32
Tibial Plateau Combined Fractures
Tibial plateau combined fractures (Schatzker types IV, V, and VI) are generally high-energy injuries (Fig. 32-1).1, 2 They are characterized by extensive soft tissue damage, comminution, instability, and articular incongruency. Treatment goals are reconstitution of the joint surface, and correct alignment and fixation, allowing early motion. The problem has been the necessity for some type of surgical intervention, often extensive, to achieve these goals, but at the same time avoiding the complications. The ideal treatment causes no or minimal additional soft tissue insult yet at the same time achieves an articular reconstruction and limb realignment, and provides rigid fracture stability. The current techniques require minimal incisions and rely on indirect reduction, having replaced the classic extensile exposures. Fracture fixation has evolved along two different routes, the minimal invasive (percutaneous) plate osteosynthesis [MI(P) PO], and circular thin-wire frames (Ilizarov or hybrid).3, 4
Surgical Indications and Other Options
As a rule, these high-energy injuries do poorly with nonsurgical treatment. Absolute indications for open treatment of these tibial plateau fractures are those that are (1) open, (2) associated with compartment syndrome, or (3) associated with vascular compromise. Relative indications are (1) articular displacement of 2 to 3 mm, (2) greater than 10 degrees of varus/valgus instability, (3) bicondylar plateau fractures with axial displacement or any medial tilt or valgus tilt greater than 5 degrees, (4) displaced medial tibial plateau fractures, (5) joint subluxation/dislocation, and (6) fractures with metaphyseal/diaphyseal dissociation.2, 5, 6 The major contraindications for immediate open reduction and internal fixation (ORIF) are potential or present soft tissue compromise. Those fractures not within the absolute/relative indications are treated with bracing with protected weight bearing.
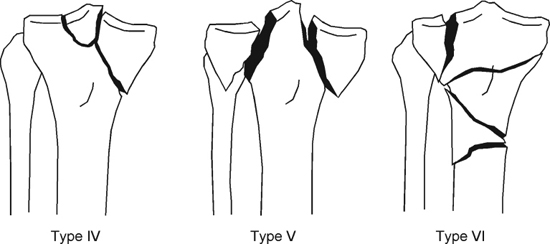
Figure 32-1 Schematic overview of the combined tibial plateau fractures: Schatzker IV, or medial condylar fracture; Schatzker V, or bicondylar fracture; Schatzker VI, or tibial plateau fracture with metaphyseal-diaphyseal dissociation.
Surgical Techniques
Patient Positioning
The patient is placed supine on a radiolucent table. We mostly use regional anesthesia and do not use postoperative epidural analgesia, because it can mask an (impending) compartment syndrome. A thigh tourniquet is applied (sterile if harvesting iliac crest bone graft). The image intensifier is utilized at right angles from the opposite side.
Initial Treatment
The treatment plan should be based on the soft tissue injury and the “personality” of the fracture. In most cases the soft tissues in Schatzker IV, V, and VI fractures are not amenable to immediate definitive fixation. Most will be temporized with a knee-spanning external fixator to allow the soft tissues to recover, or be replaced, and to address the other more life-threatening injuries. Such a spanning external fixator can be applied quickly, allowing distraction across the knee joint, restoring length, rotation, and proper alignment. Schanz half-pins (5 mm) can be placed anteromedially into the tibial shaft, and preferably laterally into the femoral shaft (anterior femoral Schanz pins are damaging to the quadriceps and cause skin and muscle irritation, often causing adhesions and restricting knee motion once removed). Place the tibial half-pins sufficiently distal so as not to contaminate future incisions.
Definitive Treatment with Internal Fixation
Medial Tibial Plateau Fracture (Schatzker Type IV)
The vast majority of these fractures are grossly unstable with associated ligamentous or vascular injuries. The medial fragment is often the “stable” fragment to which the rest of the leg has to be reduced. The incision of choice is either a medial parapatellar or a posteromedial incision.7 In the medial approach, the pes anserinus is elevated subperiosteally as a sleeve. The posteromedial incision utilizes the interval between the medial head of the gastrocnemius and the semitendinosus. The medial meniscus can be elevated off the tibial plateau by incising the meniscotibial (coronary) ligament. A small cuff is left in place for later reapproximation. PDS sutures are placed in the periphery of the meniscus to assist in closure. The fracture line often crosses the lateral joint line or crosses both the medial and lateral joint, leaving the tibial spines as separate fragments. Placement of a large femoral distractor on the medial side with one pin near the epicondylar of the distal femur and the second pin in the medial aspect of the midshaft tibia can assist in reduction using ligamentotaxis. The distal spike of the medial condylar fragment is usually most helpful in assessing the reduction. If there is an area of depression of the joint surface, a bone window can be made under the depressed area and elevated en masse using a bone tamp. This can also be accomplished by opening the fracture like a book. Bone graft morselized or block, depending on comminution, is placed under the elevated area. The tibial shaft is then reduced to the medial condylar fragment using a large reduction clamp that is placed through a stab incision on the lateral side. Once the plateau is reduced, it is temporarily fixed with one or two Kirschner wires (K-wires) (2.0 or 1.6 mm). As opposed to the lateral tibial plateau fractures, the mere placement of lag screws with washers is not sufficient stabilization for the medial side of the knee. A buttressing antiglide-type plate in addition is needed to resist the varus forces. There is no specific plate designed for the medial condyle. Most often we use the lateral tibial plateau plate designed for the contralateral side (i.e., place it backward) or a flattened semitubular or one-third tubular plate. For any associated bony ligament avulsions, peripheral meniscal tears should be repaired in the same procedure (midsubstance ligament injuries are no longer repaired or even reconstructed acutely).
Bicondylar Tibial Plateau Fracture (Schatzker Type V)
Ideally a single approach such as a lateral or medial para-patellar is used. Alternatively, a combined lateral para-patellar and posteromedial incision can be used. Reduction of the condyles to the remaining metaphyseal portion is often difficult because the metaphyseal spine can be devoid of any articular surface. In addition, there is often associated comminution of the tibial spines with the risk of narrowing the two plateaus to each other. The incision should be far enough distally to precisely key in the main lateral fragment onto the shaft. This defines the height to which the plateau should be restored. Similarly on the medial side, the reduction of the distal aspect of the medial condylar fragment to the shaft will aid in reconstructing the plateau. The use of two femoral dis-tractors (one on each side) facilitates the reduction (Fig. 32-2). Both proximal femoral distractor pins should be placed close to the epicondylar axis of the distal femur, with the two distal pins in the midshaft of the tibia. After reduction is obtained, one or two K-wires (1.6 or 2.0 mm) can be placed across the plateau to maintain temporary fixation. Definitive fixation of the lateral plateau is done using a precontoured 3.5 or 4.5 mm tibial plateau plate. The medial plateau is fixed in an antiglide fashion using a four- or five-hole one-third or semitubular plate or 3.5 mm pelvic reconstruction plate (Fig. 32-3). This can be done through the midline incision with minimal stripping or through two separate stab incisions through which the plate can be introduced and pushed and pulled into its desired position. Alternatively, in case of a compromised medial soft tissue sleeve, a two half-pin single-bar medial external fixator can be placed instead of a plate to buttress and prevent varus collapse, and be removed in the outpatient clinic setting 6 to 8 weeks later after healing is obtained. The recently introduced locked compression plates (LCPs) and less invasive stabilization system (LISS) (Synthes, Paoli, PA) (Fig. 32-4) with their fixed angle screws can substitute for dual fixation if adequate reduction is obtained from the opposite side and provided there is no significant comminution that extends proximally along the medial column.3, 8, 9
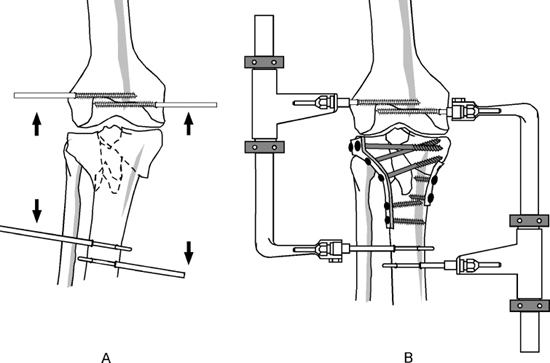
Figure 32-2 Using two femoral distractors simultaneously for ligamentotaxis in bicondylar fractures helps the reduction.
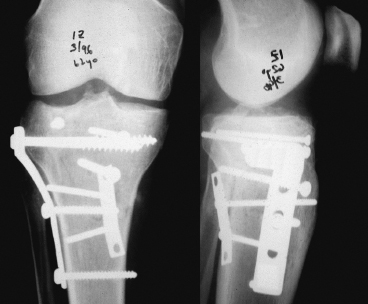
Figure 32-3 Schatzker V fracture with a large posteromedial fragment treated with a lateral plate through a lateral parapatellar incision with a contralateral posteromedial incision for a one-third tubular antiglide plate.
Bicondylar Tibial Plateau Fracture with Metaphyseal-Diaphyseal Dissociation (Schatzker Type VI)
These are the most difficult tibial plateau/tibial shaft fractures to treat. Not only is the bony reconstruction complex, but the soft tissue damage is often severe. With the tibial shaft dissociated from the metaphysis, there is no base on which to reconstitute the condyles. In addition, there is often a displaced anterior proximal fragment that involves the tibial tubercle and that needs stabilization (anterior to posterior lag screw) to avoid displacement via the tensile forces of the quadriceps/patellar tendon. The use of femoral distractors often does not help, as they merely cause distraction at the metaphyseal-diaphyseal fracture site. After reduction of the plateau with K-wires, multiple subchondral lag screws can be placed across (to prevent plateau narrowing when doing comminution, the use of fully threaded screws might occasionally be necessary). The use of 4.5 or even 3.5 mm cortical screws seems to work as well as the larger cannulated 6.5 and 7.3 mm screws. The medial fixation needed to prevent varus malalignment can be similar to that used for the bicondylar fracture (one-third or semitubular or 3.5 mm pelvic reconstruction or even a LCP buttress plate, all placed through a small medial or posteromedial incision) (Fig. 32-5A). Alternatively, again a two half-pin external fixator can be medially placed (Fig. 32-5B). The lateral fixation calls for a longer and sturdier device extending down the shaft such as a LCDCP, LCP, or even LISS plate.3, 8, 9 Current trends are to place these plates through a small stab incision into a subcutaneous tunnel with subsequent percutaneous screw fixation. In addition, the promising results of the LISS plate with unicortical fixed-angle screws might obviate the need for supplementary fixation on the opposite side of the bone (Fig. 32-5C).
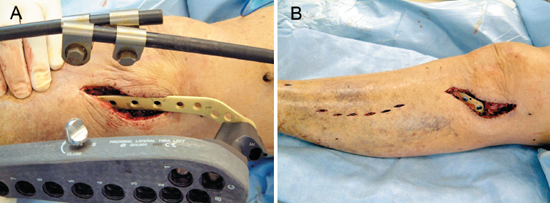
Figure 32-4 Application of a tibial less invasive stabilization system (LISS) plate after temporary spanning external fixation. (A) The LISS plate is inserted on its guide into the subcutaneous tunnel. (B) Final position of the plate after percutaneous screw fixation distally.
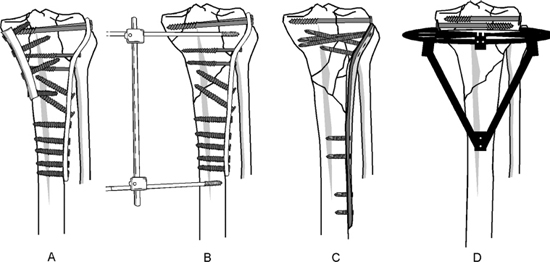
Figure 32-5 Methods of fixation for Schatzker V and VI tibial plateau fractures. (A) Standard lateral plating with a contralateral antiglide plate on the (postero) medial side. (B) If soft tissue compromise on the medial side precludes an incision, a simple two-pin external fixator can be placed to prevent varus collapse. (C) The LISS relies on closed, indirect reduction, minimally invasive plate insertion, and minimal bone contact. It serves as an internal fixator with unicortical percutaneously inserted fixed-angle screws. The articular surface is initially reduced with lag screws. In most cases, no additional medial fixation is needed. (D) Hybrid external fixation with additional lag screw fixation.
Definitive External Fixation
External fixation can be used as definitive treatment for complex tibial plateau fractures.2, 4 This can be dictated by the soft tissue envelope, that is, one that will be unlikely to allow (even limited) ORIF even after a delay, or by surgeon preference. Different frames are amenable for use as definitive fixation, including half-pin uni- and multiplanar frames, thin-wire ring fixators, and so-called hybrid fixators. Each frame configuration has advantages and disadvantages, and much is determined by individual surgeon preference. Ilizarov frames provide better rigidity than hybrid frames, but they are much more complex and bulky, and there is a steep learning curve. These are also not without problems, such as pin tract infection with the risk of septic arthritis.
Thin-wire fixation with a hybrid-type fixator is our preference in these circumstances (Fig. 32-5D). Fluoroscopy-assisted closed reduction is first attempted, resorting to minimal arthrotomy and open reduction only if necessary. Temporary fixation of the articular surface is maintained with K-wires. Lag screw fixation is then achieved with cannulated partially threaded screws of all sizes, depending on the fragment. A smooth thin wire is placed just distal (at least 15 mm) and parallel to the joint line in the coronal plane. A second wire, with an olive or bead, is then placed posterolateral to anteromedial. There is a low incidence of communication of the proximal tibiofibular joint with the knee joint; hence we prefer to place this second wire just anterior to the fibula, and have it exit medially as close to the patellar tendon as possible without violating it or the pes tendons. The third and last (beaded) wire is placed posteromedial to anterolateral. A ring is then fixed to the wires, leaving a distance of approximately two fingerbreadths between the ring and the skin. The ring should allow as much knee flexion as possible before impinging on the posterior thigh. The wires are then tensioned (smooth them first). Additional proximal anterior 5 mm Schanz half pins can be added to the ring. Two or three 4.5 or 5.0 mm half-pins are placed bicortically into the anteromedial distal third of the tibia. Using bars and clamps the proximal ring is connected to the distal half-pins, reconstituting the metaphyseal-diaphyseal disruption of the tibia.
Tips and Tricks
By prepping and draping the entire involved extremity, including the iliac crest, and then utilizing a sterile tourniquet, limb mobilization and evaluation of alignment is easier. By centering the electrocautery cord over the femoral head and over the center of the ankle joint (using C-arm imaging), the mechanical axis can be determined and adjusted easily.
Preoperative traction radiographs better identify the fracture fragments and what can be achieved with “ligamentotaxis.” Contralateral radiographs are useful templates for reduction.
External fixator pins of the spanning temporary fixator should be positioned far away from anticipated futures incisions. Similarly, incisions for compartment releases should be done keeping future reconstructive efforts in mind (i.e., use more anterior tibial incision that can be incorporated later into the anterolateral approach, if indicated).
Flexing the knee (by dropping the leg over the side of the fluorotable) relaxes the iliotibial band and greatly enhances visualization, also by using a varus or valgus force.
In fractures involving both tibial condyles, start with the reduction of the simpler or less comminuted condyle.
The use of smaller (3.5 and 4.5 mm) cortical screws allows for a higher number of screws that can be placed, also with more directional versatility, in supporting the tibial plateau after elevating and bone grafting a depressed segment.
Pitfalls and How to Avoid Them
Infection and wound healing problems are common and often disastrous complications in the surgical treatment of these fractures. ORIF should be delayed until the swelling has fully resolved and any fracture blisters have ruptured and dried. Skin wrinkles are a good indicator that acute swelling (edema) is sufficiently decreased. Incisions through fracture blisters should be avoided. Limited incisions, full-thickness flaps, careful subperiosteal dissection, and meticulous skin closure are additional keys to uneventful healing.
When soft tissue or skin compromise is present or impending, plastic surgical consultations for rotational or free flap coverage should be considered early. Wound breakdown or infection warrants repeat irrigation and debridement until a clean granulating wound bed is obtained.
Nonunions are very uncommon for the Schatzker IV fractures. They do occur, however, in Schatzker V and VI injuries, especially at the metaphyseal-diaphyseal junction. Once diagnosed, nonunion should be treated with early bone grafting and possible revision ORIF.
Malunion can be seen early or late. If seen early, it usually represents failure of reduction or fixation and warrants early intervention with revision ORIF and bone grafting, especially in young patients. The fracture lines are usually still easily identified. If seen late, it most likely represents loss of fixation or collapse of the bony structure around the hardware. This is much more difficult to manage. If there is an articular malunion of one plateau with collapse, an intraarticular (opening wedge) osteotomy can be considered. This necessitates careful preoperative planning and expertise. For extraarticular malalignment with mechanical axis deviation, open-wedge metaphyseal osteotomy may restore length and alignment.
Lateral or medial hardware friction or prominence often leads to pain. Use of lower profile and smaller plates may reduce the need for hardware removal in the future.
Knee stiffness or arthrofibrosis is often the result of suboptimal rehabilitation. If at 4 weeks the patient cannot flex beyond 90 degrees or fully extend, we advise a gentle manipulation under anesthesia, if necessary with an epidural analgesia catheter placement for postoperative continuous passive motion (CPM). Additionally, an arthroscopic knee adhesiolysis can be done.
Posttraumatic arthrosis is a combination of the often-considerable damage to the articular cartilage sustained at the time of impact and a less than perfect reduction or stabilization. It is important to preserve the meniscus at all costs, as this helps prevent excessive load bearing on the (already damaged) underlying plateau. Any residual knee joint instability because of malalignment or ligamentous injury should be addressed early to prevent further deterioration.
Conclusion
Treatment of complex tibial plateau fractures and their associated soft tissue injuries is notoriously difficult and fraught with potentially disastrous complications. However, with new developments in minimal exposure, indirect reduction, and “biologic” fixation techniques, it is expected that their outcomes will continue to improve.
References
1 Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968-1975. Clin Orthop Rel Res 1979;138:94–104
2 Virkus WW, Helfet DL. Tibial plateau fractures. In: Insall JN, Scott NS ed. Surgery of the Knee. New York: Churchill-Livingstone; 2001: 1265–1289
3 Krettek C, Gerich T, Miclau T. A minimally invasive medial approach for proximal tibial fractures. Injury 2001;32 (suppl 1): SA4–13
4 Watson TJ, Ripple S, Hoshaw SJ, Fyhrie D. Hybrid external fixation for tibial plateau fractures. Orthop Clin North Am 2002;33:199–209
5 Tscherne H, Lobenhoffer P. Tibial plateau fractures. Management and expected results. Clin Orthop Relat Res 1993;292:87–100
6 Koval KJ, Helfet DL. Tibial plateau fractures: evaluation and treatment. J Am Acad Orthop Surg 1995;3:86–94
7 Georgiadis GM. Combined anterior and posterior approaches for complex tibial plateau fractures. J Bone Joint Surg Br 1994;76:285–289
8 Stannard JP, Wilson TC, Volgas DA, Alonso JE. Fracture stabilization of proximal tibial fractures with the proximal tibial LISS: early experience in Birmingham, Alabama (USA). Injury 2003;34 (suppl 1): A36–A42
9 Cole PA, Zlowodzki M, Kregor PJ. Less invasive stabilization system (LISS) for fractures of the proximal tibia: indications, surgical technique and preliminary results of the UMC clinical trial. Injury 2003;34 (suppl 1): A16–A29
< div class='tao-gold-member'>









