23
Posterolateral Knee Reconstruction
The anatomy, biomechanics, diagnosis, and treatment of injuries of the posterolateral corner of the knee have undergone increasing scrutiny in recent decades,1–21 and there have been significant gains in our understanding of the posterolateral corner of the knee. Despite this, diagnosis of posterolateral corner knee injuries remains elusive, and their treatment remains controversial. Perhaps the difficulty in diagnosing injuries to the posterolateral corner of the knee is in its complex anatomy, with multiple layers and fibrous attachments between local tendons, ligaments, and bones.17, 20, 21
An interest in understanding the posterolateral knee structures biomechanically has contributed tremendous knowledge about the function these structures perform in providing stability to the posterolateral corner of the knee. Most authors now agree that the popliteus tendon, popliteofibular ligament, and fibular collateral ligament (FCL) are among the most important contributors to posterolateral corner knee stability.12, 22, 23 A reconstruction that reproduces the normal anatomy of these structures, when they are damaged beyond repair, is likely to yield the best functional result.7, 24
Surgical Indications and Other Options
Posterolateral knee instability is a complex surgical problem with a steep learning curve for the practicing surgeon. If possible, acute injuries to the posterolateral corner of the knee should be addressed by direct visualization and repair of the involved structures. When available tissues have been damaged beyond the scope of primary repair, or for chronic injuries where repair is not possible due to attenuation, scarring, and retraction of these structures, reconstruction is often the only viable alternative.24
Before repair or reconstruction can be initiated, the surgeon must first be able to recognize a posterolateral corner knee injury. Recognition of these injuries must often be done in patients who have a concurrently associated cruciate ligament or meniscal injury. Clinical motion tests useful for recognizing posterolateral corner knee injuries include the reverse pivot shift, posterolateral drawer, external rotation recurvatum exam, varus stress at 30 degrees, and the dial test. In the case of chronic posterolateral corner knee injuries, the patient’s history can often be the most useful tool in recognizing an underlying posterolateral corner knee injury. Classically, these patients will ambulate with a varus thrust gait.14
A variety of reconstruction techniques have been proposed to address posterolateral corner knee instability. A patient being considered for surgery for chronic posterolateral corner instability should first have an evaluation of limb alignment. When varus malalignment exists, a proximal tibial osteotomy should be performed before reconstruction of the posterolateral corner is undertaken. Correction of varus malalignment will reduce the risk of reconstruction graft failure, and in some cases may add to stability of a lax posterolateral corner. Among the most commonly referred to procedures the surgeon has to choose from when performing a reconstruction of the posterolateral corner of the knee are femoral bone block advancements,4, 17 biceps tenodesis,16, 25 FCL allograft,21 and popliteus tendon reconstruction with Achilles’ or patella tendon allografts.18 This chapter describes a new technique to reconstruct chronic posterolateral corner knee injuries that focuses on reproducing the normal anatomy of the posterolateral corner.26
Surgical Technique
The surgical technique described in this chapter uses a double-bundle, two-graft technique for anatomic reconstruction of the popliteofibular ligament, popliteus tendon, and FCL.26
To perform this surgery, the patient is placed in the supine position on the operating table, and prepped and draped in a sterile fashion. The initial skin incision is centered over Gerdy’s tubercle, starting 7 to 8 cm proximal to the joint at the level of the lateral intermuscular septum, and extending distally for 3 to 4 cm over the anterior compartment of the leg.17 This is classically described as a lateral hockey-stick incision. Two or three fascial incisions are then made. The first fascial incision splits the superficial layer of the iliotibial band in line with its fibers. It extends from Gerdy’s tubercle distally to the supracondylar process of the femur proximally. The two sides of this incision are retracted to expose the normal femoral attachments of the FCL, popliteus tendon, and the mid-third lateral capsular ligament. A vertical arthrotomy incision is then made through the meniscofemoral portion of the mid-third lateral capsular ligament. It is made through an imaginary line 1 cm anterior and parallel with the fibular shaft with the patient’s knee flexed to 70 degrees. This incision allows for access to the popliteus origin on the femur, the popliteomeniscal fascicles, and the lateral meniscus.
The second fascial splitting incision is made just posterior and parallel to the long head of the biceps femoris. This is a very delicate part of the operation. The common peroneal nerve must be identified in its location posterior and medial to the long head of the biceps femoris tendon via a common peroneal nerve neurolysis. The interval between the lateral head of the gastrocnemius and soleus is then developed with blunt dissection. This provides access to the posteromedial aspect of the fibular styloid and the posterolateral aspect of the tibia. The posterior popliteus sulcus,18 which is at the musculotendinous junction of the popliteus, can be identified through this interval by palpation of the posterolateral aspect of the tibial plateau. If necessary, the third fascial incision is made between the posterior border of the iliotibial tract and the anterior aspect of the short head of the biceps femoris. The popliteofibular ligament’s attachment site on the posteromedial downslope of the fibular styloid can be identified through this interval, if it cannot be identified through the second fascial incision.
Two tendon grafts are prepared by vertically splitting an allograft calcaneous and Achilles’ tendon into two equal portions, parallel with the fibers of the tendon.19 The tendons must be at least 23 cm in length to complete the reconstruction in most patients. The bony portions of the graft are sized with a rongeur to fit the 9 mm 20 mm femoral tunnels. Two passing sutures are placed through drill holes in the bone plugs. The bone plugs are then pulled into their respective femoral tunnels by passing the sutures through the femur with the eyelet-tipped guide pins, and are fixed into the femoral tunnels with cannulated interference screws (Fig. 23-1).
After the attachment sites of the FCL, popliteus tendon, and popliteofibular ligament are identified through the fascial incisions and the reconstruction grafts are prepared, one tibial, one fibular, and two femoral bone tunnels are reamed. The fibular tunnel is made through the fibular head from the attachment site of the FCL, on the lateral aspect of the head, to the attachment site of the popliteofibular ligament on the posteromedial downslope of the fibular styloid. A horizontal incision through the anterior arm of the long head of the biceps femoris, which enters the biceps bursa,21 is useful to identify the FCL’s attachment on the fibula (Fig. 23-2).
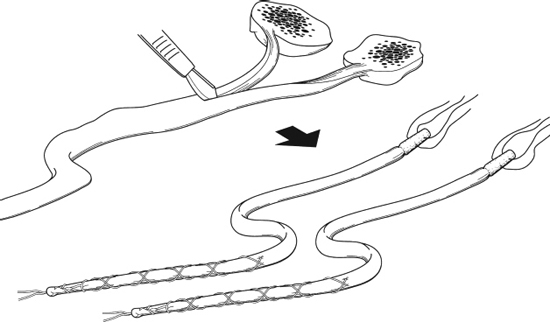
Figure 23-1 Achilles’ tendon allograft preparation.
To make the tibial tunnel, a cannulated tunnel-aiming device is placed on the posterior popliteus tibial sulcus at the level of the popliteus musculotendinous junction. It is important to leave the bony margin under the articular cartilage intact. A Kirschner wire (K-wire) is then drilled in an anteroposterior direction from the distal medial aspect of Gerdy’s tubercle to the posterior popliteal tibial sulcus.18 A 9 mm reamer then prepares this tunnel from anterior to posterior.
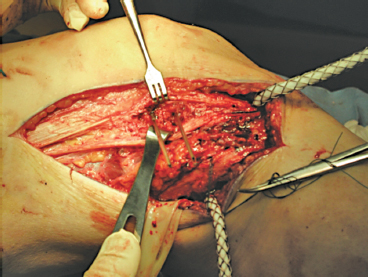
Figure 23-2 Intraoperative photograph showing the lateral aspect of a right knee. The knee’s orientation has the hip to the left of the photograph and the ankle to the right. Note the Beath pins, as they emerge from the femur, marking the sites of the femoral tunnels. The peroneal neurolysis can be observed inferiorly (peroneal nerve in Penrose drain).
To make the femoral tunnels, the femoral attachment sites of the FCL and popliteus tendon are identified. The FCL’s attachment site, just proximal and posterior to the lateral epicondyle, is identified through the retracted interval between the iliotibial band incision. The femoral attachment site of the FCL can be identified just proximal and posterior to the lateral epicondyle. The attachment site of the popliteus tendon is identified through the vertical arthrotomy in the meniscofemoral portion of the mid-third lateral capsular ligament. Two eyelet-tipped guide pins are drilled into the FCL and popliteus tendon (this tunnel should be placed at the proximal fifth of the popliteus sulcus)7 and attachment sites on the femur, parallel to each other. The guide pins should exit the femur proximomedial to the medial epicondyle and adductor tubercle. Two 9 mm tunnels are then reamed to a depth of 20 mm. The bone bridge between the two tunnels should be about 8 to 9 mm (Fig. 23-3).
The first graft, fixed into the popliteus attachment on the femur, is used to reconstruct the popliteus tendon. The free end of this graft is passed distomedially through the popliteal hiatus to reach the posterolateral aspect of the lateral tibial plateau. The graft is then pulled through the tibial tunnel from posterior to anterior, where it emerges just medial and distal to Gerdy’s tubercle (Fig. 23-4).
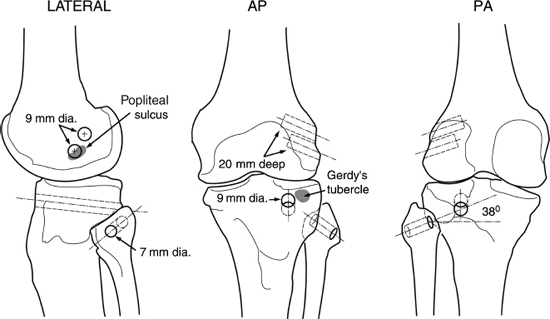
Figure 23-3 Lateral, anteroposterior (AP), and posteroanterior (PA) illustrations of tibial tunnel locations. The shaded areas represent useful surgical landmarks.
The second graft, inserted into the FCL attachment on the femur, is utilized to reconstruct both the FCL and popliteofibular ligament. Its tendinous portion is passed deep to the superficial layer of the iliotibial tract and anterior arm of the long head of the biceps femoris, along the normal course of the FCL. The graft is next passed through the fibular head from lateral to posteromedial. With the patient’s knee flexed to 30 degrees and in slight valgus, and in neutral rotation, traction is applied to the graft, and it is fixed in the fibular head with a bioabsorbable cannulated interference screw. This reconstructs the FCL. The remaining graft is then passed into and through the tibial tunnel from posterior to anterior. This portion of the graft reconstructs the popliteofibular ligament, once it is tightened (Fig. 23-5).
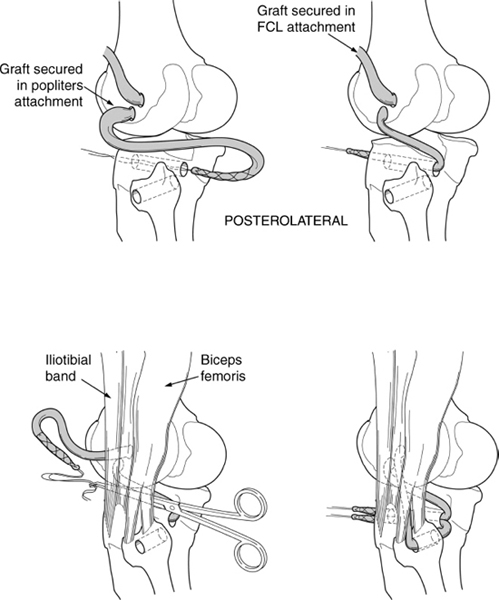
Figure 23-4 Posterolateral illustration demonstrating positioning and tunneling of the Achilles’ tendon allografts.
Finally, with the knee in 60 degrees of flexion and in neutral rotation, both the popliteofibular ligament and popliteus tendon grafts are fixed, with an anterior bioabsorbable cannulated interference screw, into the tibial tunnel, and also with a barbed staple over the grafts onto the tibia (Fig. 23-6).
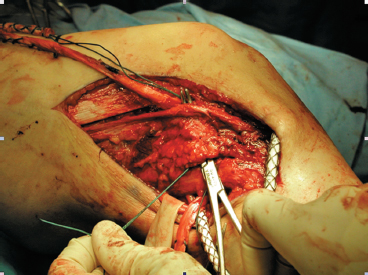
Figure 23-5 Intraoperative photograph of a right knee. The knee is oriented with the hip to the left of the photograph and the ankle to the right. Note the direction the grafts are pulled from the femur to the femoral and tibial tunnels beneath the biceps femoris.
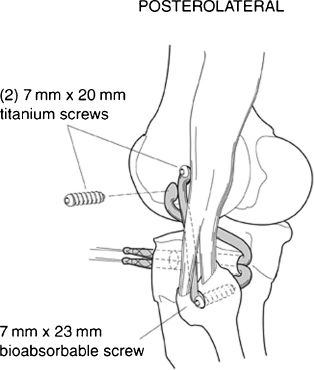
Figure 23-6 Posterolateral illustration demonstrating final fixation of the grafts into their respective tunnels.
Tips and Tricks
As is true of most surgical procedures, exposure is everything. Well-placed incisions can yield easy access to otherwise difficult-to-find structures, especially in the chronically injured posterolateral corner, where many of the natural soft tissues have been replaced by fibrous scar tissue. Anatomic data can be useful in identifying the attachment sites of the main posterolateral structures, even when severe soft tissue destruction is present.7
Important bony landmarks to consider are the femoral popliteus sulcus, lateral femoral epicondyle, tibial popliteal sulcus, and fibular styloid process. The FCL’s femoral attachment occurs in a bony depression 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle.7 Its fibular attachment is in a bony landmark 8.2 mm posterior to the anterior fibular head and 28.4 mm distal to the tip of the styloid process.7 The popliteus tendon inserts into the proximal half of the anterior fifth of the popliteus sulcus. The popliteofibular ligament attaches, with two separate arms, onto the anterior and posterior aspect of the posteromedial portion of the fibular styloid process.7
Pitfalls and How to Avoid Them
When preparing the allograft for implantation, it is advisable to trim the grafts in parallel with the sized bone block. Too large of a tendon diameter can cause the tendon to bunch up and get caught when passing it through the tunnels (particularly the smaller tunnel in the fibular head) and prevent proper tightening of the allograft in vivo. Perhaps the most serious consequences of posterolateral knee reconstruction are potential injury to the common peroneal nerve or injury to the large neurovascular bundle of the posterior knee. Exploration, identification, and neurolysis of the peroneal nerve should be done in every case to avoid unnecessary injury to it during the surgical process. Careful placement of the tibial tunnel with adequate protection of the posterior neurovascular structures during tunnel reaming is important to avoid the tibial nerve and popliteal artery/vein. A large Chandler retractor serves this protective function well.
Conclusion
Posterolateral corner knee injuries are difficult to diagnose and treat. A consensus has not yet been reached on the best way to treat chronic posterolateral corner injuries. As is the case with anterior and posterior cruciate ligament reconstructions, anatomically correct reconstruction of the posterolateral corner of the knee is likely to produce the best clinical results.7
References
1 O’Brien SJ, Warren RF, Pavlov H, et al. Reconstruction of the chronically insufficient anterior cruciate ligament with the central third of the patellar ligament. J Bone Joint Surg Am 1991;73:278–286
2 Clancy WG, Sutherland TB. Combined posterior cruciate ligament injuries. Clin Sports Med 1994;13:629–647
3 Fleming RE, Blatz DJ, McCarroll JR. Posterior problems in the knee. Posterior cruciate insufficiency and the posterolateral rotatory insufficiency. Am J Sports Med 1981;9:107–113
4 Hughston JC, Jacobson KE. Chronic posterolateral instability of the knee. J Bone Joint Surg Am 1985;67:351–359
5 Hughston JC, Norwood LA, Jr. The posterolateral drawer test and external rotation recurvatum test for posterolateral rotational instability of the knee. Clin Orthop 1980;147:82–87
6 LaPrade RF, Resig S, Wentorf FA, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. Am J Sports Med 1999;27:469–475
7 LaPrade RF, Ly T, Wentorf FA, Engebretsen L. The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament and lateral gastrocnemius tendon. Am J Sports Med 2003;31:854–860
8 Seebacher JR, Inglis AE, Marshall JL, et al. The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am 1987;64:536–541
9 Stäubli H-U, Rauschning W. Popliteus tendon and lateral meniscus: gross and multiplanar cryosectional anatomy of the knee. Am J Knee Surg 1991;4:110–121
10 Nielsen S, Rasmussen O, Ovesen J, Andersen K. Rotatory instability of cadaver knees after transection of collateral ligaments and capsule. Arch Orthop Trauma Surg 1984;103:165–169
11 Veltri DM, Warren RF. Anatomy, biomechanics, and physical findings in posterolateral knee instability. Clin Sports Med 1994;13:599–613
12 Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am 1987;69:233–242
13 Kannus P. Nonoperative treatment of grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med 1989;17:83–88
14 LaPrade RF, Terry GC. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med 1997;25:433–438
15 Noyes FR, Barber-Westin SD. Surgical restoration to treat chronic deficiency of the posterolateral complex and cruciate ligaments of the knee joint. Am J Sports Med 1996;24:415–426
16 Veltri DM, Warren RF. Operative treatment of posterolateral instability of the knee. Clin Sports Med 1994;13:615–627
17 Terry GC, LaPrade RF. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med 1996;24:732–739
18 Last RJ. The popliteus muscle and lateral meniscus, with a note on the attachment of the medial meniscus. J Bone Joint Surg Br 1950;32:93–99
19 Latimer HA, Tibone JE, El Attrache NS, McMahon PJ. Reconstruction of the lateral collateral ligament of the knee with a patellar tendon allograft. Am J Sports Med 1998;26:656–662
20 Terry GC, LaPrade RF. The biceps femoris muscle complex at the knee: its anatomy and injury patterns associated with acute anterolateral-anteromedial rotatory instability. Am J Sports Med 1996;24:2–8
21 LaPrade RF, Hamilton CD. The fibular collateral ligament-biceps femoris bursa. An anatomic study. Am J Sports Med 1997;25:439–443
22 Grood ES, Stowers SF, Noyes FR. Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am 1988;70:88–97
23 Veltri DM, Deng XH, Torzilli PA, Maynard MJ, Warren RF. The role of the popliteofibular ligament in stability of the human knee: a biomechanical study. Am J Sports Med 1996;24:19–27
24 LaPrade RF, Hamilton CD, Engebretsen L. Treatment of acute and chronic combined anterior cruciate ligament and posterolateral knee ligament injuries. Sports Med Arthro Rev 1997;5:91–99
25 Wascher DC, Grauer DJ, Markolf KL. Biceps tendonesis for posterolateral instability of the knee: an in vitro study. Am J Sports Med 1993;21:400–406
26 LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A. An analysis of an anatomical posterolateral knee reconstruction. An in vitro biomechanical study and development of a surgical technique. Am J Sports Med 2004;32:1405–1414
< div class='tao-gold-member'>









