A. Mechanism of Injury—The fracture is usually a result of a compressive force: a direct axial compressive force, an indirect coronal compressive force, or a combined axial and coronal compressive force. The most common cause is a fall or a motor-vehicle accident.
B. Factors Influencing Fracture Patterns
1. Position of the leg relative to the direction of force application and degree of knee flexion at the time of force application.
• Medial plateau fractures—Medial plateau fractures result from a combination of compression and varus stress.
• Lateral plateau fractures—Lateral plateau fractures result from a combination of valgus stress and a force applied from the lateral side of the joint.
2. Bone quality and the patient’s physiologic age.
• Young patients—Because of the good quality of their bone, young patients are prone to ligamentous injuries in combination with simple split fractures.
• Older patients—Older patients are more likely to have depression-type or split-depression fracture without associated ligamentous injury.
II. Evaluation
A. History
1. Knee pain—Clinical suspicion for a tibial plateau fracture should be high whenever a patient complains of pain about the knee after sustaining an injury.
2. Hemarthrosis with extension of the hematoma into the soft tissues—The presence of a hemarthrosis with extension of the hematoma into the soft tissues, particularly at the sites of ligamentous attachments, should heighten clinical suspicion for a tibial plateau fracture.
3. Mechanism of injury—The mechanism of injury and any other influencing factors should be determined from the history.
B. Physical Examination
1. Inspection—The skin condition of the extremity should be noted. Specifically, internal degloving as well as open wounds should be noted. All open wounds must be examined to rule out communication with the joint. The joint should be injected with 50 mL of sterile saline under sterile conditions to determine whether any suspicious wounds communicate with the joint.
2. Palpation—The neurovascular status of the extremity should be assessed.
• Compartment syndrome—Compartment syndrome, although a rare entity with these types of fractures, must always be ruled out. Direct measurement of compartment pressures should be carried out if the clinical assessment is unreliable.
• Pulses—The presence or absence of popliteal, dorsalis pedis, and posterior tibial pulses must be documented. Doppler studies or arteriograms are indicated if these pulses are absent.
• Ligamentous injury—A strong suspicion for ligamentous injury should be maintained on examination because as many as 30% of these fractures may have an associated ligamentous injury. For example, pain and swelling over the medial collateral ligament (MCL) with a displaced lateral plateau fracture should be strongly suspicious for an associated MCL tear.
• Meniscal injuries—Meniscal injuries are an associated finding in as many as 50% of tibial plateau fractures. The initial clinical examination is unreliable for diagnosing meniscal injuries in patients with tibial plateau fractures.
1. Initial radiographic series—The knee trauma series, the initial radiographic series, should include an anteroposterior view, a lateral view, two oblique views, and a 15° caudal tilt view. These films should be evaluated for shaft extension, articular depression, bone avulsions, and widening of the joint space. The 15° caudal view provides a more accurate assessment of joint depression than the anteroposterior view, since it accounts for the posterior slope of the tibial plateau.
2. Varus/valgus stress views—Varus/valgus stress views can be obtained as a supplement to the knee trauma series and may aid in the identification of associated ligamentous injuries. A collateral ligament disruption is suggested when the medial or lateral clear space is widened by more than 1 cm compared with that of the contralateral limb stressed in the same way.
3. Computed tomography (CT)—CT serves as an adjunct to plain radiographs in preoperative planning. The degree of articular displacement is best evaluated on a CT scan with sagittal and coronal reconstructions.
4. Magnetic resonance imaging—Magnetic resonance imaging does not yet have a clear role in the evaluation of tibial plateau fractures, although it may serve as an adjunct to plain radiographs in certain cases and it may aid in identifying associated meniscal and ligamentous injuries.
III. Classification
A. Schatzker Classification—The Schatzker classification (Fig. 10-1) is the most widely used and accepted system of classifying tibial plateau fractures.
1. Type I fractures are a split of the lateral plateau. They occur predominantly in the young patients with strong bone and may be associated with a trapped meniscus at the fracture site. There is a high risk of ligamentous injury with these fractures.
2. Type II fractures are split-depressions of the lateral plateau. An axial load caused by the femoral condyle first splits the plateau and then depresses its edge.
3. Type III fractures are pure central depressions of the lateral plateau. They are more likely the result of a low-energy injury, and they occur predominantly in older patients. There is a low risk of ligamentous injury associated with these fractures.
4. Type IV fractures involve the medial tibial plateau. They are usually high-energy injuries. There may be an associated traction lesion of the peroneal nerve.
5. Type V fractures are bicondylar (Fig. 10-2). Typically, these fractures involve a split of both the medial and the lateral plateaus without any associated articular depression.
6. Type VI fractures are characterized by the presence of an associated proximal tibial shaft fracture (i.e., metaphyseal-diaphyseal separation). They are almost always high-energy injuries with extensive comminution. There may be an associated popliteal artery disruption.
B. AO/OTA Classification (Fig. 10-3)
1. Advantages and disadvantages—The advantage of the AO/OTA classification is that it is a unified, consistent approach to the classification of fractures that appears to have good intraobserver reliability. The disadvantage is that it is a cumbersome system that is impractical to apply to the acute clinical setting. The AO/OTA classification distinguishes fractures by type, group, and subgroup.
2. Correspondence to the Schatzker classification—The AO/OTA type B fractures correspond to Schatzker Types I to IV. The AO/OTA Type C fractures correspond to Schatzker Types V and VI.
IV. Associated Injuries
A. Meniscal Tears—Meniscal tears occur in as many as 50% of tibial plateau fractures. Meniscal tears that cannot be repaired should be excised at the time of definitive surgical treatment. Peripheral meniscal tears identified at the time of open reduction should be repaired with suture just before closure.
B. Ligamentous Injuries—Associated ligamentous injuries are noted in as many as 30% of tibial plateau fractures. Treatment should be individualized according to the injury. The need for repair remains controversial since it is not entirely clear which combinations of ligament injury and fracture result in knee joint instability.
1. Collateral ligament repair—Collateral ligament repair in the acute setting requires an undesirable amount of soft tissue stripping. Evidence in the literature supports the nonoperative management of MCL injuries since most heal satisfactorily.
2. Repair of avulsions of the intercondylar eminence—Avulsions of the intercondylar eminence should be repaired, reattaching the cruciate ligament with a bone block.
V. Treatment and Treatment Rationale
A. Indications—The specific indications for operative vs. nonoperative management remain controversial.
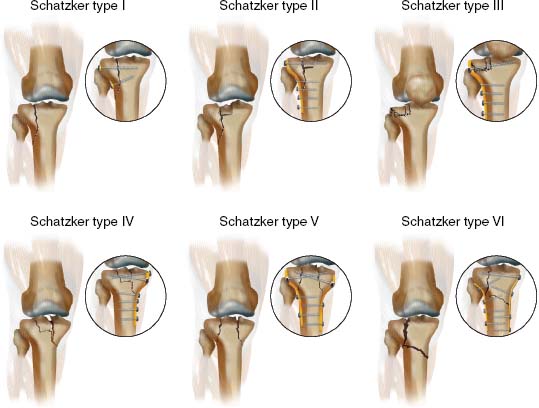
FIGURE 10-1 Schatzker classification of tibial plateau fractures. Type 1 fracture:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






