26
Proximal/Distal Realignment for Patellar Instability
Indications
- Patellar instability may be manifested in one of three ways: as an acute, isolated patellar dislocation; as recurrent patellar dislocations; or as lateral patellar subluxation without overt dislocation episodes.
- The vast majority of patients exhibit lateral instability. Medial instability is typically an iatrogenic phenomenon due to an overly aggressive lateral retinacular release.1
Nonoperative Treatment
- Quadriceps strengthening is recommended with an emphasis on the vastus medialis obliquus (VMO) muscle. Stretching of tight peripatellar tissues and the hamstring musculature is also helpful.
- Patellar stabilizing braces or patellar taping may improve the patient’s subjective sensation of stability, though objective improvement in patellar tracking is difficult to quantify.
- An acute patellar dislocation resulting in significant inflammation and loss of motion is treated with immobilization, antiinflammatory medications, ice, and adjunctive modalities (i.e., phonophoresis).
Patient History
- A traumatic patellar dislocation is usually easy to discern, whereas the diagnosis of a subtle patellar subluxation requires careful attention to the history and physical examination as well as a high index of suspicion.
- Common complaints include clicking, popping, catching, giving-way, locking, and pain with bent-knee activities.
Physical Examination
- Overall alignment of both lower extremities in the sagittal and coronal plane should be assessed with the patient standing as well as supine.
- The patella should be observed for the appearance of “squinting” indicative of medial deviation, or as a “grasshopper eye” indicative of lateral patellar tilt.
- The quadriceps angle (Q-angle) is measured with the extremity in full extension and at 90 degrees of flexion with the quadriceps relaxed. Normal ranges are from 10 to 15 degrees in males and 15 to 20 degrees in females. Standing posture, genu valgum, and foot pronation may affect this measurement.
- Patellar tracking from 90 degrees of flexion to full extension should be smooth without abrupt lateral deviation (J sign). The patella should engage the trochlear sulcus by 20 to 30 degrees of flexion.
- The inability to elevate the patella at least 5 degrees above the horizontal with the quadriceps relaxed is indicative of excessive lateral patellar tilt.
- Medial and lateral patellar glide should be evaluated with the knee at 30 degrees of flexion. Normal lateral glide is one or two quadrant widths of the patella. A lateral glide of more than two quadrants is suggestive of medial restraint incompetence. Medial glide is similarly one or two quadrants, with a glide of less than one quadrant suggestive of lateral retinacular tightness, and three to four quadrants indicative of patellar hypermobility.
- The apprehension sign is often positive in patients with acute and chronic patellar instability, especially following a dislocation episode.
- Tests for associated ligamentous or meniscal injuries should also be performed, as the history and symptoms are often similar to those of patellar instability.
- A hip examination must be documented in all patients with knee complaints.
- Tests for generalized ligamentous laxity should be performed, as they are often positive in this patient population.
Diagnostic Tests
- Plain radiographs of the knee are indicated to assess the alignment and morphology of the patellofemoral joint and to rule out the presence of any concomitant fractures or loose bodies.
- The degree of patellofemoral congruence and lateral patellar tilt is best assessed with tangential or axial views such as the Merchant2 or Laurin3 view. A positive congruence angle is associated with lateral patellar subluxation. Lines drawn along the lateral patellar facet and anterior margins of the trochlea should open laterally. A closing angle is indicative of excessive lateral patellar tilt.
- Computed tomography (CT) may be useful for patients with subtle patellar tracking abnormalities. Images of the midtransverse patella taken in 15-degree increments from 0 to 60 degrees of flexion are useful to determine the position at which the patella becomes malaligned.
- Magnetic resonance imaging (MRI) can be used to evaluate the location and degree of damage to the medial retinaculum, to rule out the presence of chondral loose bodies, and to assess other intraarticular structures that may also be injured. MRI offers little in the evaluation of patellar tracking compared with CT.
Differential Diagnosis and Concomitant Injuries
- Meniscal tear
- Articular cartilage injury
- Osteochondral fracture
- Anterior cruciate ligament injury
- Medial collateral ligament injury
- Patellar tendon rupture
- Osteochondritis dissecans
- Synovial plica inflammation
Preoperative Planning
- The selected procedure(s) should be tailored to the individual patient based on a history of patellofemoral instability, corresponding physical examination, and confirmatory imaging studies. Surgery should not be based merely on pain alone, or solely on a radiographic diagnosis.
- A lateral release should be reserved for those patients with negative passive patellar tilt, a closing patellofemoral tilt angle, and medial patellar glide of less than two quadrants.4 A lateral release should not be performed as an isolated procedure for patellofemoral instability.4
- A lateral release performed in the patient with generalized ligamentous laxity or a hypoplastic patella may only worsen the patellofemoral symptoms. An overly aggressive lateral release may cause quadriceps weakness or medial patellar subluxation.1
- A proximal realignment is indicated for the patient with recurrent patellofemoral instability, an abnormal congruence angle (with or without abnormal patellar tilt), and a normal Q-angle. An isolated proximal soft tissue procedure (realignment with or without lateral release) is not indicated for the patient with associated patellofemoral arthrosis.5
- A distal realignment with medialization of the tibial tubercle (modified Elmslie-Trillat procedure)6 is indicated for the skeletally mature patient with a history of patellofemoral instability, abnormal patellar congruence, and an elevated Q-angle.
- A distal realignment in the form of an anteromedial tibial tubercle transfer7 may be effective in relieving lateral patellar contact stress in those patients with associated lateral patellar facet arthrosis.
- A distal realignment should not be performed as an isolated procedure in patients with patellofemoral instability.
Special Consideration
The presence of a wide-open proximal tibial physis is a relative contraindication to a distal realignment procedure that involves an osteotomy of the tibial tubercle.
Special Instruments, Positioning, and Anesthesia
- Broad-spectrum prophylactic antibiotics are given preoperatively.
- Anesthetic options include general anesthesia, epidural, or spinal blockade. A femoral nerve block can be administered preoperatively to supplement general anesthesia.
- The patient is placed in the supine position with a tourniquet around the proximal thigh. A thigh-high stockinette is applied to the contralateral lower extremity to prevent venous pooling.
- The operating table is typically maintained in an extended position throughout the operation, though the foot piece may be dropped at the table break to allow the arthroscopic portion to be performed with the patient’s knee hanging in a flexed position.
Examination Under Anesthesia
The knee is examined, as above, with the patient anesthetized to remove the influence of muscle guarding. An emphasis is placed on the assessment of passive patellar mobility, tilt, and tracking as in the conscious state.
Pearls and Pitfalls
- During the arthroscopic evaluation, the median patellar ridge should seat in the trochlear sulcus by 45 degrees of flexion. However, joint distention and tourniquet inflation may influence patellar position.
- The posteromedial and posterolateral compartments are optimally viewed with a 70-degree arthroscope to rule out the presence of any occult loose bodies.
- Loose bodies may be reattached to their cancellous bed, but only if they match the defect well and contain a bony fragment that will allow fixation.
- The superolateral portal is a useful landmark for the proximal limit of a lateral release if one is performed.
- When performing a lateral release, a subcutaneous pouch is created with a curved Mayo scissors between the lateral retinaculum and skin from the anterolateral to the superolateral portal (Fig. 26-1).This enables the arthroscopy fluid to egress the joint and move the skin away from the electrocautery tip to prevent an iatrogenic skin burn.
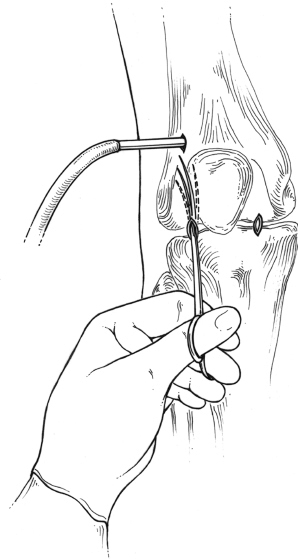
Figure 26-1 Use of curved Mayo scissors to create a subcutaneous pouch external to the lateral retinaculum that will allow the arthroscopy fluid to move the skin away from the retinaculum as the lateral release is performed. This reduces the risk of an iatrogenic skin burn from the arthroscopic electrocautery device.
- The vastus lateralis and superior lateral geniculate artery should be preserved during a lateral release.
- An adequate release results in patellar tilt of about 60 degrees above horizontal.
- The myotendinous insertion of the VMO may be included in the mobilized soft tissue flap in those patients with marked patellar instability or failure of prior surgery. It is not routinely incorporated due to its viscoelastic nature, which will allow it to stretch with time.
- Distal advancement of the proximal soft tissue flap should be avoided, as this may contribute to patella alta.
- When performing a distal realignment, the medial periosteum of the tibial tubercle should not be disrupted to preserve the blood supply to this bone.
- The tibial tubercle fragment is medially displaced 1 mm per 1 degree of desired Q-angle correction based on preoperative measurements.
- At the time of wound closure, a prophylactic anterior compartment fasciotomy is made with curved Metzenbaum scissors to dissipate the risk for a postoperative compartment syndrome and to facilitate reattachment of the anterior musculature.
Surgical Technique
Arthroscopic Evaluation
- Superolateral, anterolateral, and anteromedial arthroscopy portals are made with a No. 11 scalpel blade. The patellofemoral joint surfaces are meticulously inspected for defects, which are typically found on the lateral trochlea or medial patellar facet.
- The suprapatellar pouch and medial/lateral gutters are examined for any osteochondral loose bodies.
- Passive patellar translation and patellar tracking are assessed arthroscopically.
- The remainder of the joint is inspected for ligamentous or meniscal injuries.
Lateral Release
- The 30-degree arthroscope is placed in the anteromedial portal viewing laterally. The outflow cannula is clamped, causing further joint distention, elevation of the patella, and thus an enhanced view of the lateral retinaculum.
- The release is performed with a hooked arthroscopic electrocautery placed in the anterolateral portal. The retinacular tissues are cut within 1 cm of the patella starting at the superolateral portal. A gritty sensation is perceived as the white vertical fibers of the lateral retinaculum are released. The subcutaneous fascia typically has a maroon appearance and should not be cut.
- The knee is expressed of all fluid, and passive patellar tilt is reassessed.
Advancement of the Medial Patellofemoral Ligament (Proximal Realignment)
- The planned incisions are marked with an indelible marker along the medial border of the patella and the lateral border of the tibial tubercle (Fig. 26-2).
- A 3 cm longitudinal incision is made with a No. 15 scalpel blade over the medial border of the patella. The subcutaneous tissues are mobilized.
- The medial retinaculum and VMO are identified (Fig. 26-3). A longitudinal incision is made in the patellar insertion of the medial patellofemoral ligament (MPFL) from the 7 o’clock to the 11 o’clock position in the left knee, and the 1 o’clock to the 5 o’clock position of the right knee. The incision is extended medially at its proximal and distal extent to the level of the adductor tubercle, creating a ligamentous flap. The proximal limb is made at the myotendinous junction of the VMO. The plane underneath this flap is entered with blunt dissection while protecting the synovial fold, thus staying outside the joint.
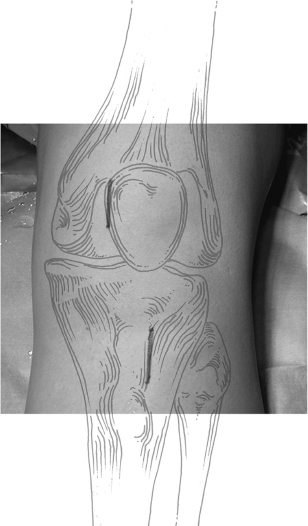
Figure 26-2 Incisions used for the proximal/distal realignment. The 3 cm proximal incision is placed along the medial border of the patella. The distal incision is made along the lateral edge of the tibial tubercle for a length of about 4 cm.
- Two Kocher clamps are placed on the tissue flap (Fig. 26-4), which is then advanced laterally 1 to 1.5 cm over the anterior surface of the patella in a pants-over-vest fashion.
- Three to four No. 2 Ethibond sutures (Ethicon, Somerville, NJ) are placed in a wide vertical mattress utilizing a double-loop configuration two finger-breadths lateral to the medial patellar border. The sutures are not tied at this time.
Realignment of the Tibial Tubercle (Distal Realignment)
- A 4 cm longitudinal incision is made along the anterolateral aspect of the tibial tubercle (Fig. 26-2). The origin of the anterior compartment musculature is sharply elevated.
- The patellar tendon insertion is identified and retracted anteriorly with an Army-Navy retractor. Multiple drill holes are then made 1 cm apart with a 3.2 mm drill bit angled 20 degrees anteriorly along a 4 cm length of the tubercle to outline the osteotomy.
- A transverse osteotomy is made just proximal to the patellar tendon insertion to a depth of 8 mm. The drill holes are connected with a 3/4-inch osteotome also angulated 20 degrees anteriorly along the length of the drill holes and tapered anteriorly.
- The tibial tubercle is medialized based on the preoperative Q-angle measurement.
- The tibial tubercle is fixed with a tapered, headless Acutrak Plus screw (Acumed, Beaverton, OR), though other fixation may be used at the surgeon’s discretion. A 0.62 mm guidewire is used to temporarily fix the tibial tubercle fragment. The Q angle is remeasured to confirm adequate correction.
- The drill is advanced up to, but not through, the posterior tibial cortex. The guidewire is overdrilled with a 3.2 mm drill bit. The depth of the drill hole is measured with a cannulated depth gauge, and an Acutrak screw of appropriate length is inserted over the guidewire. A second screw may be added as necessary. The tubercle fragment should be flush against the cancellous bone of the proximal tibia (Fig. 26-5).
- The knee is passively flexed from 0 to 90 degrees to assess the stability of fixation.
- Each Ethibond suture is tied with the patella centered in the trochlear groove with the knee at 30 degrees of flexion, while lateral traction is applied to the other sutures. The medial imbrication is reinforced with No. 1 Vicryl sutures.
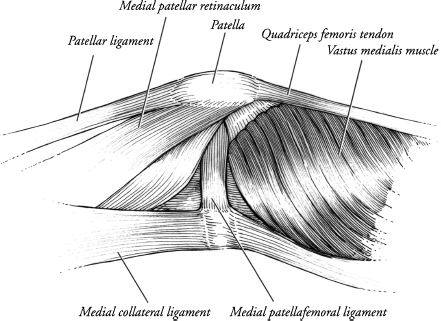
Figure 26-3 Medial view of the soft tissue restraints of the patella. (Adapted from Conlan T, Garth W Jr, Lemons J. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 1993;75:682–693.)
Final Examination of Patellar Tracking
- The tourniquet is released and patellar tracking is assessed from 0 to 90 degrees. Care is taken to assess for medial patellar subluxation caused by overcorrection of the tibial tubercle or excessive lateral advancement of the proximal soft tissue flap.
Wound Closure
- Bone wax is placed over the exposed cancellous surface of the proximal tibia uncovered by the rotated tibial tubercle.
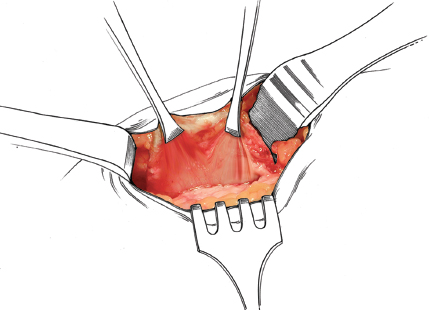
Figure 26-4 Ligamentous flap composed of the medial patellofemoral ligament and medial retinaculum that will be advanced laterally over the patella.
- The wound is thoroughly irrigated, hemostasis is achieved, and the skin is closed in layers.
Dressings and Braces
- Steri-Strips are applied to the wounds, as is a sterile compressive dressing. A CryoCuff (Aircast, Summit, NJ) is wrapped over the dressing, and the knee is placed in a hinged brace open from 0 to 60 degrees of flexion.
- Anteroposterior (AP) and lateral radiographs of the knee are obtained to confirm reduction of the tubercle fragment and placement of the fixation screw (Fig. 26-6).
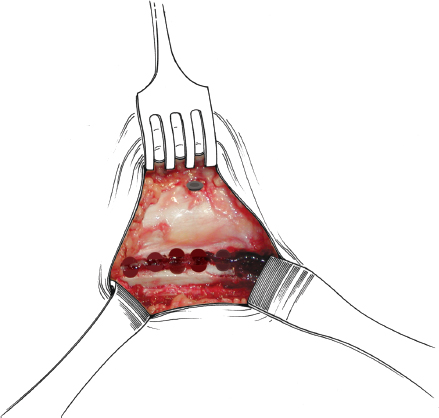
Figure 26-5 Medialized tibial tubercle. Note the drill holes used to facilitate the osteotomy, which has been performed with an osteotome, not a power saw, to prevent thermal damage to the bone.
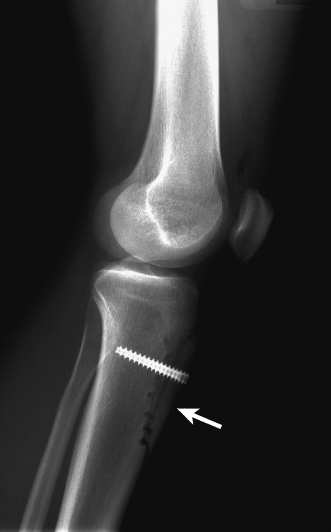
Figure 26-6 Lateral radiograph demonstrating fixation of the medialized tibial tubercle with a 6.5 mm Acutrak Plus screw.
Rehabilitation and Return to Sports
- Phase I (0 to 1 month): Graduated weight bearing is started, with the goal of attaining full weight bearing by 6 to 8 weeks. Range of motion is initiated at 0 to 60 degrees of knee flexion, with a goal of 135 degrees of flexion by 8 weeks. Active extension begins at 3 weeks for an isolated proximal soft tissue advancement, and at 6 weeks for a distal realignment pending the healing status of the tibial tubercle.
- Phase II (1 to 3 months): Normal gait patterns are reestablished. Light strengthening exercises are initiated.
- Phase III (more than 3 months): Plyometrics are begun, as is light jogging and the initiation of sport-specific functional exercises. Return to sports typically occurs at the 4-month period after the completion of a functional program and attainment of strength goals.
References
1 Nonweiler DE, DeLee JC. The diagnosis and treatment of medial patellar subluxation of the patella after lateral retinacular release. Am J Sports Med 1994;22:680–686
2 Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patello-femoral congruence. J Bone Joint Surg Am 1974;56:1391–1396
3 Laurin CA, Dussault R, Levesque HP. The tangential x-ray evaluation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop 1979;144:16–26
4 Kolowich PA, Paulos LE, Rosenberg TD, Farnsworth S. Lateral release of the patella: indications and contraindications. Am J Sports Med 1990;18:359–365
5 Fulkerson JP, Hungerford DS. Patellar subluxation. In: Fulkerson JP, Hungerford DS ed. Disorders of the Patellofemoral Joint, 2nd ed. Baltimore: Williams & Wilkins; 1990;124–148
6 Cox JS. Evaluation of the Roux-Elmslie-Trillat procedure for knee extensor realignment. Am J Sports Med 1982;10:303–310
7 Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med 1990;18:490–497
8 Conlan T, Garth W, Jr, Lemons J. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 1993;75:682–693
< div class='tao-gold-member'>









