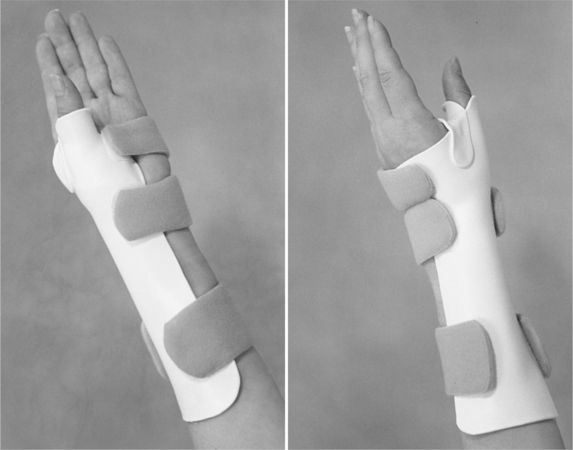
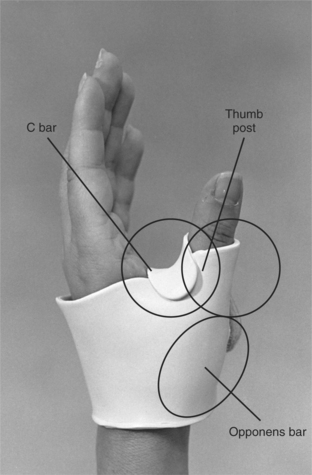
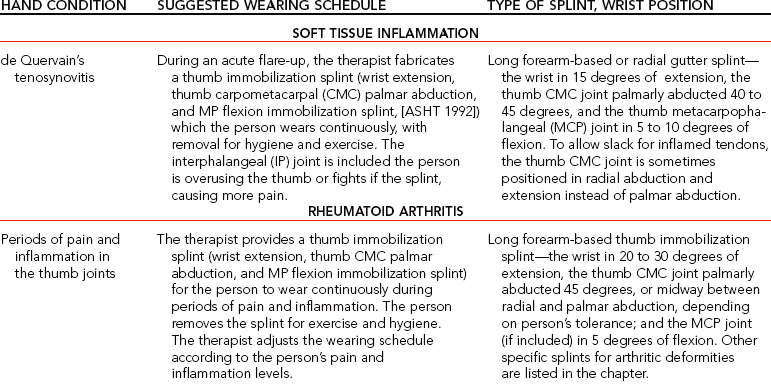
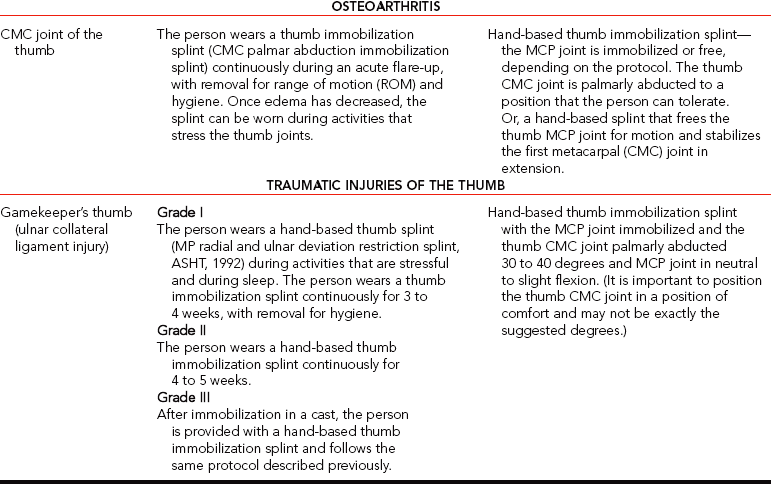
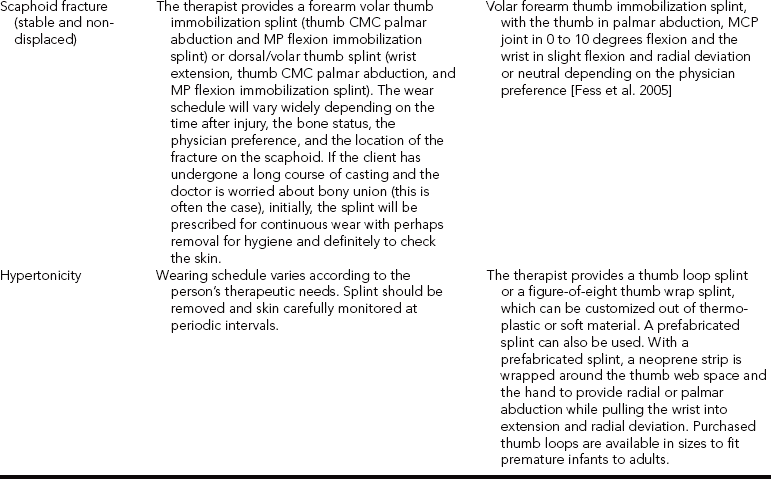
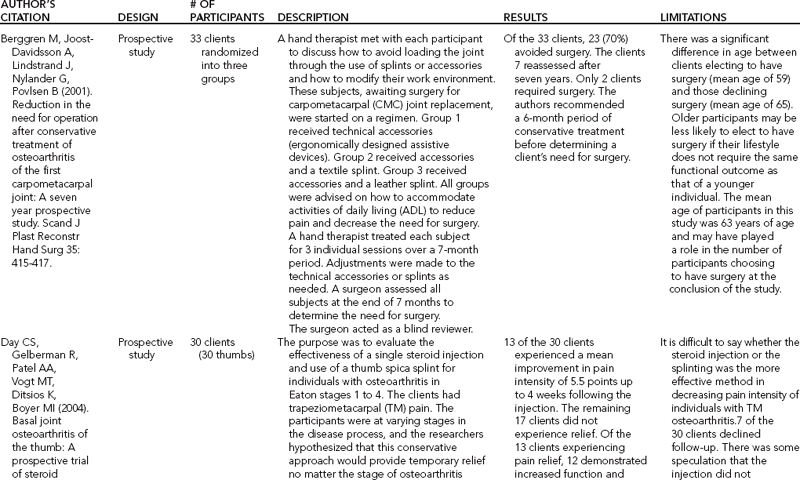
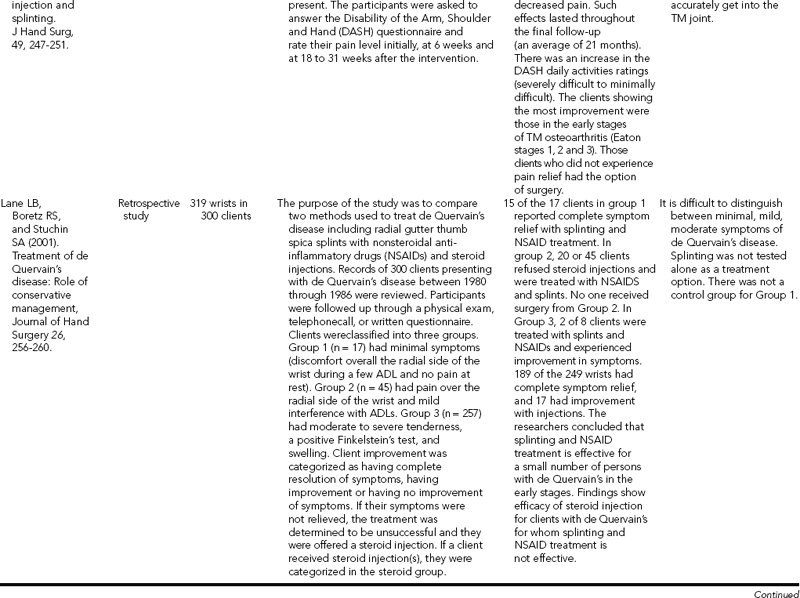
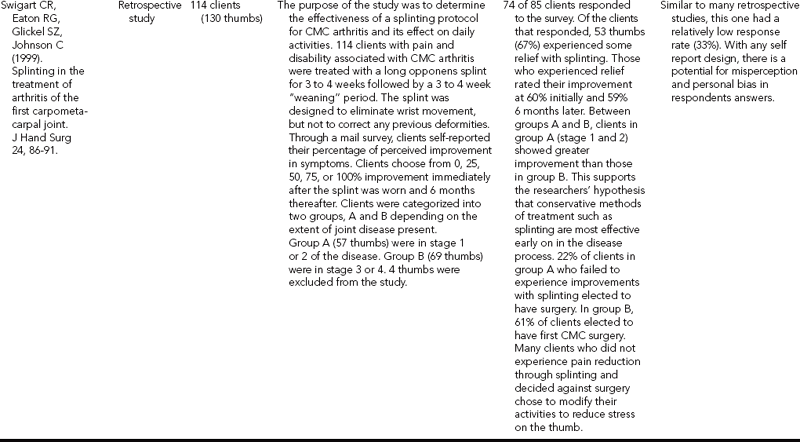
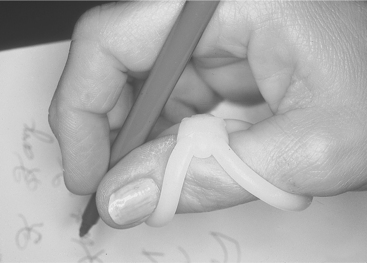
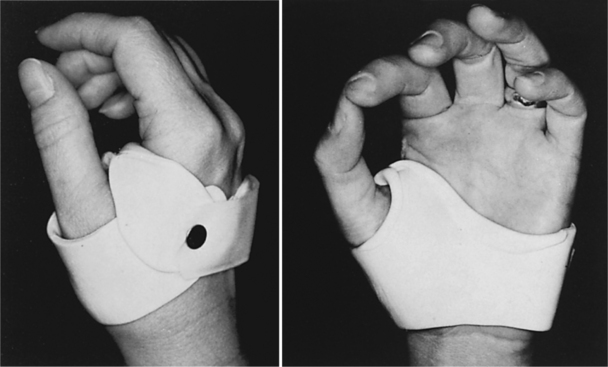
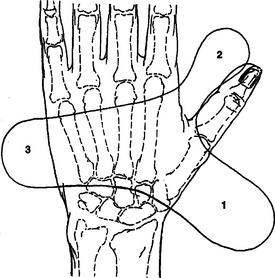
CHAPTER 8 1 Discuss important functional and anatomic considerations for splinting the thumb. 2 List appropriate thumb and wrist positions in a thumb immobilization splint. 3 Identify the three components of a thumb immobilization splint. 4 Describe the reasons for supporting the joints of the thumb. 5 Discuss the diagnostic indications for a thumb immobilization splint. 6 Discuss the process of pattern making and splint fabrication for a thumb immobilization splint. 7 Describe elements of a proper fit of a thumb immobilization splint. 8 List general and specific precautions for a thumb immobilization splint. 9 Use clinical reasoning to evaluate fit problems of a thumb immobilization splint. 10 Use clinical reasoning to evaluate a fabricated thumb immobilization splint. 11 Apply knowledge about thumb immobilization splinting to a case study. 12 Understand the importance of evidenced-based practice with thumb immobilization splint provision. 13 Describe the appropriate use of prefabricated thumb splints. A commonly prescribed splint in clinical practice is the thumb palmar abduction immobilization splint [American Society of Hand Therapists 1992]. Other names for this splint are the thumb spica splint, the short or long opponens splint [Tenney and Lisak 1986], and the thumb gauntlet splint. The purpose of this splint is to immobilize, protect, rest, and position one or all of the thumb carpometacarpal (CMC), metacarpophalangeal (MCP), and interphalangeal (IP) joints while allowing the other digits to be free. Thumb immobilization splints can be divided into two broad categories: (1) forearm based and (2) hand based. Forearm-based thumb splints stabilize the wrist as well as the thumb. Stabilizing the wrist is beneficial for a painful wrist as the splint provides support. The hand-based immobilization splints provide stabilization for the thumb while allowing for wrist mobility. Forearm-based or hand-based thumb immobilization splints are often used to help manage different conditions that affect the thumb’s CMC, MP, or IP joints. For people who have de Quervain’s tenosynovitis a forearm-based thumb splint provides rest, support, and protection of the tendons that course along the radial side of the wrist into the thumb joints. The therapist also applies a forearm-based thumb immobilization splint to splint postoperatively for control of motion in persons with rheumatoid arthritis after a joint arthrodesis or replacement. With the resulting muscle imbalance from a median nerve injury, the therapist may apply a hand-based thumb immobilization splint to keep the thumb web space adequately open. (Refer to Chapter 13 for more information on nerve injury). In addition, the thumb immobilization splint can position the thumb before surgery [Geisser 1984]. The splint provides support and positioning after traumatic thumb injuries, such as sprains, joint dislocations, ligament injuries, and scaphoid fractures. Frequently a hand-based thumb immobilization splint is applied to persons with gamekeeper’s thumb, which involves the ulnar collateral ligament of the thumb MCP joint. For hypertonicity a thumb splint sometimes called a figure-of-eight thumb wrap or thumb loop splint facilitates hand use by decreasing the palm-in-thumb posture or palmar adduction that is often associated with this condition. Therefore, because this splint is so commonly prescribed it is important that therapists become familiar with its application and fabrication. The thumb is essential for hand functions because of its overall importance to grip, pinch, and fine manipulation. The thumb’s exceptional mobility results from the unique shape of its saddle joint, the arrangement of its ligaments, and its intrinsic musculature [Belkin and English 1996, Tubiana et al. 1996, Colditz 2002]. The thumb provides stability for grip, pinch, and mobility because it opposes the fingers for fine manipulations [Wilton 1997]. Sensory input to the tip of the thumb is important for functional grasp and pinch. A thorough understanding of the anatomy and functional movements of the thumb is necessary before the therapist attempts to splint the thumb. The therapist must understand that the most crucial aspect of the thumb immobilization splint design is the position of the CMC joint [Wilton 1997]. Positioning of the thumb in a thumb post allows for palmar abduction and some opposition, which are critical motions for functional prehension. See Chapter 4 for a review of the anatomy and functional movements of the thumb. The thumb immobilization splint prevents motion of one, two, or all of the thumb joints [Fess et al. 2005]. The splint has numerous design variations. It can be a volar (Figure 8-1), dorsal (Figure 8-2), or radial gutter (Figure 8-3). The splint may be hand based or wrist based, depending on the person’s diagnosis, the anatomic structures involved, and the associated pain at the wrist. If the wrist is included, the wrist position will vary according to the diagnosis. For example, with de Quervain’s tenosynovitis the wrist is commonly positioned in 15 degrees of extension to take the pressure off the tendons. The splint components fabricated in the final product will vary according to the thumb joints that are included. The final splint product will be formed based on the therapeutic goals for the client. The therapist should have a good understanding of the purpose and the fabrication process for the various splinting components. Central to most thumb immobilization splints are the opponens bar, C bar, and thumb post (Figure 8-4) [Fess et al. 2005]. The opponens bar and C bar position the thumb, usually in some degree of palmar abduction. The thumb post, which is an extension of the C bar, immobilizes the MP only or both the MP and IP joints. The position of the thumb in a splint varies from palmar abduction to radial abduction, depending on the person’s diagnosis. With some conditions, such as arthritis, the therapist can assist prehension by stabilizing the thumb CMC joint in palmar abduction and opposition. Certain diagnostic protocols—such as those for extensor pollicis longus (EPL) repairs, tendon transfers for thumb extension, and extensor tenolysis of the thumb—require the thumb to have an extension and a radial abducted position [Cannon et al. 1985]. The thumb immobilization splint may do one of the following: (1) stabilize only the CMC joint; (2) include the CMC and MP joints; or (3) encompass the CMC, MCP, and IP joints. The physician’s order may specify which thumb joints to immobilize in the splint. In some situations, the therapist may be responsible for determining which joints the splint should stabilize. The therapist uses diagnostic protocols and an assessment of the person’s pain to make this decision. If the therapist deems it necessary to limit thumb motion and to protect the thumb, the IP may be immobilized. Certain diagnostic protocols (such as those for thumb replantations, tendon transfers, and tendon repairs) often require the inclusion of the IP joint in the splint [Tenney and Lisak 1986]. Overall the therapist should fabricate a splint that is the most supportive and least restrictive in movement. Treatment of many of these conditions may require the expertise of experienced hand therapists. In general clinical practice, therapists commonly treat persons who have de Quervain’s tenosynovitis, rheumatoid arthritis, osteoarthritis, fractures, and ligament injuries. (Table 8-1 contains guidelines for these hand conditions.) The novice therapist should keep in mind that physicians and experienced therapists may have their own guidelines for positioning and splint-wearing schedules. The therapist should also be aware that thumb palmar abduction may be uncomfortable for some persons. Therefore, the thumb may be positioned midway between radial and palmar abduction. De Quervain’s tenosynovitis, which results from repetitive thumb motions and wrist ulnar deviation, is a form of tenosynovitis affecting the abductor pollicis longus (APL) and the extensor pollicis brevis (EPB) in the first dorsal compartment. Those persons whose occupations involve repetitive wrist deviation and thumb motions (such as the home construction tasks of painting, scraping, wall papering, and hammering) are prone to this condition [Idler 1997]. De Quervain’s tenosynovitis is the most commonly diagnosed wrist tendonitis in athletes [Rettig 2001], such as with golfers [McCarroll 2001]. It may be recognized by pain over the radial styloid, edema in the first dorsal compartment, and positive results from the Finkelstein’s test. During the acute phase of this condition, conservative therapeutic management involves immobilization of the thumb and wrist for symptom control [Lee et al. 2002]. This splint is classified by the American Society of Hand Therapists (ASHT) as a wrist extension, thumb CMC palmar abduction and MP flexion immobilization splint [ASHT 1992]. It may cover the volar or dorsal forearm or the radial aspect of the forearm and hand. The therapist positions the wrist in 15 degrees of extension, neutral wrist deviation, 40 to 45 degrees of palmar abduction of the thumb CMC joint, and 5 to 10 degrees of flexion in the MCP joint [Idler 1997]. Usually the therapist allows the IP joint to be free for functional activities and includes the joint in the splint if the person is overusing the thumb or fights the splint, causing even more pain. The splint is worn continuously, with removal for hygiene and exercise within a pain-free range [Lee et al. 2002]. A prefabricated splint is recommend after the person’s pain subsides [Lee et al. 2002] for work and sports activities [Fess et al. 2005], or if the person does not want to wear a custom splint [Biese 2002]. Post-surgical management of de Quervain’s tenosynovitis also involves splinting, usually for 7 to 10 days [Rettig 2001]. Few studies have considered the efficacy of thumb splinting for de Quervain’s tenosynovitis and results have been variable (seeTable 8-2). Lane et al. [2001] studied 300 subjects and compared splinting with oral nonsteroidal anti-inflammatory drugs (NSAIDs) and steroid injections over a 2- to 4-week time period. Subjects were splinted in a custom thumb immobilization splint with the wrist in neutral and the thumb in 30 degrees between palmar and radial abduction. Subjects were placed in three groups based on symptoms (minimal, mild, moderate/severe). Those subjects who had mild symptoms responded well to splinting with NSAIDs. Limitations of this study included no control group for the mild symptom group, small numbers in the mild group, the subjective nature of classifying subjects, and no mention of a splint-wearing schedule. Weiss et al. [1994] (n = 93) compared splinting to steroid injection or combined in treatment with steroid injections. They did not find strong benefits for thumb splinting. Witt et al. [1991] (n = 95) also studied the provision of a long thumb immobilization splint including the wrist (which was worn continuously for 3 weeks, along with steroid injection) and had a good success rate. Avci et al. [2002] focused their research on conservative treatment of 19 pregnant women with de Quervain’s tenosynovitis. One group received cortisone injections and the other group received thumb splints. The group receiving cortisone injections had complete pain relief compared to partial relief from the splint-wearing group. The splint-wearing group experienced pain relief only when wearing the splint. Finally, the researchers pointed out that pregnancy-related de Quervain’s disease is self-limiting (with cessation of symptoms after breast feeding is terminated). Much more research needs to be completed to truly determine the efficacy of thumb splinting with de Quervain’s tenosynovitis. It is helpful for therapists to review these studies because these also provide information about the effectiveness of physician treatments, such as steroid injections, their clients are receiving. Rheumatoid arthritis often affects the thumb joints, particularly the MCP and CMC joints. Splinting for rheumatoid arthritis can reduce pain, slow deformity, and stabilize the thumb joints [Ouellette 1991]. The disease includes three stages, each of which has a different splinting approach, even though the therapist may apply the same thumb immobilization splint. Common thumb deformities from the arthritic process are boutonnière’s deformity (type I, MP joint flexion and IP joint extension) and swan neck deformity (type 3, MP extension or hyperextension and IP flexion) [Nalebuff 1968, Colditz 2002]. During the beginning stages of boutonnière’s deformity a circumferential neoprene splint is applied to support the MCP joint with the IP joint free to move [Colditz 2002]. To address progression of MCP joint deformity, Colditz [2002] suggested a carefully fabricated thermoplastic splint to stabilize the joint to eliminate volar subluxation and to allow for CMC motion (Figure 8-5). For early stages of swan neck deformity, a small custom-fitted dorsal thermoplastic splint over the MCP joint prevents MCP hyperextension [Colditz 2002]. Later dorsal and radial subluxation at the CMC joint causes CMC joint adduction, MCP hyperextension, and IP flexion [Colditz 2002]. For this deformity, Colditz [2002] suggested fabricating a hand-based thumb immobilization splint that blocks MCP hyperextension (Figure 8-6). With rheumatoid arthritis, laxity of the ulnar collateral ligament at the IP and MCP joint can also develop.Figure 8-7 shows a functional splint, which can also be used with rheumatoid arthritis or osteoarthritis for lateral instability of the thumb IP joint. One approach to splinting a hand with arthritis is to immobilize the thumb in a forearm-based, thumb immobilization splint with the wrist in 20 to 30 degrees of extension, the CMC joint in 45 degrees of palmar abduction (if tolerated), and the MCP joint in 0 to 5 degrees of flexion [Tenney and Lisak 1986]. This splint is classified by ASHT as a wrist extension, thumb CMC palmar abduction and MP extension immobilization splint [ASHT 1992]. Resting the hand in this position is extremely beneficial during periods of inflammation, or if the thumb is unstable at the CMC joint [Marx 1992]. Incorporating the wrist in a forearm-based thumb splint is appropriate when the client’s wrist is painful or if there is also arthritis involvement. Some persons with rheumatoid arthritis affecting the CMC joint benefit from a hand-based thumb immobilization splint (thumb CMC palmar abduction immobilization splint) [ASHT 1992], as shown inFigure 8-8 [Melvin 1989, Colditz 1990]. Positioning the thumb in enough palmar abduction for functional activities is important. With a hand-based thumb immobilization splint, if the IP joint is painful and inflamed the therapist should incorporate the IP joint into the splint. However, putting any material (especially plastic) over the thumb pad will virtually eliminate thumb and hand function. The person wears this splint constantly for a minimum of 2 to 3 weeks, with removal for hygiene and exercise. The therapist adjusts the wearing schedule according to the person’s pain and inflammation levels. Figure 8-8 A hand-based thumb immobilization splint (thumb CMC palmar abduction immobilization splint). On the other hand, some therapists stabilize the thumb CMC joint alone with a short splint that is properly molded and positioned (Figures 8-9 and 8-10). This splint works effectively on people who have CMC joint subluxation resulting in adduction of the first MP joint and anyone with CMC arthritis who can tolerate wearing a rigid splint. This splint can be also used for CMC osteoarthritis, discussed in more detail later in this chapter [Colditz 2000, 2002]. Often when a physician refers a person who has rheumatoid arthritis for splinting, deformities have already developed. If the therapist attempts to place the person’s joints in the ideal position of 40 to 45 degrees of palmar abduction, excessive stress on the joints may result. The therapist should always splint a hand affected by arthritis in a position of comfort [Colditz 1984]. When fabricating a splint on a person who has rheumatoid arthritis, the therapist should be aware that the person may have fragile skin. The therapist should monitor all areas that can cause skin breakdown, including the ulnar head, Lister’s tubercle, the radial styloid along the radial border, the CMC joint of the thumb, and the scaphoid and pisiform bones on the volar surface of the wrist [Dell and Dell 1996]. Padding the splint for comfort to prevent skin irritation may be necessary. The selected splinting material should be easily adjustable to accommodate changes in swelling and repositioning as the disease progresses. Asking persons about their swelling patterns is important because splints fabricated during the day should allow enough room for nocturnal swelling. Thermoplastic material less than CMC joint osteoarthritis is a common thumb condition, especially among women over 40 [Zelouf and Posner 1995, Melvin 1989]. Pain from osteoarthritis at the base of the thumb interferes with the person’s ability to engage in normal functional activities as the CMC joint is the most critical joint of the thumb for function [Chaisson and McAlindon 1997, Neumann and Bielefeld 2003]. Precipitating factors include hypermobility, repetitive grasping, pinching, use of vibratory tools, and a family history of the condition [Winzeler and Rosenstein 1996, Melvin 1989]. Over time, the dorsal aspect of the CMC joint is stressed by repetitive pinching and the strong muscle pull of the adductor pollicis muscle and the short intrinsic thumb muscles. Altogether, these forces may cause the first CMC joint to sublux dorsally and radially. This typically results in the first metacarpal losing extension and becoming adducted. The MCP joint hyperextends to accommodate grasp [personal communication, J. C. Colditz, April 1995; Melvin 1989; personal communication, K. Schultz-Johnson, June 2006]. Splinting for CMC joint arthritis helps to manage pain, provides stability for intrinsic weakness of the capsular structures, and preserves the first web space. In addition, splinting helps with inflammation control, joint protection, and maintaining function [Poole and Pellegrini 2000, Neumann and Bielefeld 2003]. Static splinting is recommended for hypermobile or unstable joints but not for fixed joints [Neumann and Bielefeld 2003]. There are many options for splint design, ranging from forearm splints (with the CMC and MCP joints included) to hand-based splints (with the CMC and MCP joints included, or only the CMC joint included). With any selected design, the thumb is generally positioned in palmar abduction [Neumann and Bielefeld 2003]. Based on cadaver research, people with a hypermobile MCP joint who are positioned with the thumb in 30 degrees of flexion experience reduced pressure on the palmar part of the trapeziometacarpal joint, an area prone to deterioration [Moulton et al. 2001]. Melvin [1989] suggested fabricating a hand-based thumb immobilization splint (thumb CMC palmar abduction immobilization splint,Figure 8-8) [ASHT 1992], with the primary therapeutic goal of restricting the mobility of thumb joints to decrease pain and inflammation. The splint stabilizes the CMC and MCP joints in the maximal amount of palmar abduction that is comfortable for the person and allows for a functional pinch. Splinting both joints in a thumb post stabilizes the CMC joint in abduction so that the base of the MCP is stabilized. With the splint on, the person should continue to perform complete functional tasks, such as writing, comfortably. This thumb immobilization splint may be fabricated from a thin (1/16-inch) conforming thermoplastic material. As discussed, another splinting option for CMC osteoarthritis designed by Colditz [2000] is a hand-based splint that allows for free motion of the thumb MCP joint and stabilizes the CMC joint to manage pain (Figures 8-9 and 8-10). The wrist is not included in the splint’s design to allow for functional wrist motions. Colditz suggested an initial full-time wear of 2 to 3 weeks with removal for hygiene. Afterward, the splint should be worn during painful functional activities [Colditz 2000]. Therapists should fabricate this splint only on hands that have “a healthy MP joint” because the MP joint may sustain additional flexion pressure due to the controlled flexion position of the CMC joint [Melvin 2002, p. 1652]. Therapists must be attentive to wear on the MP joint [Neuman and Bielefeld 2003]. Prefabricated splints can also be considered for CMC osteoarthritis. However, prefabricated splints should be used with caution because positioning the thumb in abduction within the splint can increase MP joint extension, which can worsen a possible deformity [Biese 2002]. Given the variety of splinting options available, therapists critically analyze which splint to provide (forearm based or hand based) and which thumb joints to immobilize. Critical thinking considerations include presence of pain, need for stability, work, and functional demands. Researchers offer some guidance. Weiss et al. [2000] compared providing a long thumb immobilization splint with the MCP joint included to a hand-based splint with only the CMC joint included. In this 2-week study (n = 26), both splints were applied to individuals in grades 1 through 4 of CMC osteoarthritis as rated by Eaton and Littler [1973]. Both splints were found to be effective for pain control with all grades of the disease. However, the splints were only effective in reducing subluxation of the CMC joint for subjects in the earlier stages (grades 1 and 2) of the disease. Subjects in the later stages of the disease (grades 3 and 4) preferred the short splint and reported pain relief with splint wear. Subjects in grades 1 and 2 slightly preferred the long splint (56%). Neither splint increased pinch strength nor changed pain levels when completing pinch strength measurements. Activities of daily living (ADL) improved with the short splint (93%) compared to (44%) with the long splint. Subjects reported that ADL were more difficult to complete with the long splint [Weiss et al. 2000]. Swigart et al. [1999] retrospectively researched (n = 114) the application of a custom long thumb immobilization splint with CMC osteoarthritis and found it to be a beneficial conservative treatment. Overall, subjects (regardless of disease stage) benefited from splinting (with a “60% improvement rate after splinting and 59% 6 months later” [Swigart et al. 1999, p. 90]). Some subjects were not able to tolerate the long splint because it felt too confining and uncomfortable. Day et al. [2004] studied splinting and steroid injections for people with thumb osteoarthritis and found that people in the earlier stages of the disease showed good improvement with conservative measures.
Thumb Immobilization Splints
Functional and Anatomic Considerations for Splinting the Thumb
Features of the Thumb Immobilization Splint
Diagnostic Indications
Splinting for de Quervain’s Tenosynovitis
Splinting for Rheumatoid Arthritis and Osteoarthritis

 -inch thick is best for small hand splints. Splints fabricated from heavier splinting material have the potential to irritate other joints [Melvin 1989]. Therapists must carefully evaluate all hand splints for potential stress on other joints and should instruct persons to wear the splints at night, periodically during the day, and during stressful daily activities. However, therapists should always tailor any splint-wearing regimen for each person’s therapeutic needs.
-inch thick is best for small hand splints. Splints fabricated from heavier splinting material have the potential to irritate other joints [Melvin 1989]. Therapists must carefully evaluate all hand splints for potential stress on other joints and should instruct persons to wear the splints at night, periodically during the day, and during stressful daily activities. However, therapists should always tailor any splint-wearing regimen for each person’s therapeutic needs.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine