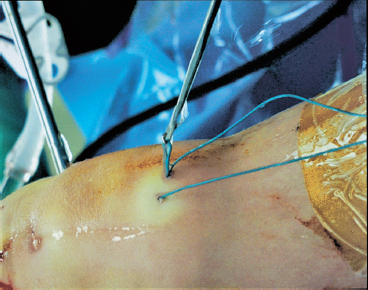
Figure 30-14 A crochet hook is passed through one puncture wound, hooking the suture exiting the opposite puncture wound, and pulling both sutures out the same puncture wound on the anteromedial tibia.
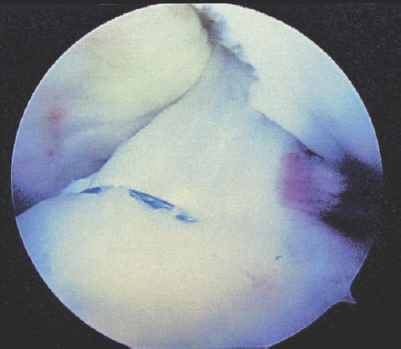
Figure 30-15 Final arthroscopic imaging demonstrating tension in the No. 5 Ethibond suture and anatomic reduction of the spine avulsion.
Postoperatively, the knee is placed in an extension brace for 4 to 6 weeks. During that period, passive range of motion is allowed from 0 to 90 degrees. This is best done with the patient in the prone position to protect against anterior translational forces on the healing avulsion fracture. Weight bearing is allowed as tolerated in the extension. Straight leg raising and quadriceps isometrics are employed to try to maintain quadriceps tone. At 4 to 6 weeks the brace is removed, and high repetition, low-load, closed-chain quadriceps exercises are begun.
Pearls and Tricks
- Visibility is critical. Thoroughly evacuate the hematoma and clean the anterior knee including as much of the pad as necessary to see the fracture fragments completely.
- The intrameniscal ligaments can be very difficult to move enough to reduce the avulsion. Removal does not destabilize the meniscus and allows easier reduction.
- At times, the avulsion won’t seat well because it is perched posteriorly. By pulling the fragments anterior first and then pushing the avulsion into the bed, a better reduction is possible.
- It can be difficult to find the drill hole with the Hewson suture passer once the 5/64-inch pin is removed. Hold the suture passer right next to the pin while the pin is removed and quickly insert through the skin to maintain the same alignment
Pitfalls and How to Avoid Them
- When using screw fixation, it is essential to monitor the progress of the guidewire and the cannulated screw using fluoroscopy.
- A screw passed percutaneously through a midmedial or midlateral patella portal passes very close to the femoral condyle. Watch carefully to be sure the screw does not damage the cartilage as it passes. When introducing the guidewire, allow enough room between the pin and femoral condyle.
- In patients with more subcutaneous fat, tying a secure knot on the tibia can be difficult. By using a sliding knot and a knot pusher, a secure knot can be advanced down to the tibia.
Conclusion
An arthroscopic approach to these fractures can be successful in the vast majority of cases. Either screw fixation or suture fixation can effectively reduce and hold the fracture in place. Screw fixation is perhaps more rigid and, therefore, the treatment of choice where the fracture is large enough to accommodate a screw and in knees where the growth plate is closed. Suture fixation becomes an excellent alternative in the growing child and in situations where there is comminution or where the fragment is too small to accommodate screw fixation. Indications for surgery are evidence of fracture displacement on x-ray or evidence of clinical laxity on examination. If the fracture is reduced, held firmly, and allowed to heal, the return to the preinjury level of sports participation can be predicted.
References
1 Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am 1970;52:1677–1684
2 McLennan JG. Lessons learned after second-look arthroscopy in type III fractures of the tibial spine. J Pediatr Orthop 1995;15:59–62
< div class='tao-gold-member'>









