25
Arthroscopic Lateral Retinacular Release
Lateral retinacular release of the patella is a surgical procedure that may be performed arthroscopically or open, depending on the underlying indication and whether other adjunctive procedures are to be performed.1 Although the procedure is straightforward and relatively easy to perform, its technical simplicity should not be confused with its potential surgical morbidity. Close attention to operative indications, surgical technique, and especially rehabilitation programs helps ensure a successful outcome.
Lateral retinacular release is often performed in conjunction with other surgical procedures, such as medial retinacular reefing, proximal and distal patella realignment, tibial osteotomy, femoral osteotomy, and patella osteochondral debridement or grafting.2 In most cases, lateral release is performed alone for recurrent patellar subluxation or patellar facet compression syndromes.3 Lateral facet overload syndrome is the most common indication for surgical release of the retinaculum. Differential diagnosis includes synovial plica, loose bodies, symptomatic fat pad impingement, patellar tendinitis, osteochondritis of the patella, symptomatic bipartite patella, and reflex sympathetic dystrophy.4 Although lateral retinacular release may be performed as an open procedure, this chapter discusses the authors’ arthroscopic approach.
Surgical Indications and Other Options
The characteristic patient who requires a lateral release presents with subpatellar or lateral patellar pain, crepitus, occasional mild swelling, and symptoms such as catching or locking. Pain is especially aggravated by loading the patella in flexion, such as during squatting, deep knee bending, jumping, or lunging. A history of patellar trauma or instability may also be elicited.4 A comprehensive history is taken, and a physical examination is performed.
The caveat in performing lateral retinacular release is to identify those patients who will benefit from other adjunctive procedures, for example, the patient with recurrent patellar dislocations secondary to a large Q angle and dysplastic patellar femoral joint.3 Patients with a history of direct trauma to the anterior aspect of the knee or previous surgical procedures often present with chronic patellar pain that does not respond to conservative measures such as physical therapy and nonsteroidal antiinflammatory drugs.3 Patellar pain and instability can progress to interfere with simple everyday activities such as stair climbing and rising from a seated position. A history of connective tissue disorders and endocrinopathies should also be considered. Prior to considering surgical intervention, the adequacy of, and the patient’s compliance with, a conservative program including physical therapy should be assessed.4
Physical Examination
The physical examination includes evaluation of biomechanical alignment, range of motion, swelling, knee stability, and quadriceps muscle tone. A specific painful arc of motion should be noted, especially when the patella engages the trochlea at about 30 degrees of flexion. Patellar mobility must also be assessed. Often patients with peripatellar fibrosis have restricted side-to-side patellar femoral motion when compared with the uninvolved side. Patellar tilt is evaluated clinically and radiographically (see below). Tenderness along the lateral retinaculum usually accompanies the lateral patellar facet overload syndrome.3 Apprehension with lateral push on the patella suggests an element of patellar instability. The patient may also complain of medial peripatellar knee pain from incompetent medial soft tissue structures or synovial plica.
Diagnostic Studies
Routine radiographic evaluation of the knee should always include Merchant views of the patella to assess patellar tilt and congruence.4 Standing weight-bearing films are also obtained. A patellar tilt greater than 10 degrees or a congruence angle that is greater than 0 degrees may be pathologic.2 Although not mandatory, magnetic resonance imaging (MRI) and computed tomography (CT) scan can be useful.3, 5 The MRI is used to evaluate degenerative changes of the articular cartilage and focal areas of mechanical overload represented by bone edema on T2-weighted images and inversion recovery sequences (Fig. 25-1). The existence of a synovial plica may also be noted. Dynamic MRI scans to help evaluate patellar tracking are available in some centers. Fu and Maday3 discussed the use of CT to assess patellar tracking. They identified two types of maltracking that may be missed on plain radiographs: one relocates with patellar-trochlear engagement, and the other worsens with flexion. These tests become more useful when the primary source of symptoms remains unclear.
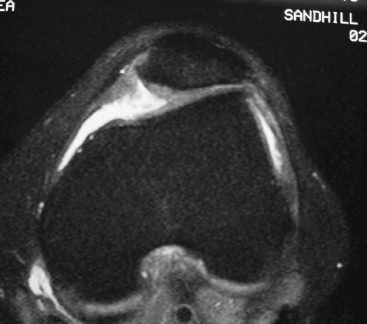
Figure 25-1 Magnetic resonance imaging (MRI) scan of patellofemoral joint. Note lateral tilt and subluxation of patella with loss of articular cartilage from lateral patella facet.
Surgical Technique
Lateral retinacular release should be considered once it is apparent that conservative measures and a patella femoral strengthening program have failed to alleviate the pain or restore the patient’s previous level of activity.2 The patient is brought to the operating room and positioned supine on a well-padded table with attention to head and limb position. Care should be taken to avoid undue contact pressure at bony prominences and neurovascular compression. General, regional, or local anesthesia can be utilized. These options are discussed preoperatively with the patient and the anesthesiologist. An examination under anesthesia is performed to reassess generalized ligamentous laxity, range of motion, stability of the knee, and the contribution of pain to the limitations seen on the physical exam. Patellar mobility is also reassessed and compared with that on the opposite side. The operative leg is then placed in a well-padded leg holder with an upper thigh-level tourniquet.
Standard diagnostic arthroscopy is performed. We prefer a superior medial inflow cannula inserted at the inferior edge of the vastus medialis. We do not routinely inflate the tourniquet during surgery, but if it is used, 300 mm Hg has been satisfactory for hemostasis. A systematic diagnostic arthroscopy includes evaluation of the articular surfaces of the patella and femoral groove, medial parapatellar recess for synovial plicae, and medial and lateral compartments for arthritic changes or meniscal tears. The knee is brought into flexion from 0 to 90 degrees to evaluate the location of patellar impact and patellar tracking throughout the range of motion. This should be done with the knee inflated with Ringer’s lactate solution and again with the knee partially deflated. Gravity feed of irrigation fluid provides adequate pressure for visualization, but an arthroscopy fluid pump can also be used if the surgeon so chooses. The arthroscope is then transferred to the medial portal and directed to the lateral patellofemoral joint and retinaculum. An arthroscopic evaluation of patellar tracking is again performed as well as an assessment of the amount of patellar tilting or overhang of the lateral facet beyond the margins of the lateral femoral condyle. A patellar chondroplasty to shave or debride loose, fibrillated articular cartilage is performed prior to the lateral release.
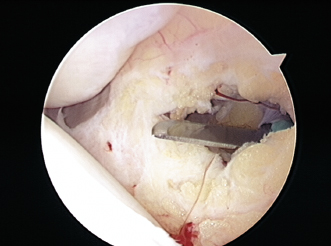
Figure 25-2 Release of inferior lateral retinaculum at lateral portal site with one-piece No. 15 scalpel. This permits easy entry of the radiofrequency (RF) lateral release probe and determines the inferior extent of the release.
The inferior aspect of the retinaculum is incised with a one-piece No. 15 blade scalpel (Fig. 25-2). This releases the lowest portion of the retinaculum adjacent to the inferior lateral portal and provides a good starting point for the radiofrequency cutting instruments. A blunt trocar is used to elevate the skin off the lateral retinaculum. This is done by inserting the trocar in the inferior lateral portal and sweeping the skin off the top of the retinaculum subcutaneously (Fig. 25-3). The skin is freed off the retinaculum up to the superior pole of the patella, which is the most proximal extent of the lateral release in most cases. A curved radiofrequency chisel is then inserted into the inferior lateral portal, and the lateral retinaculum is released from its lower margin to the level of the superior patella. The release is performed slowly to ensure coagulation of small vessels. If they are moved too fast, the radiofrequency devices will cut through the vessels rather than coagulate. The retinaculum is released in layers from the synovial side to the subcutaneous side. As the thick vertical bands of the retinaculum are released, the lateral facet of the patella lifts up away from the lateral femur condyle, and the patella articular surface becomes more parallel to the femoral trochlea. Once this is achieved, the release is stopped. The curved chisel is then used in a coagulation mode, and the cut edges of the retinaculum are painted slowly to ensure adequate hemostasis after the fluid pressure is released (Fig. 25-4). The retinacular release is performed about 1 cm away from the lateral edge of the patella. Care should be taken to avoid extension of the lateral release into the vastus lateralis tendon, as this sometimes leads to a localized area of fibrosis and pain. In some cases, the patella may track too medially if the lateral release extends too high.6
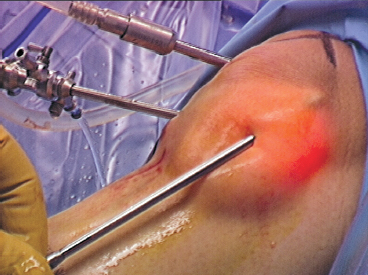
Figure 25-3 Subcutaneous separation of skin from lateral retinaculum using blunt arthroscope obturator. Subcutaneous mobilization provides a protective fluid layer that prevents extension of RF energy to the skin layer and helps define the full thickness of the retinaculum.
If a tourniquet has been inflated, we recommend it be released prior to closure to look for any small bleeding vessels that should be coagulated. Also, the arthroscopy fluid pressure should be reduced to facilitate coagulation. After the release has been performed, the patella tracking should be reexamined to confirm improved mobility and translation (Fig. 25-5). It should be possible to evert the patella about 70 degrees if an adequate release has been performed.3
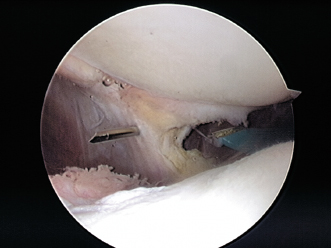
Figure 25-4 Localization of superior extent of lateral retinacular release using an 18-gauge spinal needle.
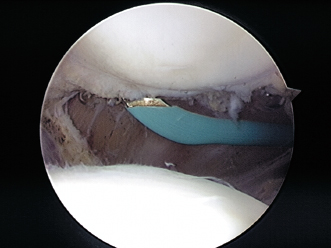
Figure 25-5 Completion of lateral release and coagulation of cut ends of retinaculum. Note the decompression of the lateral patellofemoral articulation.
Prior to closing the portals, the knee is copiously irrigated with antibiotic solution through the inflow cannula. The portals are closed with 2–0 Prolene sutures, and adhesive strips, Betadine ointment, and a sterile dry dressing are applied. A pain-management catheter can be inserted from an accessory puncture if desired.
Rehabilitation
Range of motion and physical therapy are started within the first 3 to 5 days after surgery. If the patient has experienced a high level of pain prior to surgery or a symptom complex consistent with reflex dystrophy, a continuous passive motion machine is prescribed.
This may be used the first week to initiate motion and reduce swelling. Physical therapy emphasizes range of motion and control of swelling for the first 3 weeks followed by a progressive closed-chain strengthening program and vastus medialis retraining.3 A lateral buttress knee sleeve can give the patient additional security and help facilitate the strengthening program in cases of patellar subluxation.
Tips and Tricks
Be sure to undermine the skin with a blunt probe prior to performing the lateral release. This helps to define both the superficial and deep margins of the retinaculum, provides an insulating layer of fluid between the retinaculum and the skin, and provides better distribution of local anesthetic when utilized.
The use of an 18-gauge spinal needle to mark the upper extent of the release is helpful. This is inserted after undermining the skin at the level of the superior pole of the patella (Fig. 25-6). It is much easier to determine the extent of the release “externally” rather than arthroscopically.
Move the radiofrequency probe slowly. Many new users of radiofrequency devices have a tendency to move the handpiece too rapidly across the tissue. This cuts the tissue quite nicely but unfortunately often cuts through small bleeding vessels as well rather than coagulating. A layer-by-layer slow release controls intraoperative bleeding much better.
Avoid the use of a tourniquet or, if used, deflate it prior to removing the arthroscope. Individual bleeders can then be identified and coagulated. Likewise, lowering the inflow fluid pressure also helps identify small bleeding vessels.
Pitfalls and How to Avoid Them
The most common complication after lateral release is hemarthrosis.2 Attention to the Tips and Tricks section should help avoid these complications. The most troublesome bleeder is usually at the superior extent of the lateral release near the edge of the vastus lateralis muscle. If the release is extended too far into this area, care should be taken to identify and coagulate this vessel. Thorough painting of the cut retinacular edge with the radiofrequency device also minimizes postoperative swelling.
The second most common pitfall is an inadequate release. Be sure the release extends down into the inferior lateral portal. Always check to be sure the lateral edge of the patella can be manually elevated after the knee is deflated. Be sure the release is performed “full thickness.” This should extend to the subcutaneous layer.6 The use of a blunt trocar to separate the skin from the retinaculum helps in defining the outer edge of the retinaculum.
Be careful not to use high-power settings on the subcutaneous layer. Rare cases of skin necrosis from using high-power cautery devices directly on the subcutaneous layer have been reported.
Conclusion
Lateral retinacular release is a quick and easy operation to perform arthroscopically. However, it should not be performed injudiciously. Preoperative indications and postoperative goals should be discussed with the patient, and a conservative program of antiinflammatory medication and physical therapy should always be pursued first. The length of the lateral release is usually determined by the preoperative indications and whether other procedures are to be performed. A limited retinacular release is performed from the inferior lateral portal to the superior pole of the patella in most cases of patellar facet overload syndrome. A more extensive release may be required in patients with patellar subluxation or dislocation, or in patients who are having adjunctive procedures including patellar realignment.4, 7 The most important interoperative concern should be control of bleeding. A dry knee intraoperatively facilitates the rehabilitation program and minimizes postoperative quadriceps atrophy.
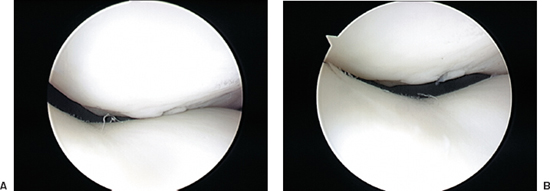
Figure 25-6 (A) Lateral impact of patella facet during knee flexion prior to retinacular release. (B) Centralization of patella after retinacular release. Note damaged articular cartilage with fissuring.
References
1 O’Neill DB. Open lateral retinacular lengthening compared with arthroscopic release. J. Bone Joint Surg Am 1997;79:1759–1769
2 Busch MT, DeHaven KE. Pitfalls of the lateral retinacular release. Clin Sports Med 1989;8:279–290
3 Fu FH, Maday MG. Arthroscopic lateral release and the lateral patellar compression syndrome. Orthop Clin North Am 1992;23:601–612
4 Grelsamer RP. Current concepts review: patellar malalignment. J Bone Joint Surg Am 2000;82:1639–1650
5 Shellock FG, Mink JH, Deutsch AL, Fox JM. Patellar tracking abnormalities: clinical experience with kinematic MR imaging in 130 patients. Radiology 1989;172:799–804
6 Nonweiler DE, DeLee JC. Diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med 1994;22:680–686
7 Marumoto JM, Jordan C, Akins R. Biomechanical comparison of lateral retinacular releases. Am J Sports Med 1995;23:151–155
< div class='tao-gold-member'>









