21
Posterior Cruciate Ligament Reconstruction: All-Inside Arthroscopic Technique and Tibial Inlay Technique with Two-Strand Quadriceps Tendon-Patellar Bone Graft
Indications
- Acute and chronic complete posterior cruciate ligament (PCL) rupture associated with other ligament injuries (Figs. 21-1 and 21-2)
- Acute and chronic isolated PCL rupture (greater than 8 mm increased posterior tibial translation, 90 degrees of flexion) in active, athletic patients
- If symptomatic associated meniscal tears or early patellofemoral or tibiofemoral articular cartilage damage exists, early PCL reconstruction is recommended to lessen long-term damage.
Contraindications
- Chronic PCL rupture in which advanced symptomatic patellofemoral or tibiofemoral arthrosis has already developed
- Chronic PCL rupture in a varus-angulated knee with early medial tibiofemoral arthrosis where osteotomy is required prior to PCL reconstruction
- Dislocated knee where initial observation, arteriography, rehabilitation, protected range of motion (ROM), and muscle function return are indicated prior to surgical reconstruction; protect lower limb with a posterior padded splint to prevent posterior tibial subluxation
- 4Patients who have had inadequate rehabilitation, loss of ROM, quadriceps weakness, hyperextension gait abnormalities, where extensive rehabilitation and gait retraining are required prior to surgical reconstruction
Physical Examination
- An increase in posterior translation of the knee joint, greatest at 90 degrees of flexion, with loss of normal palpable anterior tibial stepoff relative to the femoral condyle
- Careful comparison of stability tests between knees to diagnose abnormal varus-valgus rotations or tibiofemoral rotational subluxations requiring reconstruction
- Exclude partial PCL tears with less than 8 mm posterior tibial translation (on stress radiography1); reconstruction is not required, and prognosis is good.
- Tibiofemoral rotation “dial” test at 30 and 90 degrees of knee flexion2 to determine increase in external tibial rotation with posterior subluxation of the lateral tibial plateau indicative of lateral collateral ligament (LCL) and posterolateral ligament deficiency requiring reconstruction3
- Confirm any abnormal increase in varus or valgus rotations by arthroscopic observation of lateral or medial joint opening (gap test4), indicating collateral ligament and other ligament damage.
- Complete knee examination for associated problems including patellofemoral, limb alignment, gait abnormalities, and neural and vascular examination for injuries.
Diagnostic Tests
- In dislocated knees, vascular consultation and arteriography required; delay surgery for observation
- Patellofemoral, standing 45-degree posteroanterior (PA) views and lateral radiographic views are recommended. Magnetic resonance imaging (MRI) is important in complex and revision knees for a more complete diagnosis.
- Stress radiography at 90 degrees of knee flexion to quantitate millimeters of posterior tibial subluxation, important pre- and postoperatively for long-term clinical studies (Telos or weighted sunrise techniques3). Total anteroposterior (AP) tibial translation at 30 and 70 degrees (KT-2000 arthrometer, MedMetric, San Diego, CA) provides quantitative pre- and postoperative results.
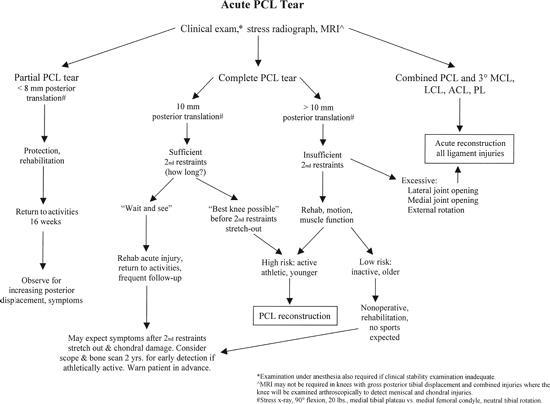
Figure 21-1 Treatment algorithm for patients with acute posterior cruciate ligament (PCL) ruptures.
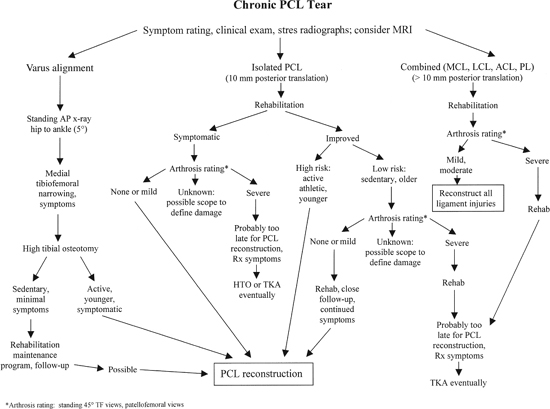
Figure 21-2 Treatment algorithm for patients with chronic PCL ruptures. HTO, high tibial osteotomy; TKA, total knee arthroplasty.
- In chronic PCL instabilities, isokinetic tests (Biodex, Biodex Medical Systems, Shirley, NY) to document adequate preoperative return of muscle strength and comparative tests postoperatively after recovery
Differential Diagnoses and Concomitant Injuries
- Associated collateral ligament, posterolateral, posteromedial, or anterior cruciate ligament (ACL) injury requiring concomitant reconstruction
- Associated neurovascular, articular cartilage injuries, joint fractures in complex injury cases
- In dislocated knees, beware of later neurovascular problems even though initial examination is normal due to arterial wall intimal damage and subsequent vascular compromise.
- Associated muscle contusions, hematomas, posterior calf musculature damage, which contraindicate posteromedial approach when tibial inlay procedure is contemplated
- Patellofemoral dislocation or injury in which adequate extensor mechanism function would not be expected to recover contraindicates PCL reconstruction.
Special Considerations
- The all-inside arthroscopic approach (arthroscopically placed tibial one or two tunnels, arthroscopically placed femoral tunnel, patellar bone inlay trough) is used in dislocated knees and where complex combined ligament reconstructions are required to decrease the operative morbidity of an additional open posteromedial approach. The all-inside technique is the procedure of choice where prior arterial injury has occurred or with concomitant posterior calf skin or muscle damage.
- The tibial inlay technique (secondary posteromedial approach with two arthroscopically placed femoral tunnels) is our preferred procedure, as it has the advantage of superior tibial graft fixation and healing. This technique is frequently required in revision knees in which prior tibial tunnels must be avoided.
Preoperative Planning and Timing of Surgery
- In acute PCL injuries with concomitant medial or lateral ligament injuries, the decision for ligament reconstruction should be delayed until observation of the neurovascular status and other injuries allows for major knee ligament surgery to be safely performed. Protect with a posterior padded splint or brace. Return of muscle function, assisted ROM, electrical muscle stimulation, decreased joint effusion, and soft tissue edema are important prior to extensive knee surgery.
- With associated damage to the LCL and posterolateral tissues, acute anatomic repair within 2 weeks is advantageous prior to scarring and loss of the ability to restore these structures. A similar situation exists for the medial ligamentous structures, which, however, are easier to reconstruct later if the ideal period for anatomic repair is not possible.
- The all-inside arthroscopic approach for PCL and ACL reconstruction, associated with limited lateral or medial anatomic approaches and surgical repair, is favored over large open operative procedures. Sufficient healing and sealing of soft tissues occurs by 2 weeks to allow low-pressure arthroscopic fluid control with careful observation at surgery. Establishing adequate outflow anterior portals for fluid egress will prevent posterior fluid extravasation.
- Appropriate use of allografts for other ligament reconstruction to avoid additional surgical trauma in dislocated knees. For PCL reconstruction, a quadriceps tendon-patellar bone-bone autograft is favored for healing purposes over an allograft. Bone-patellar tendon-bone grafts have insufficient cross-sectional area for PCL reconstruction.5 Quadriceps tendon–patellar bone or Achilles’ tendon allografts have the advantage of bone at one attachment site and sufficient collagen cross-sectional area for a two-strand reconstruction.
- Meniscus repairs of peripheral, outer one third, and complex tears extending into the middle one third are performed using a meticulous inside-out arthroscopic technique and limited posterolateral or posteromedial approach to tie the sutures directly over the posterior meniscus attachment.10 Multiple meticulous inferior and superior vertical divergent sutures are used, particularly in double longitudinal tears, major flap tears, and complex horizontal and longitudinal tears.
Special Instruments, Positions, and Anesthesia
- The arthroscopic all-inside tibial tunnel procedure involves patient positioning in a standard supine manner, thigh-high tourniquet, knee flexed 90 degrees.
- The technique for the tibial inlay posteromedial approach requires the patient to be placed on a beanbag, contoured to the patient’s thorax and pelvis and suction deflated. A safety belt is placed over the thorax and kidney rests to allow the patient to be rotated outward (operative site down) during the posteromedial approach.
- The PCL reconstruction instruments include the Acufex (Smith and Nephew, Andover, MA) Director PCL drill guide and the Acufex PCL elevator/wire catcher and Acufex Director PCL safety stop to protect the neurovascular structures.
- The arthroscopic viewer is opposite the operative knee, and the arthroscopic pump is placed conveniently to allow direct vision and control at all times.
- The tourniquet is inflated intermittently for short time periods during graft harvest or the posteromedial approach; otherwise, it is rarely used.
- General anesthesia or a spinal is most frequently used, and in prolonged multiple ligament reconstructions an indwelling urinary catheter is indicated. The opposite limb has a thigh-high venous compression stocking and is carefully protected.
- With a suspected vascular injury, the foot is draped in a sterile plastic bag to allow configuration of pulses during the reconstructive procedure.
Examination Under Anesthesia
- The examination is highly important and is used to confirm the preoperative examination, diagnosis, and operative plan.
- The examination is performed carefully on both knees for comparison to detect associated subluxations and ligament insufficiencies requiring treatment.
- Any abnormality in varus-valgus rotations requires confirmation by arthroscopic medial or lateral tibiofemoral compartment opening (gap test) under loading at 30 degrees of flexion. Tibiofemoral rotation tests are performed at 30 and 90 degrees of flexion9 in a reduced position, correcting the posterior subluxation.
Surgical Procedure
Arthroscopic Procedure
- Initial diagnostic arthroscopy is performed to confirm diagnosis, detect articular cartilage damage, do tibiofemoral gap tests, visualize cruciate ligaments, and detect meniscus tears.
- Arthroscopic medial or lateral meniscus repair is performed through a limited posteromedial or posterolateral approach6 (when subsequent medial or lateral exposure is not performed).
Quadriceps Tendon-Patellar Bone Harvest
- After exsanguination and tourniquet inflation (275 mm), a 5 to 6 cm longitudinal incision is made from the superior pole of the patella extending in the midline proximally.
- The incision is carried through the anterior investing fascia over the rectus tendon, and the pre-patellar retinaculum is reflected and protected for later closure over the grafted patellar defect.
- The quadriceps tendon and its junction with the vastus medialis oblique (VMO) and vastus lateralis oblique (VLO) are identified proximally. The proximal VMO and VLO are superficially elevated to preserve maximum quadriceps tendon length. Leaving a 4 mm margin of tendon medially, the tendon is incised perpendicularly in line with its fibers through all three layers. The knee is flexed 90 degrees to maintain tendon tension. A second sharp tendon incision is made 12 mm laterally. The overall length is 90 to 110 cm (Fig. 21-3).
- Place a curved Mayo scissor bluntly behind the quadriceps tendon to protect the underlying synovium. The proximal end of the tendon is transected and all three tendon layers grasped with an Ellis clamp.
- The tendon attachment to the anterior superior pole is carefully identified and the synovial attachment protected.
- A powered saw with the cutting blade marked to a depth of 8 to 9 mm (Steri-Strip) is used to cut the anterior cortex to 8 to 9 mm deep to produce a graft 22 mm long by 12 mm wide. The saw is used to cut the superior pole of the patella in the coronal plane. A 1/4-inch osteotome gently removes the patellar bone.
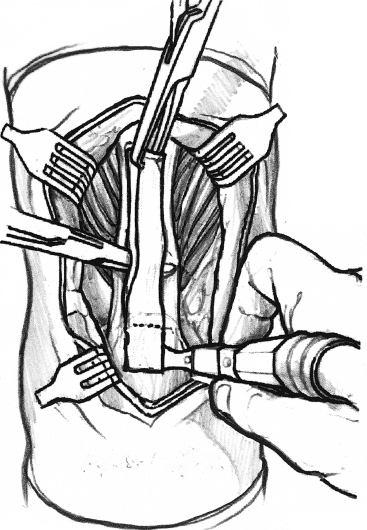
Figure 21-3 Quadriceps tendon harvest.
Two-Strand Graft Preparation
- The three layers (rectus femoris, confluent VMOVLO tendon, and vastus intermedius tendon) are identified. A sagittal split in the quadriceps tendon is performed starting at the superior pole of the patella and progressing to the end of the quadriceps tendon, perpendicular to the three layers. A meticulous technique is required to include all three layers, and two Ellis clamps are used to stabilize the proximal tendon.
- Each strand is sutured with four No. 2 nonabsorbable sutures using a baseball locking whipstitch with two or three throws on each end of the tendon graft. The graft is sized to 7 or 8 mm in diameter (Fig. 21-4).
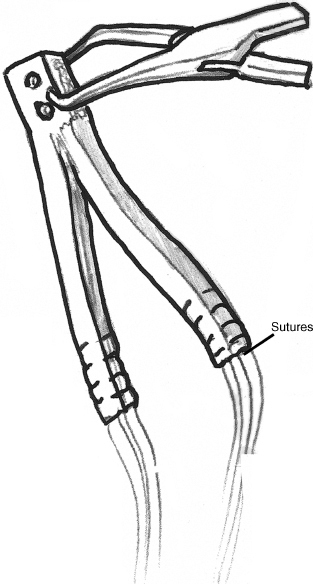
Figure 21-4 Quadriceps tendon graft preparation.
- In the all-inside arthroscopic technique, the patellar bone is sized to 9 by 12 mm to fit into the Acufex oblong tunnel graft sizer. A single drill hole with a No. 2 nonabsorbable suture is placed as a leader suture. A marking pencil marks the bone-tendon junction and 1:00 strand (anterolateral strand) for lateral arthroscopic identification.
- In the tibial inlay technique, the patellar bone is fashioned into a 8 × 12 × 22 mm cube shape. Two 4.5 mm holes are overdrilled at the one-third and two-third lengths, leaving a sufficient bridge of bone at each end for later cancellous screw internal fixation.
Femoral Tunnel Location
- The native PCL footprint is identified if possible. The PCL attachment extends from high in the notch (12 o’clock position) to approximately the 5 o’clock position, occupying the distal one third of the lateral wall of the medial femoral condyle. The most distal (shallow) portion follows the articular cartilage being 3 mm from the edge, up to the 5 o’clock position, where the footprint is 5 mm from the edge. The deep portion is 11 to 12 mm from the articular edge high in the notch.6
- The PCL attachment is divided into anterior, middle, and posterior thirds with a small postero-oblique portion (posterior-proximal insertion). The shallow to distal portions are also divided into distal, middle, and proximal thirds. This provides a grid for identification of PCL tunnel locations.
- The anterior and posterior meniscofemoral ligaments when present help define the attachment site.
- The PCL attachment is mapped with a calibrated probe, shallow and deep portions identified, and the 12, 1, 2, 3, and 4 o’clock position marks made on the cartilage edge with electrocautery.
- The Acufex PCL femoral template is used to define the placement of the two 8 mm femoral tunnels (Fig. 21-5). The femoral hole is initially marked with an arthroscopic pick to maintain correct guidewire placement. The first guide pin is placed at the 1 o’clock position, 6 mm proximal to the cartilage edge. The second guide pin is placed at the 3 o’clock position, 8 mm proximal to the cartilage edge. This places the tunnels in the central and distal thirds of the PCL attachment.
- In the all-inside technique, the two 8 mm holes overlap. The femoral trough is further gently dilated with the Acufex dilator (9 × 13 mm trough) to conform to the sized patella bone.
- In the tibial inlay technique, the two femoral guide pins are separated an additional 2 to 3 mm to separate the bone tunnels. The diameter of each tunnel is based on the diameter of each graft. The guidewire is positioned at 90 to 110 degrees of knee flexion to exit in an extraarticular location on the anteromedial femoral surface at least 15 mm proximal to the articular cartilage.
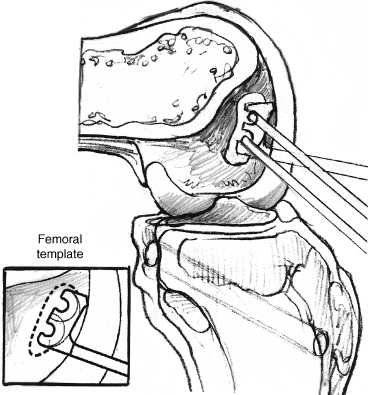
Figure 21-5 Use of Acufex PCL femoral template to identify correct placement of guide pins in all-inside technique.
- The tunnel is drilled completely through the proximal cortex to allow the graft to exit proximally and to attach the graft in a subperiosteal position. A gentle VMO muscle-splitting approach is used to identify the proximal tunnel for later graft fixation using the prior graft harvesting skin incision. All tunnel bony edges are smoothed with a rasp.
All-Inside Technique Tibial Preparation
- Using the 30-degree arthroscope, proceed through the anteromedial portal, high in the notch to view the posterior region of the joint. A central and anterolateral portal is used to pass instruments protecting the ACL. The Acufex PCL elevator carefully frees the posterior capsule and recess behind the PCL. The tibial PCL stump is removed with curved baskets, electrocautery, and shaver. Rarely, a posteromedial accessory portal is used to remove the PCL stump with the shaver.
- The Acufex tibial aiming device is placed through the central portal. The tip of the guide rests on the most distal posterior tibial capsule insertion at the PCL distal attachment to ensure sufficient bone (15 to 20 mm) proximal to the tibial tunnel. The anterior location of the tibial tunnel is 4 cm from the joint line, about 50 degrees (Fig. 21-6). The safety stop attachment of the guide, with the guide pin chucked to a defined length, prevents too far advancement of the tibial pin. The PCL elevator-catcher is placed over the pin.
- In the single tibial tunnel technique, the tunnel is placed in the central far distal PCL tibial attachment. In the two-tunnel technique (preferred), the tunnel is separated by 1 to 2 mm, 7 to 8 mm diameter, carefully matched to each graft strand diameter, and the tunnel originates on each side of the tibial tubercle (Fig. 21-6). The two tibial tunnel technique allows more secure fixation (separate soft tissue interference screw and post to each strand) and better healing by avoiding the larger single osseous tunnel.
All-Inside Graft Passage
- The soft tissue ends of the graft are passed through a 12 to 15 mm lateral arthrotomy (at the inferolateral portal). A posteromedial switching stick may be used to facilitate passage into the tibial tunnels.
- The bone block is threaded with a No. 2 suture, placed through a guide pin that is passed through the anterolateral portal and medial femoral tunnel, and exits just above the knee joint. The bone block is passed under arthroscopic control. If any difficulty is encountered with graft passage due to the large nature of the graft, the lateral arthrotomy may be simply enlarged to allow direct graft visualization.
- The bone block at the femur is fixated with a 7 or 9 mm × 20 mm absorbable interference screw placed at the 1 o’clock position.
- The graft is tensioned to 45 N, and the knee is cycled 30 times to condition the graft. The graft should not lengthen with knee flexion, indicating correct graft placement. The normal 10 mm anterior tibial stepoff is verified at 90 degrees of flexion. An 89 N anterior drawer force is added and graft fixation performed, tying each graft suture over a post (4.0 mm cancellous screw/washer). A 30 mm absorbable soft tissue interference screw (carefully sized and usually 7 to 9 mm diameter) is added to each separate tibial tunnel.
- The knee joint is flexed from 0 to 135 degrees, graft tension arthroscopically observed, and stability confirmed.
Tibial Inlay Technique Reconstruction
- After preparation of the two femoral tunnels and debridement of the PCL stump to reestablish the normal posterior synovial recess, a separate posteromedial exposure is initiated.
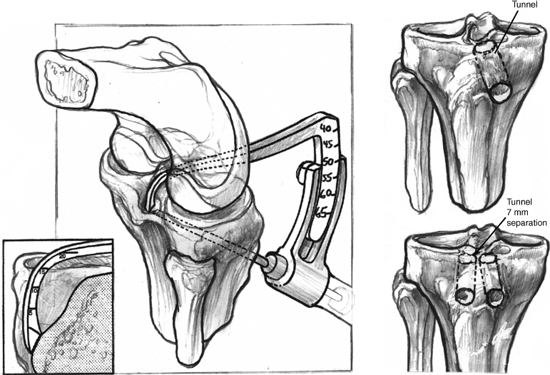
Figure 21-6 Location of single- or double-tibial tunnels.
- The patient is rolled (airplaned) to the operative side in a down position. The tourniquet is inflated. A figure-four knee position is assumed (60 degrees of external hip rotation, 30 degrees of knee flexion). The foot is placed on a well-padded Mayo stand, elevated to lift the knee away from the table. An assistant externally rotates the foot and controls the lower limb. The surgeon and assistant, with operative headlights, are seated at the opposite side of the table, able to look directly at the operative site.
- The 7 to 8 cm longitudinal posteromedial incision is made just proximal to the knee flexion crease, carried distally over the medial head of the gastrocnemius and medial to the semitendinosus tendon.
- The sartorial fascia layer is incised in line with the gracilis and semitendinosus tendons, medial to the gastrocnemius, avoiding the saphenous nerve and vein. The pes tendons are retracted anteriorly to visualize the interval between the semimembranosus tendon attachment and medial gastrocnemius muscle. The oblique popliteal expansion of the semimembranosus is identified and may require partial cutting to improve exposure. With gentle lateral retraction of the medial gastrocnemius and popliteal neurovascular structures (not visualized), the inferolateral semimembranosus tendon sheath extension to the popliteus is seen and cut from its attachment to the posterior border of the common semimembranosus tendon. This exposes the direct insertion of the semimembranosus tendon to the posteromedial tibia and is a key point for dissection to the PCL attachment just laterally.
- An S-shaped retractor is placed to lift the semimembranosus tendon medially away from the dissection. The medial head of the gastrocnemius is carefully retracted laterally with a Richardson retractor and gravity assistance, exposing the popliteus. Two Steinmann pins carefully placed can be used in place of the Richardson retractor to maintain the lateral position of the gastrocnemius muscle. Care is taken not to provide undue retraction of the popliteal neurovascular structures.
- Knowledge of the posterior vascular anatomy is crucial to avoid complications and damage to geniculate arteries and recognition of vascular abnormalities. The medial inferior geniculate artery runs 2 to 3 mm from the superior surface of the popliteus muscle and is protected during dissection by subperiosteal tibial dissection superior to the muscle along the posteromedial tibial border. The middle geniculate artery arises just proximal to the joint line to pierce the posterior central capsule and supply the cruciate ligaments and is protected by knee flexion and avoiding more proximal dissection. Most importantly, in 5 to 7% of knees, the popliteal artery divides 2 cm or more proximal to the popliteus muscle7, 8 and may pass anteriorly (and not posteriorly) to the popliteus muscle belly, placing the artery at risk during exposure of the PCL attachment adjacent to the popliteus muscle. In the rarer popliteal artery entrapment syndrome, the popliteal artery passes medial or directly through the medial gastrocnemius muscle head, again at risk during the posteromedial approach.
- The PCL tibial attachment, as a midline proximal tibial depression, and the medial femoral condyle are palpated and identified. The posterior capsule is incised along the medial femoral condyle superiorly to enter the joint. Further dissection of the capsule distally, direct to the PCL attachment, avoids the posterior horn medial meniscus attachment. The dissection identifies intraarticularly the PCL attachment, and further distal dissection subperiosteally lifts up a tissue flap just beneath the popliteus, thereby protecting the vascular structures.
- A rectangular slot to match the patellar bone is cut with an osteotome. The slot is started 1 cm distal to the normal PCL attachment site, to position the graft against the posterior tibial slope, 15 to 20 mm distal to the joint line, to preserve the more proximal posterior tibial slope that the graft lies on. Avoid recessing the bone graft.
- The rectangular patellar graft is fixated with two 4.0 mm cannulated screws. The guidewires are angled distally to avoid intraarticular penetration. The graft screw hole is overdrilled to achieve compression.
- Two wire loops previously placed through the femoral tunnels and angled into the posterior recess are brought into the wound site for graft passage. The soft tissue portion of the graft is divided and marked into 1 o’clock and 3 o’clock strands and passed through the joint and femoral tunnels. Tension on the graft confirms fixation. A lateral radiograph confirms placement.
- The capsulorrhaphy is closed. Vascular clips are available for possible geniculate injury or other bleeding sources. The tourniquet is deflated and hemostasis controlled, the wound is irrigated, and closure is performed.
- The patient is rolled (airplaned) to the operative side in a down position. The tourniquet is inflated. A figure-four knee position is assumed (60 degrees of external hip rotation, 30 degrees of knee flexion). The foot is placed on a well-padded Mayo stand, elevated to lift the knee away from the table. An assistant externally rotates the foot and controls the lower limb. The surgeon and assistant, with operative headlights, are seated at the opposite side of the table, able to look directly at the operative site.
Graft Femoral Fixation with Tibial Inlay Technique
- The anteromedial extracapsular subperiosteal exposure along the anteromedial femur, proximal to the joint, is performed, identifying the femoral tunnels and graft exiting proximally. The VMO is carefully protected, limiting the exposure.
- Arthroscopic visualization of the graft confirms proper placement of both strands prior to fixation. With 45 N graft tension on each strand, the graft is conditioned (knee flexed 30 times) through a full range of motion, monitoring the normal anterior tibial stepoff and graft length changes.
- A staple post is placed proximal to the femoral tunnels, the graft is fixated by tying each suture, placing 45 N on each graft strand, 90 degrees of flexion, and 89 N anterior drawer. A soft tissue interference screw for each tunnel is added (Fig. 21-7). Arthroscopic evaluation of the graft confirms tension, fixation, and return of stability.
- The graft harvest site is closed. The patella is grafted from bone saved, including the posterior tibial bone that was removed.
Initial PCL Graft Protection After PCL Reconstruction
- Lower leg hinged postoperative brace for 8 weeks, including sleep, to prevent sudden knee flexion greater than 135 degrees
- Weight bearing: 1/4 body weight (BW) for 1 to 4 weeks postoperative at 0 degrees in brace; 1/2 BW in brace, 0 to 90 degrees of flexion 5 to 6 weeks postoperative; full weight bearing, wean crutches, 7 to 8 weeks postoperative in brace
- ROM: 0 to 120 degrees from postoperative day 1 to 6 weeks; 0 to 135 degrees 7 to 8 postoperative weeks. Do not push ROM greater than 135 degrees, which places high forces on graft. No full flexion squatting activities. Limit total daily knee motion cycles to 60 for first 4 weeks.
- Regain 0 to 110 degrees as soon as possible, definitely by second postoperative week.
- Regain normal hyperextension (3 degrees) as soon as possible; no further hyperextension, which overloads the graft.
- Full progression of quadriceps exercises from closed to open chain consistent with weight-bearing rules. No hamstring isotonics until 8 weeks postoperative.
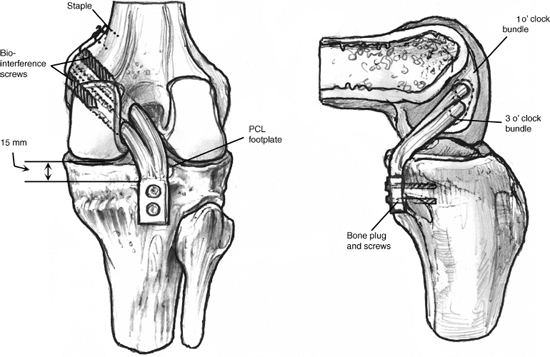
Figure 21-7 Details of graft fixation are shown for tibial inlay technique.
Pearls and Pitfalls
- Quadriceps tendon harvest requires knowledge of the three layers (rectus femoris tendon, confluent VMO and VLO tendons, vastus intermedius tendon) to make sure an absolute perpendicular cut is made through all layers with the knee flexed 90 degrees to maintain tension.
- The quadriceps tendon may appear too short; however, reflection of the VMO and VLO muscles allows additional length, particularly for the arthroscopic all-inside technique. The longer length (90 to 110 mm) allows the graft to pass completely through the tibial tunnel for anterior tibial secure fixation and faster healing.
- The patellar bone defect is bone-grafted using bone obtained with a core tunnel reamer at a tibial or femoral site. Meticulous closure of the quadriceps tendon uses a combination of nonabsorbable (sparingly) and absorbable sutures.
- The PCL femoral attachment site must be thoroughly mapped out to place the graft into the correct position. A graft tunnel located only in the distal one third (close to the articular edge) or proximal one third (deep attachment portion) of the PCL will have abnormally large and potentially injurious forces with knee flexion or knee extension, respectively. Placement within the central third of the PCL attachment at the 1 and 3 o’clock positions results in more uniform load sharing between the two strands.9
- Double fixation of the collagenous two-strand graft is performed using four No. 2 baseball sutures tied over a post, with an additional soft tissue interference screw in correctly sized holes equal to the diameter of the graft.
- The determination of the graft tension in both strands with knee flexion is critical to avoid over-constraining the joint, resulting in high graft forces and failure. The femoral PCL tunnel in the central third to distal third is preferred to replace the majority of the PCL that functions (maximal graft elongation) with progressive knee flexion10 and avoiding proximal graft placement, which functions (maximal elongation) with knee extension. Accordingly, the two-strand graft is tensioned at 90 degrees of flexion (45 N graft tension, 89 N anterior tibial displacement), assuming the ACL is intact and the normal anterior tibial stepoff is confirmed with stability restored.
- Use of the tibial inlay posteromedial approach requires thorough knowledge of normal anatomy and variations in the vascular structures, which may occur in up to 5% of limbs. For example, the popliteal artery may course medial to the medial gastrocnemius head or through the medial head posteriorly, which could be injured on the approach. The anterior tibial artery may pass directly through the popliteus muscle. A subperiosteal dissection of the superior portion of the popliteus muscle belly is favored to protect against potential damage to the anterior tibial artery. Anatomic references are available that thoroughly describe abnormal vascular patterns.7, 8
- In the tibial-inlay technique, the two graft strands are secured by a suture post, and great care is required to perform a limited VMO muscle split to achieve subperiosteal anteromedial femoral fixation without excessive injury to the VMO, which would cause postoperative pain and limit postoperative knee flexion.
- Site of tibial graft attachment, either by inlay or single/double tibial tunnel, is always greater than 15 mm from the joint line, as far distal as possible, extending to the posterior tibial rounded edge to prevent upward migration of the graft or cutting into the posterior tibial proximal buttress. In the tibial inlay, too deep an inlay results in too vertical of a graft position, which is less advantageous for resisting posterior tibial translation.
- In knees with ACL disruption, avoid excessive anterior tibial displacement and graft shortening by placing the knee at full extension, which, usually with intact medial and lateral ligaments, produces a normal tibiofemoral relationship. Mark the graft length (either tibial or femoral side with all-inside or tibial inlay technique, respectively). Place the knee at 90 degrees of flexion, maintain graft length, and confirm a normal anterior tibial stepoff (equal to opposite knee on preoperative testing). Maintain this stepoff by gentle anterior tibial positioning to compensate for gravity effects, and avoid further anterior tibial displacement. Confirm arthroscopically the normal position of the medial and lateral tibiofemoral joint at 30 and 90 degrees by observing the anterior position of the medial and lateral meniscus relative to the femoral condyles. An abnormal anterior tibial subluxation is easily recognized.
- Use of the tibial inlay posteromedial approach requires thorough knowledge of normal anatomy and variations in the vascular structures, which may occur in up to 5% of limbs. For example, the popliteal artery may course medial to the medial gastrocnemius head or through the medial head posteriorly, which could be injured on the approach. The anterior tibial artery may pass directly through the popliteus muscle. A subperiosteal dissection of the superior portion of the popliteus muscle belly is favored to protect against potential damage to the anterior tibial artery. Anatomic references are available that thoroughly describe abnormal vascular patterns.7, 8
Postoperative Care
- The all-inside arthroscopic procedure may be performed as an outpatient or 24-hour admission, using appropriate pain management. Intraarticular local anesthetic plus morphine is initially used. Continuous cold therapy is instituted. Antiinflammatory medication is avoided if possible to increase healing effects.
- All patients take two aspirins a day for 10 days, wear compression stockings, and do ankle pump exercises throughout their waking hours. Patients who have undergone complex reconstruction of two or more ligaments with extended operative time wear postoperative intermittent compression boots to facilitate venous return and reduce postoperative swelling.
- Appropriate careful postoperative monitoring is instituted for knee dislocations or prior vascular injury.
- A postoperative motion brace (Bledsoe Brace Systems, Grand Prairie, TX) is used initially to protect the PCL reconstruction from sudden knee flexion.
- Associated posterolateral and lateral reconstructions require added postoperative protection up to 4 weeks against undue varus loading using a bivalved padded cylinder cast, removed four to six times a day for protected active-assisted ROM.
- The patient is instructed to maintain limb elevation at all times, except out of bed, to lessen postoperative edema (unless vascular issues contraindicate this position).
Advanced Rehabilitation and Return to Activity
- Continued muscle strengthening, balance, proprioceptive conditioning, gait retraining
- Running program initiated at 9 months postoperative assuming less than 30% isokinetic quadriceps and hamstring deficit, and no pain, swelling, or cartilage damage
- Avoid weighted squats greater than 45 degrees of flexion.
- Avoid sudden downhill deceleration activities, which overload the graft. Sport-specific drills are begun at 9 months postoperation.
- Repeat stress radiographs, KT-2000, confirm stability. Consider repeat MRI if any question on graft healing, maturation.
- Try to limit full athletic participation until 9 to 12 months postoperation, given magnitude of operation and added graft maturation time.
References
1 Hewett TE, Noyes FR, Lee MD. Diagnosis of complete and partial posterior cruciate ligament ruptures. Stress radiography compared with KT-1000 arthrometer and posterior drawer testing. Am J Sports Med 1997;25:648–655
2 Noyes FR, Stowers SF, Grood ES, et al. Posterior subluxations of the medial and lateral tibiofemoral compartments. An in vitro ligament sectioning study in cadaveric knees. Am J Sports Med 1993;21:407–414
3 Noyes FR, Barber-Westin SD, Grood ES. Newer concepts in the treatment of posterior cruciate ligament ruptures. In: Insall JN, Scott WN, eds. Surgery of the Knee. Philadelphia: WB Saunders; 2001: 841–877
4 Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 2000;28:282–296
5 Noyes FR, Butler DL, Grood ES, et al. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 1984;66:344–352
6 Rubman MH, Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscal tears that extend into the avascular zone. A review of 198 single and complex tears. Am J Sports Med 1998;26:87–95
7 Colborn GL, Lumsden AB, Taylor BS, Skandalakis JE. The surgical anatomy of the popliteal artery. Am Surg 1994;60:238–246
8 Mauro MA, Jaques PF, Moore M. The popliteal artery and its branches: embryologic basis of normal and variant anatomy. AJR Am J Roentgenol 1988;150:435–437
9 Mannor DA, Shearn JT, Grood ES, et al. Two-bundle posterior cruciate ligament reconstruction. An in vitro analysis of graft placement and tension. Am J Sports Med 2000;28:833–845
10 Galloway MT, Grood ES, Mehalik JN, et al. Posterior cruciate ligament reconstruction. An in vitro study of femoral and tibial graft placement. Am J Sports Med 1996;24:437–445
< div class='tao-gold-member'>









